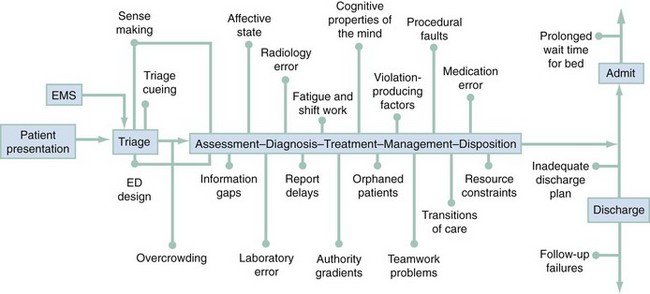
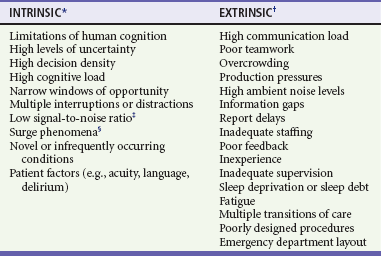
Chapter 197 The overall process of patient care in the emergency department (ED) begins with the initial decision by the patient (or caregiver or family) to seek emergency assistance and ends with the patient’s disposition and follow-up. The care process is highly complex, with many separate components, people, and interfaces with other processes in the health care organization (Fig. 197-1). This complexity, among other things, provides many opportunities for process failures, “errors,” and adverse outcomes. Although process failures in health care have been studied for decades, most of that effort originated from outside of the field of health care, with health care professionals largely unaware of it.1 This began to change in the early 1990s when the Harvard Medical Practice Study reported that almost 4% of hospitalized patients suffered significant adverse events during their care and that almost 30% of these were due to human error.2 The study noted that failures in ED care accounted for only approximately 3% of all adverse events, but more than 90% of adverse ED events were judged to be preventable. This study and others ultimately led the Institute of Medicine to issue a report in 1999 titled To Err Is Human: Building a Safer Health System.3 This report provoked the interest of the media and the general public and thrust the issue of safety in health care onto the national agenda. The major accomplishment of the Institute of Medicine report was the introduction of some of the fundamental concepts regarding safety in complex systems for the first time into the world of health care. The most transforming concept was the idea that failures (or errors) in care are not the result of bad decisions or bad individuals but are instead intrinsic properties of the processes of care in the health care system. Thus efforts to reduce these failures should be focused on changing the processes of care rather than on identifying, retraining, or punishing the workers. The response within health care was mixed. Most health care professionals focused on the projected number of deaths due to error, arguing that they were either too high4,5 or too low,6 and a third, smaller group argued that the concept of error is essentially contestable and thus an approach aimed at counting errors is fundamentally flawed.7 The transforming concept of “system failure” rather than “human error” gradually gained acceptance, despite going against the natural human tendency to believe that individuals cause outcomes. This viewpoint is problematic because it undermines a clinician’s sense of free agency; health care providers prefer not to view themselves as trapped in a system that is moving inexorably toward a poor outcome. Within emergency medicine, safety and quality have been addressed by task forces, interest groups, and special sections examining the practice of emergency care, its processes, and environments with tools from the “science of safety” to improve performance and to cultivate patient safety.8 A basic curriculum for teaching about safety at the undergraduate level was developed, with similar efforts taking place to implement safety concepts into medical education.9 Interesting lines of research on the safety and processes within emergency care have been performed, with a number of patient safety case reports published in the emergency medicine literature.10 Chisholm11 reported that emergency physicians are interrupted, on average, approximately once every 6 minutes and that two thirds of those interruptions cause a change in task; this is important because both interruptions and task switching frequently lead to process failures. Fordyce12 reported that self-detected errors occurred in almost 20% of all ED cases but that only 2% were associated with adverse events. Fordyce’s work emphasizes that errors are ubiquitous but only rarely combine with other factors to produce adverse events, and it supports the notion that focusing on elimination of errors is not likely to be a productive strategy for improvement. Coiera13 studied emergency physicians in Australia and reported high communication loads and found similar levels of interruptions. Morey14 reported that specific training of emergency physicians and nurses to work together in teams led to reductions in failures and improved performance. Perry and colleagues15,16 identified a number of unexpected yet highly consequential failures of information technology that were difficult to detect, some occurring during emergency resuscitations. Wears and Perry17 noted ergonomic shortcomings in the workplace and pointed out their potential to contribute to failures in care. Hall18 identified significant delays related to ED layout, with time to assessment of chest pain patients being longer for patients placed behind a door or who were 25 feet or farther away from the physicians assigned to care. These examples of safety research in emergency care demonstrate the wide range of known and unknown contributors to patient safety and the importance of the work processes that overlay this complex work environment. Many characteristics of emergency medical practice make it vulnerable to failures (Table 197-1).19–26 This section focuses on some of the principal factors that contribute to adverse outcomes and how they might be better managed to improve safety. Table 197-1 Characteristics of the Emergency Department That Affect Performance *Intrinsic factors are intimately part of the nature of emergency care and as such are not amenable to change but instead must be compensated for. †Extrinsic factors