Fig. 61.1
Anatomy of the sciatic nerve. (a) (1) Sciatic nerve, (2) posterior femoral cutaneous nerve, (3) piriformis muscle, (4) tibial nerve, (5) common peroneal (fibular) nerve (Reproduced with permission from Danilo Jankovic). (b) (1) Sciatic nerve, (2) posterior cutaneous femoris nerve, (3) infrapiriform foramen with sciatic nerve and gluteal inferior nerve,(4) piriformis muscle (Reproduced with permission from Danilo Jankovic)
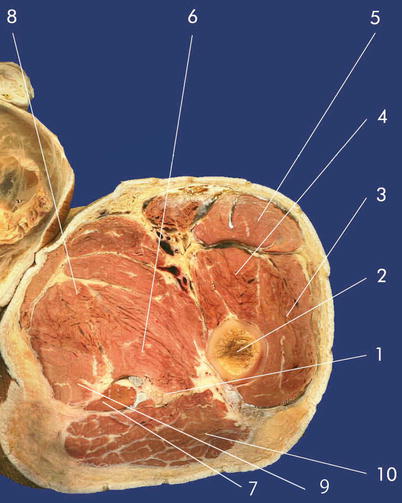
Fig. 61.2
Transversal dissection. (1) Sciatic nerve, (2) femur, (3) vastus lateralis muscle (4) vastus intermedius muscle, (5) rectus femoris muscle, (6) semimembranosus muscle, (7) semitendinosus muscle, (8) adductor brevis muscle, (9) adductor magnus muscle, (10) gluteus maximus muscle (Reproduced with permission from Danilo Jankovic)
Distal to this, the nerve lies on the posterior surface of the adductor magnus muscle, where it is covered by the flexor muscle originating from the ischial tuberosity and thus extends as far as the popliteal fossa (Fig. 61.2). Here it lies slightly laterally and above the popliteal vein and artery, with thick popliteal fascia overlying it. At the proximal end of the popliteal fossa, the nerve usually divides into the thicker tibial nerve, which continues the trunk and the smaller common peroneal (fibular) nerve (Fig. 61.1).
The sensory branches of the nerve innervate the dorsal thigh, the dorsolateral lower leg, and lateral half of the foot, the hip, and knee joint, as well as the femur.
Its muscular branches are responsible for supplying the biceps femoris, semimembranosus, semitendinosus, and adductor magnus muscles.
Indications
Surgical
Superficial procedures in the innervated area.
Carrying out surgical procedures in the region of the lower extremity under tourniquet, but in combination with a block of the lumbar plexus (“three-in-one” block or dorsal psoas compartment block). A need for larger volumes of local anesthetics must be expected (toxicity!).
Therapeutic
An isolated block of the sciatic nerve is rarely indicated. A combination with block of the lumbar plexus or femoral nerve is recommended.
Block Series
A series of six to eight blocks is recommended. When there is evidence of improvement in the symptoms, additional blocks can also be carried out.
Contraindications
Specific
Infection or hematoma in the injection area
Anticoagulant treatment
Lesion in the nerves to be blocked distal to the injection site
Relative
The decision should be taken after carefully weighing up the risks and benefits:
Hemorrhagic diathesis
Stable central nervous system diseases
Local nerve injury
Procedure
This block should be carried out by experienced anesthetists or under their supervision. Full prior information for the patient is mandatory.
Preparations
Check that the emergency equipment is complete and in working order. Sterile precautions, intravenous access, ECG monitoring, pulse oximetry, intubation kit, ventilation facilities, emergency medication.
Materials
Peripheral nerve stimulator
Single-Shot Technique
Fine 26-G needle, 25 mm long, for local anesthesia.
80–100 mm long (120–150 mm for ventral access), short-bevel insulated stimulating atraumatic 22-G needle (15°) with injection lead (“immobile needle”)
Continuous Technique
Tuohy set: 102-mm-long 18-G Tuohy needle with catheter Catheter kit: 18-G needle (80–110 mm, 15°) with catheter.
Syringes: 2, 10, and 20 mL.
Local anesthetics, disinfectant, swabs, compresses, sterile gloves, and drape.
Classic Dorsal Transgluteal Technique (Labat Technique)
Patient Positioning (Fig. 61.3a)
Fig. 61.3
(a) Classic dorsal transgluteal technique (positioning) (Reproduced with permission from Danilo Jankovic). (b) Landmarks. (1) Posterior superior iliac spine, (2) greater trochanter, (3) sacral hiatus, (4) ischial tuberosity, (5) sciatic nerve (Reproduced with permission from Danilo Jankovic)
Lateral decubitus, with the leg being blocked on top (Sims position).
The upper leg is bent at the hip and knee joints and the upper knee lies on the table. The lower leg is straight.
Landmarks (Fig. 61.3b)
The important landmarks are: the greater trochanter and posterior superior iliac spine (and/or sacral hiatus). The greater trochanter and posterior superior iliac spine are located. From the midpoint of the connecting line, a line is drawn medially and the injection point is marked at 5 cm (Labat line).
To check this, another line connecting the greater trochanter and the sacral hiatus is bisected (Winnie line). The two points should coincide.
Skin prep, local anesthesia, sterile draping, drawing up local anesthetic into a 20-mL syringe, checking patency of the injection needle and correct functioning of the nerve stimulator, attaching the electrodes.
Preliminary puncture with a large needle or stylet.
During the procedure, the biceps femoris, semimembranosus and semitendinosus muscles, and the foot must be observed.
Injection Technique
1.
The injection needle is introduced perpendicular to the skin surface (Fig. 61.4).


Fig. 61.4
The injection needle is introduced perpendicular to the skin surface (Reproduced with permission from Danilo Jankovic)
Stimulation current of 1 mA at 2 Hz is selected with a stimulus duration of 0.1 ms.
2.



After about 1–4 cm, there should be direct stimulation of the gluteus maximus muscle.

Full access? Get Clinical Tree








