KEY POINTS
Approximately 20% of deaths in the United States are associated with or occur in an intensive care unit and a substantial majority of these deaths will have some aspect of intensive care treatment either withheld or withdrawn. High-quality care for patients dying in the ICU should incorporate the principles and practice of palliative care and therefore intensive care unit clinicians should familiarize themselves with basic aspects of palliative care.
High-quality communication with critically ill patients and their family is an essential skill for ICU clinicians and one component of palliative care. Communication about end-of-life issues requires navigating cognitive, emotional, and ethical elements of decision making.
The use of structured, patient- and family-centered approaches to end-of-life communication improves outcomes among family of deceased ICU patients.
The provision of high-quality palliative care requires a multidisciplinary approach to effectively address physical, psychosocial, and spiritual suffering.
An ideal model for palliative care in the ICU should include integrating principles of palliative care into routine ICU practice as well as the use of palliative care, ethics, and spiritual support teams for some patients and family members.
Withdrawing or withholding life-sustaining therapy is widely accepted and common in the United States. This practice should adhere to the standards for quality medical care including appropriate documentation, attention to detail, an explicit plan for addressing patient, family, and clinician needs, and interdisciplinary implementation. An institutional protocol may help achieve these standards.
THE ROLE OF PALLIATIVE CARE IN THE ICU
Palliative care is a unique approach and a distinct model of clinical care when compared to conventional care. It focuses on patients with serious, life-threatening illness and is characterized by three main principles.1The first principle is that the overarching goal of palliative care is to improve the quality of life through the relief of suffering in each of its major domains: physical, emotional, psychosocial, and spiritual. Thus, follows the second principle that palliative care is provided by an interdisciplinary team that generally includes the professions of medicine, nursing, social work/counseling, and chaplaincy. The third principle is that the patient and family are the focus of care rather than the patient individually. An important feature of palliative care for ICU clinicians to understand is that it can be offered simultaneously with aggressive efforts to extend life and does not impose an “either-or choice” between conventional critical care and palliative care.
Given the substantial risk of death for many critically ill and injured patients, ICU clinicians can enhance important aspects of patient and family outcomes by considering how to integrate these principles into their practices. Although not focused primarily on the relief of suffering, critical care has increasingly begun to value the importance of symptom management,2-4 emotional and psychological outcomes,5 and psychosocial support.6-8 More generally, investigation into health-related quality of life following critical illness has identified important deficiencies9,10 especially when considered in the context of the substantial resources invested. For example, a prospective, cohort study of 126 patients designated as chronically dependent on mechanical ventilation found that at 1 year only 9% were alive with a good outcome at a cost of $3.5 million per independently functioning survivor.10 These findings raise the notion that critical care may need to evolve and expand its purview into post-ICU issues of survivorship, analogous in some ways to emerging focus on cancer survivorship.11
Effective interdisciplinary care has proven value in intensive care units.12,13 Furthermore, patients and families report that interdisciplinary collaboration is a key element to good end-of-life care,14 yet the value that intensivists place on nursing involvement in end-of-life decisions is variable as documented in an international survey. A questionnaire completed by 1961 intensivists found that only one-third of surveyed intensivists in the United States, Brazil, Japan, and Southern Europe would involve nursing in end-of-life decision making for a hypothetical patient without a surrogate decision maker as compared to 62% in Northern and Central Europe.15 In addition, interdisciplinary conflict around end-of-life care in ICUs is associated with increased professional burnout, depression, and posttraumatic stress among ICU clinicians, which should further prompt intensivists to work toward improving interdisciplinary collaboration around end-of-life care in ICUs.16-18
While the three main principles of palliative care are relevant to the practice of quality critical care, two recent randomized, controlled trials of interventions designed to integrate fundamental aspects of palliative care such as basic communication techniques for critical care clinicians into existing ICUs systems of care have not shown significant improvements.19,20 These studies suggest that significant improvements may require more in-depth interventions as well as involvement of palliative care specialists in the care of these patients and families.
Fortunately, palliative care is emerging as a separate medical subspecialty that can be offered in conjunction with conventional critical care. Hospice and Palliative Medicine was recognized as a new medical subspecialty by the American Board of Medical Specialties in 2005 and in the United States the growth of palliative care programs in acute care hospitals has been substantial with 30% of US hospitals and 70% of hospitals with greater than 250 beds offering palliative care programs in 2005, representing a 96% increase since 2000.21 Palliative care consults reduce physical and psychological suffering,22-24 increase patient and family satisfaction,23 reduce costs among patients who die,21 and increase survival in outpatient populations.24,25
Specific to critical care, several studies have found that proactive approaches to palliative care and/or ethics consultations reduce both ICU length of stay (LOS) and the use of specific, aggressive ICU therapies among patients who died in the ICU26-30 and one multicenter, randomized, controlled trial found that proactive ethics consultations could achieve reductions in hospital LOS, ICU LOS, and days of mechanical ventilation among decedents.31 Importantly, none of these investigations found a difference in overall mortality between their control and intervention groups suggesting proactive, palliative care interventions do not shorten survival. Furthermore, each found high rates of acceptance among ICU clinicians and families.