are in principle manageable and typically relate to resource constraints. ‡Low signal-to-noise ratio refers to the low likelihood of a critical diagnosis compared with a benign diagnosis for similarly presenting symptoms and findings (e.g., subarachnoid hemorrhage vs. tension headache). §Surge phenomena are the rapid changes in volume and acuity routinely experienced in many emergency departments. Two frequently overlooked contributors to lowered safety in any work environment are the design of the workspace and the engineering of the tools, technology, and procedures used to perform the work.27 This is especially true for EDs because the majority were not designed for the care actually being delivered there.28 ED caregivers are required to adapt to the space by creating “work-arounds” to cope with the limitations and impediments of the workspace. Consistency is rarely found in equipment across or between areas. For instance, the blood pressure monitor in the ED is often not the same type or model as that used in the radiology department when the patient goes for diagnostic tests. In addition, tools and technology are seldom developed or assessed for their “user-centered design” or ability to be integrated into existing workspace and the associated hazards for doing so. This is most apparent with regard to health information technology, which is often introduced for improvement of safety and quality; however, embedded latent features that can produce clinical failures that are “hard to see” have been demonstrated.29,30 Study of computerized physician order entry by Koppel31 showed that the software facilitated 22 types of medication error risks, for example, displays that prevented a coherent view of the patients’ medications and inflexible ordering formats that generated wrong orders. Other contributors to information technology failure within health care are the lack of usability testing,32 delays in in-service training, and failure to reassess the impact of the new technology and changes in clinical work after implementation.33 The contribution of poor design to the difficulty in maintaining safety in a health care environment is generally overlooked by staff members, who cope with these difficulties as “part of the job.”17 Vigilance is the common solution but despite caregivers’ best efforts cannot be sustained, given competing demands for their attention. This increases the risk of a failure’s not being recognized as linked to the workplace, the procedures, or the equipment, despite being “tightly coupled” to any or all of these. ED crowding has long been recognized as a major source of time-delay failures and a threat to patient safety.34,35 Such delays are not simply an inconvenience to the patient but may give rise to significant adverse events. For example, patients with atypical presentations of severe illness who have been mis-triaged to low levels of acuity may experience inordinate and, occasionally, fatal delays. In other cases, such as community-acquired pneumonia, cellulitis, and lacerations, more expedient care may significantly improve the outcome of the illness. A significant proportion of patients who leave the ED without being seen may have serious illness and incur delays in diagnosis and treatment. At the other end of the process, when the patient is ready for admission to the hospital from the ED, further time-delay errors may occur (see Fig. 197-1). Not only do such delays create throughput problems for the ED and contribute to overcrowding by front-end loading or “entry block,” but they also give rise to discontinuities in care and may lead to adverse events that are difficult to identify because they are manifested once the patient has left the ED.36–39 Manifestations of cognitive overload associated with ED overcrowding are diminished overall with increased use of heuristics (mental shortcuts) in medical decision-making and more biased and risk-laden decisions. Missing information is common in emergency care and can significantly affect quality of care.40 Hospital records, especially discharge summaries, details of past medical history, and other important information, are often difficult to access in an expedient manner, even with electronic medical records. Referral notes sent by family physicians with the patient may not reach the emergency physician or may not contain relevant or significant details. In these situations, emergency physicians make clinical decisions and take action on the basis of incomplete, limited, or erroneous information. Emergency clinicians often end up not seeking additional or clarifying information because of time pressures, patient volume, or limited methods to obtain more information (e.g., the referring physician’s office is closed), essentially accommodating to this “gap” in continuity of care and the associated increase in patient risk.41 Blaming individuals for errors contributes little to an understanding of risk, vulnerability, and failure. A wide variety of ambient, systemic conditions in the ED contribute to the majority of adverse events and near misses that occur (see Table 197-1). Some performance-shaping factors can be considered to be “intrinsic,” part and parcel of the milieu of emergency medicine and thus not amenable to direct control (e.g., cognitive workload, multiple distractions and interruptions, and high acuity). These factors must be managed by strategies to buffer or to mitigate their effects. In contrast, other “extrinsic” performance-shaping factors typically reflect limitations of resources (e.g., staffing ratios, production pressure, and ED layout). When resources are limited, a tradeoff can occur in the ability of