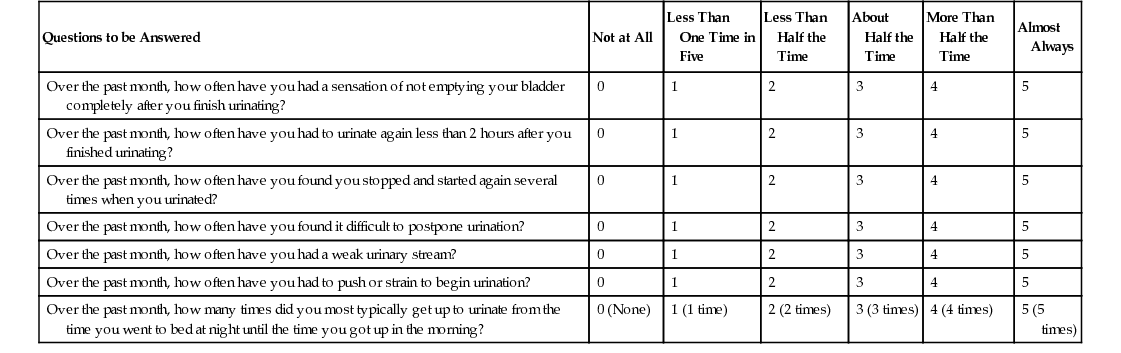
Kenneth Peterson Benign prostatic hyperplasia (BPH), an almost ubiquitous phenomenon among older men, is a noncancerous enlargement of the prostate gland. Although the exact prevalence of BPH is unknown, by the eighth decade of life BPH is present in more than 90% of all men.1 The prostate gland undergoes its first growth spurt during puberty and attains an average size of 20 g ( The development of the prostate gland depends on androgen secretion, and both the presence of testes and advancing age are necessary for the development of BPH. Dihydrotestosterone (DHT) is the main mediator of the growth and secretory function of the prostate and is the active metabolite that results from testosterone conversion.2 BPH seems to be related to a complex interaction between androgen and estrogen secretion; abnormal serum elevations of androgen and estrogen stimulate prostatic growth. Other factors that contribute to prostatic enlargement appear to be related to the elaboration of certain growth factors, the formation and maintenance of DHT levels, and the functioning of androgen receptors.2 Men with BPH can also have bladder outlet obstruction (BOO), lower urinary tract symptoms (LUTS), or a combination of these problems.3 Thus, the symptoms of BPH are either obstructive or irritative in character, depending on the particular BPH components involved. Obstructive symptoms include urinary hesitancy, decreased caliber and force of the stream, and postvoid dribbling. These symptoms are related to BOO. Irritative symptoms include frequency, urgency, and nocturia and occur as a result of decreased functional bladder capacity and instability or infection. In men, the term LUTS was originally used to describe the irritative symptoms primarily associated with BPH but has been expanded to include symptom related to bladder storage and/or voiding disturbances; the term used now is male LUTS or MLUTS.3 On occasion, hematuria accompanies BPH. Episodic symptoms may be present during many years with a gradual increase in the intensity of symptoms over time. A thorough history is important and should include questions related to general health, history of type 2 diabetes, and sexual health. A family history of BPH or prostate cancer should be explored as well as any past history of urethral trauma, urethritis, or urethral instrumentation. Current over-the-counter and prescription medication use should be explored to determine the use of anticholinergics (including diphenhydramine and those in cold preparations), which can impair bladder contractility, or sympathomimetics such as pseudoephedrine, which increase outflow resistance. Diuretics, which can cause an increased output of urine, may lead to urinary retention, especially in the presence of a partially decompensated detrusor muscle. Frequency volume charts or voiding diaries can be used to evaluate nocturia.3 BPH symptoms may be quantified by a symptom index developed by the American Urological Association to aid in classifying symptom severity and in developing a treatment plan4 (Table 147-1). Symptoms are rated according to frequency of occurrence.4 TABLE 147-1 American Urological Association Symptom Index for Benign Prostatic Hyperplasia4 A digital rectal examination (DRE) is done to evaluate the prostate gland for size, consistency, shape, symmetry, and abnormalities and to evaluate anal sphincter tone. Prostatic nodules or induration should be noted on rectal examination because these findings suggest prostate cancer. The normal prostate is heart shaped and measures approximately 4 × 3 × 2 cm ( A urinalysis should be performed to exclude a urinary tract infection or hematuria. Determination of the creatinine level may be prudent to assess renal function. Office-based bladder ultrasound examination to determine postvoid residual is helpful in the diagnosis and treatment of BPH. According to American Urological Association guidelines, measurement of serum prostate-specific antigen (PSA) is appropriate for men with a life expectancy of more than 10 years in the presence of physical findings suggestive of prostate cancer (abnormal DRE findings) and if 5α-reductase inhibitor therapy is planned.6 Men with BPH should be advised that data from the Prostate Cancer Prevention Trial revealed that BPH is not a risk factor for prostate cancer.7 Assessment of free PSA and PSA velocity (the rate of rise per year) may help increase specificity for prostate cancer. Noncancerous prostate growth rarely results in a PSA velocity of more than 0.75 ng/mL/yr.8 The use of finasteride, a medication indicated for BPH, may increase the accuracy of PSA testing and even decrease the incidence of prostate cancer in select men at increased risk of prostate cancer.9 Symptoms of BOO mandate evaluation for bladder calculi, urethral stricture, cancer of the prostate, and bladder neck contracture. Bladder cancer (as well as renal cancer) should be a consideration in a male patient with unexplained hematuria. Urinary tract infection must be excluded if there are complaints of irritative voiding symptoms. If abnormalities are found on neurologic examination and problems with urinary retention are present, neurologic disease must be considered. Prostate cancer should be considered when an asymmetric enlargement, nodule, or induration is palpated on rectal examination. The traditional management goal for treatment