In the United States, 22% of deaths are associated with an ICU admission,32 an observation that may seem incongruous with the notion of intensive care as representing aggressive attempts at cure. However, given that the leading causes of death in the United States often incorporate a trajectory that includes an unexpected and potentially reversible decline, it becomes understandable why a substantial proportion of US deaths are accompanied by ICU admissions. The top four causes of death for Americans today are chronic health conditions and include heart disease, cancer, stroke, and chronic respiratory diseases.33
The trajectory of declining health status preceding death has been conceptualized as assuming one of several patterns.34,35 The most common pattern is of chronic illness with progressive organ failure punctuated by acute exacerbations and incomplete improvement. Examples of conditions that often assume this pattern include congestive heart failure and chronic respiratory diseases. A second common pattern is observed in terminal conditions such as advanced cancer where patients often experience good functional status until an acute, rapid decline followed by death. Frailty that may accompany advanced age or progressive dementia generally imposes a poor functional status over an extended period of time prior to death.
Acute care hospitalizations may occur at any stage during declining health status and especially during an acute exacerbation of a chronic health condition. These three conceptual representations of health status prior to death, combined with inherent uncertainty in prognostication, help explain why the majority of Americans die in an institutional setting. Fifty-eight percent of Americans die in an acute care hospital, 21% die in a nursing home or other chronic care facility, and 21% die at home.36 The reliance on acute care hospitals as the location for end-of-life care often encourages the option of an ICU admission, and in fact having increased ICU resources available is a significant predictor of using critical care services during a terminal hospitalization.37 Thus, ICU clinicians often find themselves providing end-of-life care to many ICU patients and families during their careers. Improved communication about end-of-life care and advance care planning may help limit terminal ICU admissions for some patients,38 but the ICU will always remain a setting where death and end-of-life care are relatively common. Furthermore, many patients who survive the ICU will also have important palliative care needs. Therefore, critical care clinicians must become skilled at providing palliative care.
PROVIDING PALLIATIVE CARE IN INTENSIVE CARE UNITS
Whether the end-of-life care provided in ICUs is also palliative care is an important distinction and as described above should necessarily include the three main principles of palliative care: relief of suffering, collaborative interdisciplinary care, and patient/family-centered care. Assistance from formal palliative care or ethics teams can be beneficial. Asking whether improved palliative care should be achieved through involvement of palliative care specialists or training in palliative care for critical care clinicians raises a false dichotomy: High-quality palliative care in the ICU will require both approaches simultaneously.39 Discussed below are approaches that ICU clinicians can integrate into their practices to better meet the palliative care needs of their patients including improving communication, pain management, and spiritual support.
Effective communication between patients, families, and clinicians in ICUs is a cornerstone to providing patient/family-centered care, yet significant deficiencies in the quality of communication40,41 as well as resultant adverse psychological outcomes among families have been reported.42 Analyses of audiotaped ICU family conferences have found specific opportunities for improvement including listening and responding to questions, providing emotional support, and addressing palliative or ethical principles.43 Other analyses of these data found that when physicians spoke less and families spoke more during ICU family conferences, families’ ratings of the quality of communication were higher.44 Notably, families of patients who survive report less satisfaction with communication than families of patients who die, suggesting a broad opportunity for improvement in communication regardless of anticipated survival status.45
Communication about end-of-life care in the ICU can be especially challenging. This communication is complicated by several factors: There is typically reliance on surrogate decision makers,46 ICU clinicians often lack a longitudinal relationship with the patient and family, and the time between consideration of end-of-life care and death is often brief.47 An important objective of communication about end-of-life care in the ICU is to determine the goals of care for the patient. Physicians have an obligation to provide information on the diagnosis and prognosis whereas families are generally the best source of information about patients’ beliefs and values. The recommended framework for end-of-life decisions is a shared decision-making model in which the physician and family jointly assume responsibility for decisions about end-of-life care.48,49 Substantial variation, however, is observed in the degree to which families want to be responsible for decisions about end-of-life care. Some family members favor a shared decision-making role with physicians50,51 whereas others do not wish to be involved in decision making or conversely prefer the physician not be involved in decision making.52-54 There is also substantial variation in the degree to which physicians report involving families in ICU discussions about end-of-life care. Families in the United States are traditionally more involved in these decisions than families in Europe55 and nearly 100% involvement among families is reported in some Asian countries.56,57
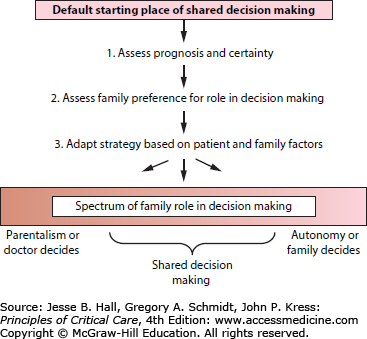
In order to accommodate the variation in preferences among families, one recommended procedure is offered in Figure 18-1.58,59 This approach begins with a default position of shared decision making. The physician assesses prognosis and the degree of prognostic certainty and offers to assume a greater burden of decision making as prognosis worsens and certainty increases. This framework assumes a certain degree of confidence in physician prognostication, which has limitations, but is nonetheless important for families to make informed choices.
