62 Pulmonary Embolism
Venous thromboembolism (VTE), deep venous thrombosis (DVT), pulmonary embolism (PE), or all three can complicate the course of sick hospitalized patients but may also affect ambulant and otherwise apparently healthy individuals.1–3 Pulmonary embolism remains the most common preventable cause of hospital death and is responsible for approximately 150,000 to 200,000 deaths per year in the United States. Most patients who die from PE succumb suddenly or within 2 hours of the acute event before therapy can be initiated or can take effect.4 Effective prophylaxis against VTE is now available for most high-risk patients.5,6 Prophylaxis is more effective in preventing death and morbidity from VTE than is treatment of the established disease.
 Pathophysiology
Pathophysiology
Acquired and inherited risk factors for VTE have been identified and are shown in Table 62-1. The risk of VTE increases when more than one predisposing factor is present.7,8
TABLE 62-1 Factors Predisposing to Development of Venous Thromboembolism
| Clinical Risk Factors |
| Inherited or Acquired Abnormalities |
Activated protein C resistance is the most common hereditary abnormality predisposing to VTE. The defect results from substitution of glutamine for arginine at residue 506 in the factor V molecule, making factor V resistant to proteolysis by activated protein C. The gene mutation is commonly designated factor V Leiden and follows autosomal dominant inheritance. Patients who are homozygous for the factor V Leiden mutation have a markedly increased risk of thromboembolism and present with clinical thromboembolism at a younger age (median 31 years) than those who are heterozygous (median age 46 years).7,9 Factor V Leiden is present in approximately 5% of the normal Caucasian population, 16% of patients with a first episode of DVT, and up to 35% of patients with idiopathic DVT.7,9,10
Prothrombin G20210A is another gene mutation that predisposes to VTE. It is present in approximately 2% to 3% of apparently healthy individuals and in 7% of those with DVT.9 An inherited abnormality cannot be detected in up to 40% to 60% of patients with idiopathic DVT, suggesting that other gene mutations are present and have an etiologic role.
Pulmonary embolism originates from thrombi in the deep veins of the leg in 90% or more of patients.11–13 Other less common sources of PE include the deep pelvic veins, renal veins, inferior vena cava, right ventricle, and axillary veins. Most clinically important PE arise from thrombi in the popliteal or more proximal deep veins of the leg. Pulmonary embolism occurs in 50% of patients with objectively documented proximal vein thrombosis; many of these emboli are asymptomatic.11 Usually only part of the thrombus embolizes, and 50% to 70% of patients with angiographically documented PE have detectable DVT of the legs at the time of presentation.12 The clinical significance of PE depends on the size of the embolus and the cardiorespiratory reserve of the patient.
 Clinical Features
Clinical Features
The clinical features of DVT include leg pain, tenderness and swelling, a palpable cord, discoloration, venous distention, prominence of the superficial veins, and cyanosis. The clinical diagnosis of DVT is highly nonspecific because none of the symptoms or signs is unique, and each may be caused by nonthrombotic disorders. Patients with relatively minor symptoms and signs may have extensive DVT, whereas those with florid leg pain and swelling, suggesting extensive DVT, may have negative results on objective testing. Thus, objective testing is mandatory to confirm or exclude a diagnosis of DVT.14–16
The location of the initial DVT has an impact on the incidence of recurrence; thus the presence of an ilial femoral vein thrombosis was shown to have a higher rate of recurrent VTE compared with popliteal vein thrombosis.17 Also, there is a high correlation between venographic results as measured by the Marder Score and recurrence of VTE.18