the ED to provide safety and quality in patient care. This condition is referred to as RACQITO (resource availability continuous quality improvement trade-off),42 a concept derived from speed-accuracy tradeoffs described in industrial settings. Although at first one might think that violations of organizational policies, rules, and procedures would always be causes of failures and adverse events, the modern approach to safety has pointed out that some violations are actually necessary for the safe functioning of the system, and others fall somewhere in between.43 Aside from recklessness, drug use on the job, moral failings, and other egregious acts, research in other domains has identified other factors that are associated with the occurrence of rule and safety violations (Box 197-1). The “normalization of deviance”44 is an accumulated tolerance of small variances from safe operating conditions that develops over time, ultimately compromising safety. This is evidenced in overtaxed EDs coping with overcrowding of patients (e.g., performing evaluation and management of patients in hallways). Violations can also occur in response to perceptions of authority. They may occur through a directive supporting violation from an authority figure (e.g., nursing supervisors order admitted patients moved to inpatient beds without calling to report if there are delays in reaching inpatient nurses), the absence of a disapproving authority (e.g., physicians leaving shifts early and the medical director does not address the behavior), or an individual’s self-perception that he or she is authorized to disregard or to deviate from prescribed procedures (e.g., ED electrocardiograms done on patients in chairs because there are no available stretchers). Fluctuations in mood can also contribute to violations for a variety of reasons and will result in inconsistent clinical performance; men are more likely to break safety rules and to engage in more risk-taking behavior than women are.43 Risk-seeking and risk-averse attitudes are associated aspects of decision-making in the ED.45 Good teamwork is essential to the safe practice of emergency medicine, but emergency caregivers are not trained or evaluated as teams. Teamwork training in other fields, such as aviation, has been successful in reducing failures related to poor communication, cross-monitoring (observing others’ behaviors to reduce risk of failure and share workload), and authority gradients (both within and between professions).46 Work on transferring teamwork training principles to emergency medicine suggested that teamwork failures are involved in approximately 40% of malpractice cases.47 The lack of cross-monitoring across team members and the failure of advocacy or assertion on behalf of the patient by caregivers to avoid patient harm were two of the factors most frequently identified. A multidisciplinary teamwork training course implemented in nine EDs showed a significant improvement in quality of team behaviors and a sixfold decrease in observed clinical errors.14 Teamwork is not a specific fix for any one type of error, but it should be viewed as one type of adaptable human factor intervention with a set of teachable skills and behaviors capable of increasing system resilience and safety, which are hallmarks of high-reliability organizations.48 Teamwork training requires a change of culture, which can be difficult for ED staff. Institutional and ED leadership must be fully committed to the process before implementation of teamwork training for all staff. Resistance to behavioral change is likely to be encountered, and it will be necessary to demonstrate the clinical relevance of this training. High-fidelity medical simulation supported by audiovisual feedback offers the educational methodology to help clinicians and staff understand the necessity of behavioral change.49 A major unanswered question is how to embed teamwork behaviors into medical training and how to sustain the behaviors over time. Almost all human groups have some form of authority gradient among members. This hierarchy can be based on profession (e.g., physicians have greater authority than nurses) or organizational rank (e.g., attending physicians have more authority than residents). Ideally, information between team members should flow freely, but this may not occur if low-authority members are inhibited by differences in seniority, stature, expertise, profession, or social status. There are clear examples of cases in which authority gradients have been responsible for adverse events.50 A work environment in which all team members feel comfortable expressing their viewpoint, especially if it is a dissenting one, requires cultural change that can begin with the physicians who occupy the highest authority position in the clinical setting. Authority figures have the ability to initiate change by recognizing the value of perspectives other than their own and eliciting them from other clinicians and staff (e.g., asking a patient’s nurse what he or she thinks may be going on with the patient). Senior clinicians are in a powerful position to bridge gradients by fostering open communication through multidisciplinary rounds, demonstrating that they are approachable (e.g., acknowledging staff by name), and using clinical narratives from their own experience that illustrate near misses and judgment failures.51
Process Improvement and Patient Safety
Perspective
Sources of Failure in Emergency Care
Emergency Department Design, Human Factors, and Ergonomics
Overcrowding
Information Gaps
Performance-Shaping Factors
Violation-Producing Factors
Teamwork
Authority Gradients

Full access? Get Clinical Tree