The second step is to assess family preferences in decision making and finally to adapt the strategy to both the clinical context and family preferences. Significant communication skills are necessary to align clinicians and families around shared goals of care and implement this decision-making framework, and most physicians have not received formal education or training in communication.60,61 Fortunately there are descriptive reports and clinical trials that provide insights into how ICU clinicians should approach family conferences.58,62
After evaluating 21 articles representing 16 unique interventions, a systematic review of interventions to improve ICU communication identified two recurring themes associated with improved outcomes.62 First, the use of a structured approach to communication with families improves patient- and family-centered outcomes and timing of decisions about major treatments. The VALUE mnemonic detailed in Table 18-1 is a useful tool for clinicians demonstrated, in a randomized trial, to improve family-centered outcomes of emotional distress and lessen the use of nonbeneficial ICU therapies.63Table 18-2 provides additional guidance for a structured and evidence-based approach to communication during ICU family conferences.59 The three stages of an ICU family conference include activities prior to the conference, during the conference, and following the conference. Prior to the family conference, consensus should be achieved among the clinicians treating the patient to ensure consistency and avoid confusion. The setting for the conference should include a private, quiet location free from distractions,64 and each person present should introduce themselves and describe their relationship, whether clinical or personal, to the patient.
Useful Mnemonic for Critical Care Clinicians Leading ICU Family Conferences (Demonstrated to Improve Family Outcomes)63
| Mnemonic Cue | Explanation |
|---|---|
| Value | Appreciate what family members say |
| Acknowledge | Explicitly recognize family emotions |
| Listen | Allow families time to speak and to think about information presented |
| Understand | Learn and understand who the patient is as a person |
| Elicit | Solicit questions from family members |
Key Steps for Improving Communication During Interdisciplinary ICU Family Conferences
| Stages of the ICU Family Conference | Common Steps and Topics |
|---|---|
| Prior to a family conference in the ICU |
|
| Conducting a family conference in the ICU |
|
| Finishing a family conference in the ICU |
|
The physician usually opens the conference and a strategy to achieve family-centered communication starts by asking the family their perception of the patient’s status including diagnosis and prognosis.65 This should be followed by active listening and offering families adequate time to speak.44 Then the physician often provides medical information; it is important to do this using language the family understands and confirm their understanding. The conversation should center on what the patient’s values and treatment preferences would be in the current clinical context.43 The use of empathetic statements66 and acknowledging and addressing family emotions can improve family experiences.43 Families should be assured that the patient will not suffer or be abandoned prior to death66 and receive explicit support for their decisions.67 The conclusion of a family conference should include summarizing the discussion and decisions, asking for questions, affirming family decisions,67 and arranging for follow-up as necessary.
After the family conference, it is important to establish that the family understands the information provided and the treatment plans and knows how to contact the clinical team if additional questions arise. The role of nurses during and following ICU family conferences is important as nurses often find themselves functioning as the front line for family questions and concerns.
The second theme identified in the systematic review of interventions to improve ICU communication was the provision of printed information to families. This practice increases family comprehension and reduces emotional distress associated with ICU hospitalizations.62 This is a simple and effective mechanism to improve ICU clinician-family communication and several major professional societies including the American College of Chest Physicians, American Thoracic Society, and the Society for Critical Care Medicine have appropriate materials available through their respective Web sites. Another excellent source for ICU palliative care resources can be found from the Center to Advance Palliative Care’s IPAL-ICU Project available at http://www.capc.org/ipal-icu/.68
Pain assessment and management is a broad topic and full discussion is beyond the scope of this chapter, yet some basic aspects to pain management are especially relevant to ICU clinicians if a transition to end-of-life care is planned. ICU patients experience significant physical suffering with 55% to 75% of ICU patients who were able to complete assessment tools reporting pain, anxiety, sleep disturbance, hunger, or thirst and rating these symptoms as moderate to severe in intensity.69 Furthermore, among chronically critically ill patients completing symptom assessment tools, 90% are symptomatic with 54% reporting pain at the highest possible level.70
The first step in symptom management is a symptom assessment. Pain is an important symptom to address, although there are many other symptoms that are prevalent among critically ill patients as noted above. A patient’s self-report is considered the most reliable pain assessment and among patients who can communicate the 0-to-10 numeric rating scale is the most commonly used assessment tool. This simple and reliable tool has been validated for ICU patients.71

Full access? Get Clinical Tree