The prognosis for long-term survival and recurrent VTE may be worse for patients presenting with PE as opposed to DVT. This may be a reason to treat patients presenting with PE more aggressively in the future, but at the present time, anticoagulant management for each entity is identical. Various studies have attempted to identify risk factors for recurrent VTE, including fatal PE, in patients presenting initially with PE. Factors contributing to recurrent VTE include length of initial hospitalization, presence of cancer, older age, hospitalization for multiple injuries, and surgery within 3 months.19,20 Risk factors for an adverse outcome include factors such as older than age 70, hypotension, congestive heart failure, chronic obstructive pulmonary disease (COPD), cancer, presence of a DVT, and right ventricular hypokinesis on echocardiography. Using a standardized Pulmonary Embolism Severity Index21 and measurement of troponin and beta-type natriuretic peptides are useful in the initial diagnosis and in estimating prognosis in patients presenting with PE.22–27
 Etiology and Pathogenesis
Etiology and Pathogenesis
Pulmonary embolism occurs in at least 50% of patients with objectively documented proximal vein thrombosis.1 Many of these emboli are asymptomatic. The clinical importance of PE depends on the size of the embolus and the patient’s cardiorespiratory reserve. Usually only part of the thrombus embolizes, and 30% to 70% of patients with PE detected by angiography also have identifiable DVT of the legs.11,12 Deep vein thrombosis and PE are not separate disorders but a continuous syndrome of VTE in which the initial clinical presentation may be symptoms of either DVT or PE. Therefore, strategies for diagnosis of VTE include both tests for detection of PE (lung scanning, computed tomography [CT], or pulmonary angiography)8–10 and tests for DVT of the legs (ultrasound or venography)11–13
 Prevention of Venous Thromboembolism
Prevention of Venous Thromboembolism
Over the years, numerous clinical trials have been carried out for the prevention of VTE, particularly in patients undergoing orthopedic surgery and in hospitalized medical patients. Agents tested include heparin, low-molecular-weight heparin, fondaparinux, warfarin, and more recently, specific inhibitors of activated factor X or thrombin. In addition, medical devices and, in particular, intermittent pneumatic compression alone or in addition to pharmacologic agents have been studied. Effective prophylaxis against VTE is now available for most high-risk patients; prophylaxis is more effective for preventing death and morbidity and more cost-effective than treatment of the established disease. Evidence-based recommendations for the prevention of VTE are available.5,6
 Assessment of Clinical Probability
Assessment of Clinical Probability
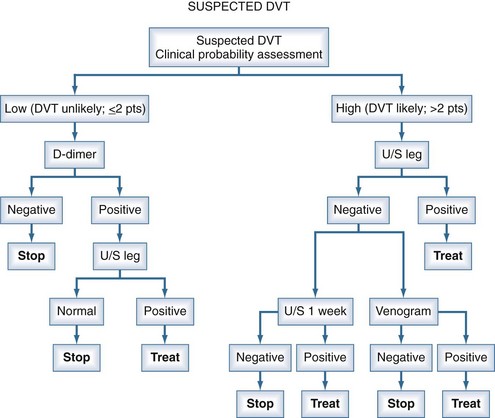
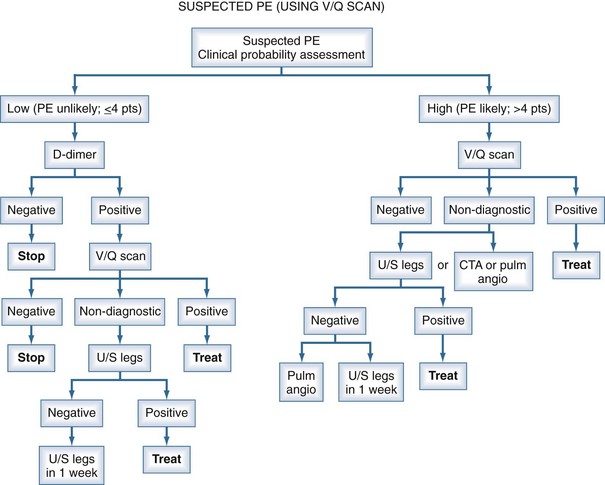
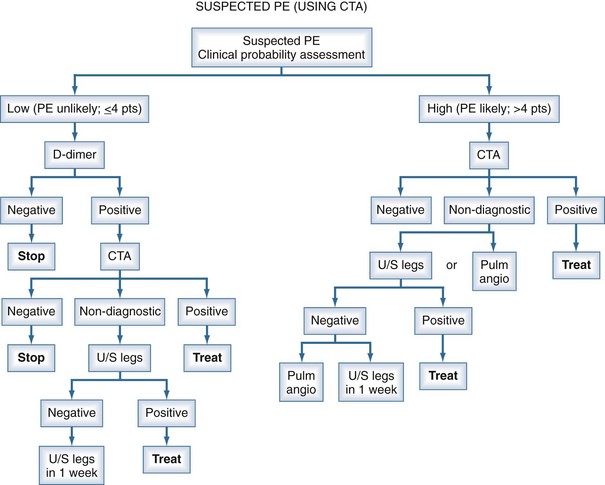
Management studies over the past 2 decades have demonstrated that patients can be assigned categories of pretest probability using decision rules such as the Geneva Score or the approach of Wells.28–34 With the shift of the burden of thromboembolic disease to the out-of-hospital population, these clinical probability guidelines have proven to be extremely useful in stratifying patients into low, moderate, or high risk for the diagnosis of PE. However, the prevalence of PE in these categories is not sufficiently low or high to withhold further investigations altogether based on the clinical probability assessment. The measurement of a D-dimer or performance of an objective diagnostic test is mandatory to exclude or confirm the presence of PE in many patients. The assessment of pretest probability and measurement of the D-dimer have now been integrated into diagnostic algorithms for PE (using either CT angiography [CTA] or ventilation/perfusion [V/Q] scanning) and for DVT (using ultrasonography to objectively confirm the diagnosis28–34 (Figures 62-1, 62-2, and 62-3).
