Preterm Labor | 14 |
Defined as a delivery that occurs prior to 37 weeks gestation, preterm birth is the leading cause of perinatal mortality and long-term infant morbidity worldwide (Frey & Klebanoff, 2016). According to the National Center for Health Statistics, the preliminary preterm birth rate in the United States for 2015 was 9.62% (Hamilton, Martin, & Osterman, 2016). Although this represents a small percent rise from 2014 (9.57%), the preterm birth rate in the United States has been steadily decreasing since 2006 when the rate peaked at 12.8% (Hamilton et al., 2016). Despite these trends, the preterm birth rate in the United States remains one of the highest among industrialized nations (Frey & Klebanoff, 2016). Although advances in perinatal and neonatal medicine have improved the survival rates for these infants, the consequences of prematurity still pose lifelong disability and economic burden (Frey & Klebanoff, 2016). Preterm births are classified as either spontaneous (i.e., premature rupture of membranes or preterm labor with cervical dilatation) or indicated (i.e., induction of labor for maternal or fetal complications). Preterm births are also categorized by gestational age at delivery. For example, preterm births occurring between 34 and 36 weeks are referred to as late preterm births (Hamilton et al., 2016). This chapter will present the diagnosis and management of spontaneous preterm labor in singleton pregnancies occurring between 24 and 34 weeks gestation.
PRESENTING SYMPTOMATOLOGY
Etiology and Risk Factors
Regular and painful uterine contractions that result in cervical change have been the long-accepted definition of labor. Until recently, this “common pathway of parturition” was thought to occur similarly in both full-term and preterm labor (Romero, Dey, & Fisher, 2014). Unlike labor at full-term gestations, however, spontaneous preterm labor is an enigmatic process that occurs when the normal labor pathway is triggered through various pathologic mechanisms. Intrauterine infection or inflammation, immunologic reactions, hormonal disorders, cervical insufficiency, and uterine ischemia, hemorrhage, or overdistention have all been implicated as associated factors in preterm labor (Romero et al., 2014). More recently, specific genetic and genome pathways have been linked to birth 148timing, providing opportunities for future research aimed at understanding the mechanisms of preterm parturition (Monangi, Brockway, House, Zhang, & Muglia, 2015).
A number of contributing factors have been identified that increase a woman’s chances of giving birth before 37 weeks. This comprehensive list represents years of epidemiologic investigation that has yet to establish a clear chain of causality with the sole exception of intra-amniotic infection (Romero et al., 2014). In addition, strategies to identify and treat medical risk factors during pregnancy have not reduced the preterm birth rate (Iams, 2014). A history of prior preterm birth or a short cervical length (measured by transvaginal ultrasonography) of less than or equal to 20 mm remain the most significant risk factors for preterm delivery (Iams, 2014). A summary of preterm birth risk factors can be found in Exhibit 14.1.
EXHIBIT 14.1
Risk Factors Associated With Spontaneous Preterm Birth
Major Risk Factors
• Previous preterm birtha
• Non-White raceb
• Infection/inflammationc
• Cervical insufficiencyd
• Multiple gestation
• Bleeding in second trimester
• Mullerian uterine anomalies
Associated Risk Factors
• Low socioeconomic status
• Maternal age less than 18 or greater than 40
• Limited maternal education
• Unmarried
• Poor nutrition/underweight
• Short interconception period (<6 months)
• Smoker
• Drug abuse
• Life stressors
• Occupational fatigue
• Family history of preterm birth
• Periodontal disease
• Sexually transmitted infections
• Shifts in vaginal ecosystem
aInduced or spontaneous.
bBlack, African American, Afro Caribbean.
cChorioamnionitis or systemic infections (pneumonia, pyelonephritis, appendicitis).
dShortened cervix less than or equal to 2.5 mm on transvaginal ultrasound in second trimester.
Source: Adapted from Goldenberg, Culhane, Iams, and Romero (2008).
149HISTORY AND DATA COLLECTION
Subjective Assessment
Women with threatened preterm labor often present with a myriad of nonspecific symptoms such as constant low backache, pelvic pressure, mild irregular uterine cramping, and increased watery vaginal discharge. While the majority of women admitted to the hospital for treatment of threatened preterm birth will go on to deliver at full-term gestations, any persistent abdominal, pelvic, or vaginal symptoms warrant a full obstetric evaluation to rule out preterm labor.