of BPH has been relief of symptoms to improve quality of life. Treatment focuses on balancing the severity of the patient’s symptoms with potential side effects of therapy. For men with BPH who have mild symptoms and no complications, behavioral modifications including limiting fluids before bedtime, limiting use of caffeine and alcohol, and double voiding can be helpful. Treatment options include watchful waiting and lifestyle modifications, alpha1-adrenergic antagonist therapy, 5α-reductase enzyme inhibitor therapy or combination drug therapy, balloon dilation, and surgery.6 The benefits and risks associated with each treatment should be explained. It is important to advise the patient that if he chooses watchful waiting, other treatment approaches can be considered at any time if symptoms increase. Alpha-adrenergic antagonists have long been the main treatment of BPH. They work by relaxing smooth muscle in the bladder neck, prostate capsule, and prostatic urethra. Doses can be titrated up while monitoring for side effects. Terazosin and doxazosin need to be initiated at bedtime to reduce dizziness and postural effects. If patients cannot tolerate this class of medications, 5α-reductase inhibitor therapy (e.g., dutasteride and finasteride) can be initiated as monotherapy. These drugs work by shrinking prostatic glandular hyperplasia by decreasing tissue DHT levels, but it may take up to 6 to 12 months to see improvement in symptoms based on reduced prostate size. Phosphodiesterase-5 (PDE5) inhibitors such as sildenafil or tadalafil can be used for men with mild to moderate BPH symptoms and erectile dysfunction. Combination therapy with alpha-adrenergic antagonists and 5α-reductase inhibitors can also be used for men with large prostates and severe symptoms.6 Use of herbal preparations such as saw palmetto, Cernilton, and Pygeum africanum may be increasing, but there is limited evidence as to their safety and efficacy.10–12 Saw palmetto may contribute to increased risk of bleeding, and patients need to notify their providers so that it can be stopped before invasive procedures. Balloon dilation reduces symptoms in the short term, but long-term follow-up after the procedure has not been adequately studied. Transurethral resection of the prostate (TURP), transurethral incision of the prostate, and open prostatectomy are surgical procedures that are effective for severe BPH. TURP has long been considered the gold standard treatment of BOO, but it is limited to prostates weighing less than 100 g and is associated with significant complications and mortality.13
Prostatic Hyperplasia (Benign)
Benign Prostatic Hyperplasia
Definition and Epidemiology
Pathophysiology
 ounce) by the age of 20 years. The gland then undergoes a second growth spurt during the fifth decade of life.
ounce) by the age of 20 years. The gland then undergoes a second growth spurt during the fifth decade of life.
Clinical Presentation
Questions to be Answered
Not at All
Less Than One Time in Five
Less Than Half the Time
About Half the Time
More Than Half the Time
Almost Always
Over the past month, how often have you had a sensation of not emptying your bladder completely after you finish urinating?
0
1
2
3
4
5
Over the past month, how often have you had to urinate again less than 2 hours after you finished urinating?
0
1
2
3
4
5
Over the past month, how often have you found you stopped and started again several times when you urinated?
0
1
2
3
4
5
Over the past month, how often have you found it difficult to postpone urination?
0
1
2
3
4
5
Over the past month, how often have you had a weak urinary stream?
0
1
2
3
4
5
Over the past month, how often have you had to push or strain to begin urination?
0
1
2
3
4
5
Over the past month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning?
0 (None)
1 (1 time)
2 (2 times)
3 (3 times)
4 (4 times)
5 (5 times)
Physical Examination
 ×
×  ×
×  inches). With BPH, there may be uniform or focal enlargement of the prostate. The size of the prostate does not always correlate with symptom severity, however, and should not direct therapy. The median sulcus is often obliterated in BPH, and it is often difficult to palpate over the base of the prostate because of the gland’s enlarged size in advanced stages. With BPH, the gland is nontender and should be rubbery and smooth in consistency. A focused neurologic examination is done to assess sacral nerve roots to identify neurologic problems that could be contributing to bladder symptoms. A lower abdominal examination is necessary to ascertain bladder distention from urinary retention.3,5
inches). With BPH, there may be uniform or focal enlargement of the prostate. The size of the prostate does not always correlate with symptom severity, however, and should not direct therapy. The median sulcus is often obliterated in BPH, and it is often difficult to palpate over the base of the prostate because of the gland’s enlarged size in advanced stages. With BPH, the gland is nontender and should be rubbery and smooth in consistency. A focused neurologic examination is done to assess sacral nerve roots to identify neurologic problems that could be contributing to bladder symptoms. A lower abdominal examination is necessary to ascertain bladder distention from urinary retention.3,5
Diagnostics
Differential Diagnosis
Management

Full access? Get Clinical Tree


Prostatic Hyperplasia (Benign)
Chapter 147