D-Dimer Assay
Measurement of the plasma D-dimer has been extensively studied for the exclusion of patients with suspected PE.35–39 Numerous assays for the D-dimer exist, but the most extensively studied have been enzyme-linked immunosorbent assay (ELISA) and quantitative rapid ELISA, which have high sensitivity and negative likelihood ratios equal to a normal perfusion lung scan. A positive D-dimer result is not useful for the exclusion of PE. Numerous management studies have demonstrated that PE can be excluded without performing imaging studies in patients with a low clinical probability35–39 (see Figures 62-2 and 62-3). Patients with a high clinical probability (i.e., PE likely) should not undergo D-dimer testing but go directly to objective diagnostic tests.
 Differential Diagnosis
Differential Diagnosis
The differential diagnosis in patients with suspected PE includes cardiopulmonary disorders for each of the modes of presentation (see Clinical Features). For the presentation of dyspnea and tachypnea, they include atelectasis, pneumonia, pneumothorax, acute pulmonary edema, bronchitis, bronchiolitis, and acute bronchial obstruction. For pulmonary infarction exhibited by pleuritic chest pain or hemoptysis, they include pneumonia, pneumothorax, pericarditis, pulmonary or bronchial neoplasm, bronchiectasis, acute bronchitis, tuberculosis, diaphragmatic inflammation, myositis, muscle strain, and rib fracture. For the clinical presentation of right-sided heart failure, they include myocardial infarction, myocarditis, and cardiac tamponade. For cardiovascular collapse, they include myocardial infarction, acute massive hemorrhage, gram-negative septicemia, cardiac tamponade, and spontaneous pneumothorax.
 Diagnostic Imaging
Diagnostic Imaging
Computed Tomography and Computed Tomography Angiography
Spiral CT imaging has gained an increasingly important role in the diagnosis of PE in recent years and is now the primary imaging test in most centers. Single-detector spiral CT is highly sensitive for large emboli (segmental or larger arteries) but much less sensitive for emboli in subsegmental pulmonary arteries40; such emboli may be clinically important in patients with severely impaired cardiorespiratory reserve. Therefore, a negative result by single-detector spiral CT should not be used alone to exclude the diagnosis of PE. A filling defect of a segmental or larger artery on single-detector spiral CT is associated with a high probability (>90%) of PE.40
The development of multidetector row CT, together with the use of contrast enhancement, has further improved the utility of CT for the diagnosis of PE.41–44 Contrast-enhanced CTA has the advantage of providing clear results (positive or negative) with a relatively low rate of non-diagnostic test results, good characterization of nonvascular structures for alternate or associated diagnoses, and the ability to simultaneously evaluate the deep venous system of the legs (CT venography [CTV]).