The diagnosis of true preterm labor can be challenging to determine clinically. Regular, painful contractions with a progressive change in cervical effacement and/or dilatation or cervical dilatation of at least 2 cm are reliable clinical indicators (American College of Obstetricians & Gynecologists [ACOG], 2016b). The presence of any vaginal bleeding or premature rupture of membranes greatly adds to the likelihood of impending birth. More importantly, the transition from subclinical parturition to overt preterm labor has been most likely triggered by one or more pathologic processes (Romero et al., 2014). Consequently, the presence of past or current risk factors for preterm birth is important to ascertain, as well as any recent associated symptoms such as fever, malaise, nausea, vomiting, diarrhea, urine symptoms, drug use, and trauma. Previous cervical assessments (digital or ultrasound) or recent sexual intercourse are also noted.
Gestational Age Assessment
A crucial next step in data collection is a thorough review of the dating criteria used to determine gestational age. Women who conceive with assisted reproductive technologies will have the most accurate pregnancy dating, followed by first trimester ultrasound assessment (Benson & Doubilet, 2016). Menstrual dating is still considered to be reliable, especially when corroborated by an ultrasound performed prior to 20 weeks gestation (Benson & Doubilet, 2016). Accuracy of fetal biometry ultrasound decreases with advancing gestational age. Consequently, women who present for care in the third trimester with an unsure menstrual history could potentially have a margin of error with ultrasound dating of anywhere from 21 to 30 days (ACOG, 2014; Benson & Doubilet, 2016). No matter how the gestational age was determined, some margin of error exists and clinicians must use the best evidence-based criteria to discern the boundaries for preterm labor treatment.
PHYSICAL EXAMINATION
Pregnant women with a gestational age of greater than 24 weeks who present with any symptoms suggestive of preterm labor require continuous external fetal monitoring for contractions and assessment of fetal well-being. Observation of the woman’s demeanor and response to contractions is ongoing while the remainder of the physical examination is completed. Constitutional assessment includes temperature, pulse, respirations, and blood pressure, paying careful attention for the presence of any fever, tachycardia, or tachypnea. Auscultation of the heart and lungs is performed, as well as thorough palpation of the abdomen and uterine fundus for any signs of tenderness, rebound, or guarding. Percussion of the flank area for costovertebral angle tenderness is another requisite component of this evaluation to assess for signs of renal etiologies.
150Lastly, a complete pelvic exam is performed. It is imperative that a digital examination is not performed until the vagina and cervix are first visually inspected using a sterile speculum. This enables the clinician to initially exclude the possibility of preterm premature rupture of membranes (PPROM) and obtain any necessary specimens for further evaluation. Cervical dilation, bleeding, or discharge can also be assessed during this inspection. Regardless of the appearance of the cervix, once PPROM is ruled out and the possibility of placenta previa is also excluded, a digital examination can be safely performed to more thoroughly assess cervical dilatation, effacement, consistency, and position.
LABORATORY AND IMAGING STUDIES
Since there are a number of pathologic processes that could lead to preterm labor, the physical examination must be accompanied by laboratory studies that will facilitate accurate diagnosis of etiologies such as intrauterine and extrauterine infections. A complete blood count and clean catch urinalysis (with micro) are basic first steps of this evaluation. During the pelvic examination, cultures for gonorrhea, chlamydia, and a vaginal swab for wet mount assessment are collected. Specifically, a wet mount is obtained to identify the presence of either bacterial vaginosis or trichomoniasis. These infections have been implicated as risk factors for preterm labor, especially in women with a history of preterm birth, although absolute causality has not been established (Koullali, Oudijk, Nijman, Mol, & Pajkrt, 2016).
Fetal Fibronectin
Fetal fibronectin (fFN) is an extracellular glycoprotein normally found in the amniochorionic membrane prior to 20 weeks gestation and again as labor approaches in full-term gestations due to physiologic cervical remodeling and effacement (Berghella & Saccone, 2016). For women presenting with threatened preterm labor between 24 and 34 weeks gestation, the presence or absence of fFN was thought to hold some predictive value in determining the risk of delivery within 7 days. The fFN sample must be collected prior to any other vaginal or cervical examination and its validity is greatly hampered by the presence of lubricants, bleeding, amniotic fluid, and sexual intercourse within 24 hours (Wax, Cartin, & Pinette, 2010). Proper technique requires that the swab is placed in the posterior vaginal fornix (avoiding the cervical os) during the speculum examination but can also be inserted blindly into the vagina (Wax et al., 2010). In either case, the swab is left in position for a minimum of 10 seconds and placed in the appropriate culture medium according to the manufacturer’s instructions. The specimen can then be set aside and either sent or discarded as the clinical situation dictates.