The accuracy and clinical utility of multidetector CTA and combined CTA-CTV was evaluated in the PIOPED II Study.42 Among 824 patients with a reference diagnosis and a completed CT study, CTA was inconclusive in 51 (6%) because of poor image quality. Sensitivity of CTA was 83%, and specificity was 96%. CTA and CTV were inconclusive in 87 (11%) of 824 patients because the image quality of either CTA or CTV was poor. Multidetector CTA-CTV had a higher sensitivity (90%) than CTA alone (83%), with similar specificity (about 95%) for both testing techniques. Positive results on CTA in combination with a high or intermediate probability of PE by the clinical assessment, or normal findings on CTA with a low clinical probability, had a predictive value (positive or negative) of 92% to 96%.32 Such values are consistent with those generally considered adequate to confirm or rule out the diagnosis of PE. Additional testing is necessary when clinical probability is discordant with CTA or CTA-CTV imaging results.42
Radionuclide Lung Scanning
Radionuclide V/Q scanning continues to have a role in the diagnosis of suspected PE. A normal perfusion lung scan excludes the diagnosis of clinically important PE.45,46 A normal perfusion lung scan is found in approximately 10% of patients with suspected PE seen at academic health centers or tertiary referral centers. A high-probability V/Q scan result (i.e., large perfusion defects with ventilation mismatch) has a positive predictive value for PE of 85% and provides a diagnostic endpoint to give antithrombotic treatment in most patients.45–47 A high-probability V/Q scan is found in approximately 10% to 15% of symptomatic patients. For patients with a history of PE, careful comparison of the lung scan results to the most recent lung scan is required to ensure the perfusion defects are new. Further diagnostic testing is indicated for patients with a high-probability V/Q scan who have a “low” pretest clinical suspicion, and in those who are at high risk for major bleeding, to reduce the likelihood of a false-positive diagnosis.
The major limitation of V/Q scanning is that the results are inconclusive in most patients, even when considered together with the pretest clinical probability.45 The nondiagnostic V/Q scan patterns are found in about 70% of patients with suspected PE.12,45,47 These lung scan results have historically been called “low-probability” (matching ventilation/perfusion abnormalities or small perfusion defects), “intermediate probability,” or indeterminate (because the perfusion defects correspond to an area of abnormality on chest x-ray film). Further diagnostic testing is required in most of these patients because regardless of the pretest clinical suspicion, the posttest probabilities of PE associated with these lung scan results are neither sufficiently high to give antithrombotic treatment nor sufficiently low to withhold therapy. The uncommon exception is the patient with a low clinical suspicion and a so-called low-probability V/Q scan result. However, even in these patients, objective testing for DVT with ultrasound may provide added diagnostic value. A randomized trial has established that CTA is not inferior to using V/Q scanning for excluding the diagnosis of PE when either test is used in an algorithm together with venous ultrasonography of the legs.43
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) appears to be a promising diagnostic approach for PE. However, clinically important interobserver variation exists in the sensitivity for PE, ranging from 70% to 100%.48,49 Further studies are required to determine the clinical role of MRI in the diagnosis of patients with suspected PE.
Pulmonary Angiography
Pulmonary angiography using selective catheterization of the pulmonary arteries is a relatively safe technique for patients who do not have pulmonary hypertension or cardiac failure.45,46 If the expertise is available, pulmonary angiography should be used when other approaches are inconclusive and when definitive knowledge about the presence or absence of PE is required.
Objective Testing For Deep Vein Thrombosis
Objective testing for DVT is useful in patients with suspected PE, particularly those with nondiagnostic lung scan results47 or inconclusive CT results.42 Detection of proximal vein thrombosis by objective testing provides an indication for anticoagulant treatment regardless of the presence or absence of PE and prevents the need for further testing. However, a negative result by objective testing for DVT does not exclude the presence of PE.12
Currently, the primary role for using ultrasound testing of the legs is for those centers that do not have the capability for combined CTA-CTV, or if the results of such imaging are inconclusive. If the patient has adequate cardiorespiratory reserve, serial ultrasound testing for proximal vein thrombosis can be used as an alternative to pulmonary angiography in patients with non-diagnostic lung scan or CT results, and withholding anticoagulant therapy is safe if repeated ultrasound testing of the legs is negative.50–53 The rationale is that the clinical objective in such patients is to prevent recurrent PE, which is unlikely in the absence of proximal vein thrombosis. Selective pulmonary angiography should be done among patients with features suggesting a possible source of embolism other than proximal DVT of the leg (e.g., upper-extremity thrombosis, renal vein thrombosis, pelvic vein thrombosis, or right-heart thrombus).
 Integrated Strategies for Diagnosis of Pulmonary Embolism
Integrated Strategies for Diagnosis of Pulmonary Embolism
Figure 62-3 summarizes the approach to diagnosis of suspected PE using CTA or CTA-CTV as the primary imaging test. Figure 62-2 summarizes the approach to diagnosis using V/Q scanning for settings in which CTA capabilities are not available. Figure 62-3 summarizes the approach to the diagnosis of DVT using ultrasonography. The specific approach used will depend on the local availability of technology, expertise with the different diagnostic techniques, and individual patient circumstances.
An appropriately validated assay for plasma D-dimer, if available, provides a simple and rapid first-line exclusion test in patients with low, intermediate, or unlikely clinical probability. The appropriate use of D-dimer can reduce the need for more expensive imaging tests without compromising patient safety. If a validated D-dimer test is not available or the patient has high clinical probability for PE, diagnostic imaging should be employed. If capability for combined CTA-CTV exists, that is the preferred approach for most patients because it provides a definitive basis to give or withhold antithrombotic therapy in about 90% of patients. Lung scanning may be indicated as the first-line imaging test in women of reproductive age, because the radiation exposure to the breast is significantly less than with CTA.53
Echocardiography
Echocardiography provides a number of independent parameters related to pulmonary hemodynamics and, in addition to measurement of troponin and beta-type natriuretic peptide levels, can identify patients with non-massive PE who are at risk of dying or are candidates for thrombolytic therapy.22–27 Transthoracic echocardiography is particularly useful for patients in the intensive care unit (ICU) and can further identify patients who are candidates for thrombolysis or catheter fragmentation or who may progress to chronic thromboembolic pulmonary hypertension.23,24
 Clinical Course of Venous Thromboembolism
Clinical Course of Venous Thromboembolism
Proximal DVT is a serious and potentially lethal condition. Untreated proximal vein thrombosis is associated with a 10% rate of fatal PE. Inadequately treated proximal vein thrombosis results in a 20% to 50% risk of recurrent VTE events.54,47,55 Prospective studies of patients with clinically suspected DVT or PE indicate that new venous thromboembolic events on follow-up are rare (≤2%) among patients in whom proximal vein thrombosis is absent by objective testing.50–52 The aggregate data from diagnostic and treatment studies indicate that the presence of proximal DVT is the key prognostic marker for recurrent VTE.
Thrombosis that remains confined to the calf veins is associated with low risk (≤1%) of clinically important PE. Extension of thrombosis into the popliteal vein or more proximally occurs in 15% to 25% of patients with untreated calf vein thrombosis.11 Patients with documented calf vein thrombosis should receive either anticoagulant treatment to prevent extension or undergo monitoring for proximal extension using serial noninvasive tests.
The postthrombotic syndrome is a frequent complication of DVT.56,57 Patients with postthrombotic syndrome complain of pain, heaviness, swelling, cramps, and itching or tingling of the affected leg. Ulceration may occur. The symptoms usually are aggravated by standing or walking and improve with rest and elevation of the leg. A prospective study documented a 25% incidence of moderate to severe postthrombotic symptoms 2 years after the initial diagnosis of proximal DVT in patients who were treated with initial heparin and oral anticoagulants for 3 months.56 The study also demonstrated that ipsilateral recurrent DVT is strongly associated with subsequent development of moderate or severe postthrombotic symptoms. Thus prevention of ipsilateral recurrent DVT likely reduces the incidence of the postthrombotic syndrome. Application of a properly fitted graded compression stocking, as soon after diagnosis as the patient’s symptoms will allow and continued for at least 2 years, is effective in reducing the incidence of postthrombotic symptoms, including moderate to severe symptoms.58
Chronic thromboembolic pulmonary hypertension is a serious complication of PE. Historically, thromboembolic pulmonary hypertension was believed to be relatively rare and occur only several years after the diagnosis of PE. A prospective cohort study provides important information on the incidence and timing of thromboembolic pulmonary hypertension.59–61 The results indicate that thromboembolic pulmonary hypertension is more common and occurs earlier than previously thought. On prospective follow-up of 223 patients with documented PE, the cumulative incidence of chronic thromboembolic pulmonary hypertension was 3.8% at 2 years after diagnosis despite state-of-the-art treatment for PE. The strongest independent risk factors were a history of PE (odds ratio 19) and idiopathic PE at presentation (odds ratio 5.7).59 Further clinical studies on identification and prevention of chronic thromboembolic pulmonary hypertension are needed.
 Objectives and Principles of Antithrombotic Treatment
Objectives and Principles of Antithrombotic Treatment
Recommendations for treatment of established VTE are linked to the strength of the evidence from clinical trials using the approach for grading evidence of the American College of Chest Physicians (ACCP) guideline committee.55 Recommendations classified as 1A are supported by evidence from scientifically valid randomized clinical trials (grade A evidence), and the results provide a clear risk-to-benefit conclusion (grade 1). Such recommendations should be implemented for most patients. Grade 2A recommendations also are supported by definitive clinical trial evidence (grade A), but the results indicate a less clear risk-to-benefit conclusion (grade 2); therefore, such recommendations may or may not be appropriate for the individual patient. The remaining grades of recommendation are based on nondefinitive evidence (grade B or C) and are less strong.
 Anticoagulant Therapy
Anticoagulant Therapy
Heparin Therapy
Unfractionated Heparin Therapy
Unfractionated heparin (UFH) has been used extensively to prevent and treat VTE, but more recently, low-molecular-weight heparin (LMWH) has replaced UFH for the treatment of VTE in most cases, either entirely or predominantly in the out-of-hospital setting. However, there are patients in whom UFH by continuous infusion continues to be used primarily because the anticoagulant effect can be reversed by stopping the intravenous (IV) infusion and/or administering protamine sulphate.62 Such patients include critically ill patients in the ICU or cardiovascular unit, patients who may be candidates for interventions requiring interruption of anticoagulant therapy (e.g., surgical procedures, thrombolysis), or patients with severe renal failure.62 In some countries, UFH is the anticoagulant of choice for patients suffering PE who are hemodynamically unstable.
The anticoagulant activity of UFH depends upon a unique pentasaccharide that binds to antithrombin (AT) and potentiates the inhibition of thrombin and activated factor X (Xa) by ATIII.62–64 About one-third of all heparin molecules contain the unique pentasaccharide sequence.62–64 It is the pentasaccharide sequence that confers the molecular high affinity for AT.62–64 In addition, heparin catalyses the inactivation of thrombin by another plasma cofactor, cofactor II, which acts independently of AT.62
Heparin has a number of effects other than inhibition of thrombin and activated factor X.63 These include the release of tissue factor pathway inhibitor; suppression of platelet function; increase in vascular permeability, and binding to numerous plasma and platelet proteins, endothelial cells, and leucocytes. The anticoagulant response to a standard dose of UFH varies widely between patients. This makes it necessary to monitor the anticoagulant effects of UFH, using either the activated partial thromboplastin time (APTT) or heparin levels, and to titrate the dose to the individual patient.62
The simultaneous use of initial UFH and warfarin has become clinical practice for all patients with VTE who are medically stable.62,65 Exceptions include patients who require immediate medical or surgical intervention, such as in thrombolysis or insertion of a vena cava filter, or patients at very high risk of bleeding. Heparin is continued until the International Normalized Ratio (INR) has been within the therapeutic range (2 to 3) for 2 consecutive days.62
It has been established from experimental studies and clinical trials that the efficacy of UFH therapy depends upon achieving a critical therapeutic level of UFH within the first 24 hours of treatment.66–68 Data from double blind clinical trials indicate that failure to achieve the therapeutic APTT threshold by 24 hours was associated with a 23.3% subsequent recurrent VTE rate, compared with a rate of 4% to 6% for the patient group who were therapeutic at 24 hours.67,68 Recurrences occurred throughout the 3-month follow-up period and could not be attributed to inadequate oral anticoagulant therapy.67 The critical therapeutic level of UFH, as measured by the APTT, is 1.5 times the mean of the control value or the upper limit of the normal APTT range.66–68 This corresponds to a UFH blood level of 0.2 to 0.4 U/mL by the protamine sulphate titration assay, and 0.35 to 0.70 by the antifactor Xa assay. It is vital for each laboratory to establish the minimal therapeutic level of UFH, as measured by the APTT, that will provide a UFH blood level of at least 0.35 U/mL by the antifactor Xa assay for each batch of thromboplastin reagent being used, particularly if a new batch of reagent is provided by a different manufacturer.62
Numerous audits of UFH therapy indicate that administration of IV UFH is fraught with difficulty, and that the clinical practice of using an ad hoc approach to UFH dose titration frequently results in inadequate therapy. Use of a prescriptive approach or protocol for administering IV UFH therapy has been evaluated in two prospective studies in patients with VTE.66,68 Both protocols were shown to achieve therapeutic UFH levels in the vast majority of patients. Using the weight-based nomogram, there were fewer episodes of recurrent VTE as compared to standard care. Continued use of the weight-based nomogram has been shown to be similarly effective.69
Adjusted-dose subcutaneous UFH has been used in initial treatment of VTE.70 Four randomized clinical trials compared the efficacy of subcutaneous UFH with subcutaneous LMWH in patients with proven VTE.71–74 Nomograms have been developed for subcutaneous UFH. The importance of achieving the therapeutic range by 24 hours was reaffirmed.75 The largest of these trials compared subcutaneous UFH dose adjusted with the use of APTT by means of a weight-adjusted algorithm with fixed-dose LMWH for the initial treatment of patients with VTE, 16% of who presented with PE.74 Subcutaneous UFH was shown to be similar to fixed-dose LMWH in terms of efficacy and safety.74
Complications of Unfractionated Heparin Therapy
Management of bleeding on heparin will depend on the location and severity of bleeding, risk of recurrent VTE, and APTT; in these instances, heparin should be discontinued temporarily or permanently. Patients with recent VTE may be candidates for insertion of an inferior vena cava filter. If urgent reversal of heparin effect is required, protamine sulphate can be administered.62
Heparin-induced thrombocytopenia is a well-recognized complication of UFH therapy, usually occurring within 5 to 10 days after heparin treatment has started.76,77 Approximately 1% to 2% of patients receiving UFH will experience a fall in platelet count to less than the normal range or a 50% fall in the platelet count within the normal range. In the majority of cases, this mild to moderate thrombocytopenia appears to be a direct effect of heparin on platelets and is of no consequence. However, patients receiving UFH may develop an immune thrombocytopenia mediated by immunoglobulin G (IgG) antibody directed against a complex of PF4 and heparin.29 In some cases, neutrophil acting peptide 2 (NAP-2) and interleukin 8 (IL-8) also play a role in pathogenesis.
The incidence of heparin-induced thrombocytopenia (HIT) is lower with the use of LMWH76,78–82; however, the clinical manifestations may be as or more severe than those seen with UFH. Furthermore, the nadir of the platelet count, onset, and duration of thrombocytopenia have been shown to be somewhat different.80 Recently, delayed onset of HIT has been described, with the onset being as long as several weeks after the end of exposure to heparin, thus making this syndrome sometimes more difficult to diagnose. Furthermore, the incidence and severity of HIT varies among different patient populations, being more prevalent in patients having cardiac or orthopedic procedures than for medical patients.83 The development of thrombocytopenia may be accompanied by arterial or DVT which may lead to serious consequences such as death or limb amputation.76,83
When a clinical diagnosis of HIT is made, heparin in all forms must be stopped immediately.77,84 In most centers, the confirmatory laboratory test is an ELISA for the PF4-heparin complex but where possible, this should be confirmed with a functional assay such as the serotonin release assay.83 In those patients requiring ongoing anticoagulation, an alternative form of anticoagulation must be undertaken immediately because of the high incidence of thrombosis when heparin is stopped.85 Some authorities recommend the use of alternative anticoagulants in all patients once a diagnosis is made. The most common alternative agents are the specific antithrombin, argatroban,77,86,87 or the direct thrombin inhibitor, lepirudin.88–91 Both agents are given by IV infusion. Lepirudin, which is renally excreted, has the advantage that it can be given to patients with hepatic insufficiency,77,85 but it has the disadvantage that with prolonged use, antibodies develop, and some of these can have series deleterious effects, including anaphylaxis.92 Argatroban is only partially excreted by the kidney, so it can be used in persons with renal failure, but it cannot be used in patients with significant hepatic insufficiency.77,85 Both agents can be used in conjunction with vitamin K antagonists, but it should be noted that argatroban by itself increases the INR beyond that observed with warfarin alone, and this must be taken into account in controlling the vitamin K antagonist.87 The alternative antithrombotic agents should be continued until the platelet count is at least back to 100 × 109/L and/or the INR is therapeutic for 2 consecutive days.77 The pentasaccharide, fondaparinux, has been used as an alternative antithrombotic agent in HIT patients, and it has the advantage that it is given by a once-daily subcutaneous injection.93,94 Insertion of an inferior vena cava filter is seldom indicated.
Osteoporosis has been reported in patients receiving UFH in dosages of 20,000 U/day (or more) for more than 6 months.62 Demineralization can progress to the fracture of vertebral bodies or long bones, and the defect may not be entirely reversible.62 Laboratory and clinical studies indicate that the incidence of osteoporosis with use of long-term LMWH is low.62

Full access? Get Clinical Tree