Previous evidence on the clinical utility of fFN testing in threatened preterm labor has demonstrated a negative predictive value of almost 98%, providing reassurance that delivery is unlikely within the next 7 days (Sanchez-Ramos, Delke, Zamora, & Kaunitz, 2009). The positive predictive value of fFN unfortunately is only 25.9%, often leading to overtreatment and increased costs (Sanchez-Ramos et al., 2009). In a more recent systematic review, Berghella and Saccone (2016) state fFN testing has not been found to improve outcomes or decrease the incidence of preterm birth and should not be used routinely in the management of women with threatened preterm labor. They further conclude fFN is best utilized in screening protocols that include transvaginal ultrasound measurement of cervical length (Berghella & Saccone, 2016).
151Cervical Length Assessment
Initially, real-time abdominal ultrasound is performed to confirm the presenting part, identify placental location, or gauge an approximate gestational age, if needed. Ultrasound can also be utilized to provide a transvaginal measurement of cervical length (TVCL). When compared to digital assessments performed in early labor, transvaginal cervical sonography imparts a more consistent and objective measurement of the cervix (Nijman, van Vliet, Koullali, Mol, & Oudijk, 2016). Moreover, decreasing TVCL has been associated with increased risks of spontaneous preterm birth (Nijman et al., 2016). As a screening tool in selected asymptomatic high-risk women (those with a history of prior preterm birth), a second trimester TVCL measurement of 25 mm is considered the threshold discriminator for predicting future recurrence risk of preterm delivery and may indicate cervical insufficiency (Iams, 2014).
For women presenting with preterm contractions at 24 weeks or beyond, a TVCL measurement can distinguish a low (less than 5%) versus high probability of preterm delivery (Nijman et al., 2016). For example, a TVCL of 30 mm or greater precludes the likelihood of preterm birth within the next 7 days (Nijman et al., 2016; Van Baaren et al., 2014). The addition of an fFN culture further stratifies the risk category when the TVCL is between 15 to 30 mm. Symptomatic women with a TVCL of less than 15 mm or 15 to 30 mm with a positive fFN are at high risk to deliver within the next week and require prompt treatment (Nijman et al., 2016). Conversely, when combined with a negative fFN, a normal TVCL measurement can greatly reduce false positive diagnoses and provide a more cost-effective alternative to hospital admission (Nijman et al., 2016; Van Baaren et al., 2014). As a result, many hospitals have now incorporated protocols that include a combination of both TVCL and fFN in efforts to more accurately discriminate those women truly at high risk for delivery (Nijman et al., 2016; Van Baaren et al., 2014).
Mid trimester ultrasound can also assess other characteristics of the lower uterine segment and cervix that may provide additional risk stratification for the likelihood of a preterm delivery. Cervical funneling, for example, is a term used to describe a measurable opening of the internal os and has been associated with cervical insufficiency (Mella & Berghella, 2009). Protrusion of the amniotic membrane into the inner cervical canal can have a “V” or “U” shaped appearance (Mancuso et al., 2010). In the presence of a shortened cervix, a “U” shaped funnel in particular is an ominous sign and the risk of preterm birth is greatly increased (Berghella et al., 2007; Mancuso et al., 2010). See Figure 14.1 for a transvaginal measurement of shortened TVCL with funneling.
DIFFERENTIAL DIAGNOSIS
Women experiencing the wide array of symptoms associated with threatened spontaneous preterm labor will generate a broad list of differential diagnoses. This inventory includes fairly straightforward etiologies such as Braxton Hicks contractions and round ligament pain. More serious causes such as pyelonephritis or chorioamnionitis must be conclusively ruled out. Regardless of the presumed cause(s), overt preterm labor calls for expeditious treatment, especially in cases where birth seems imminent. A comprehensive list of differential diagnoses is noted in Exhibit 14.2.
152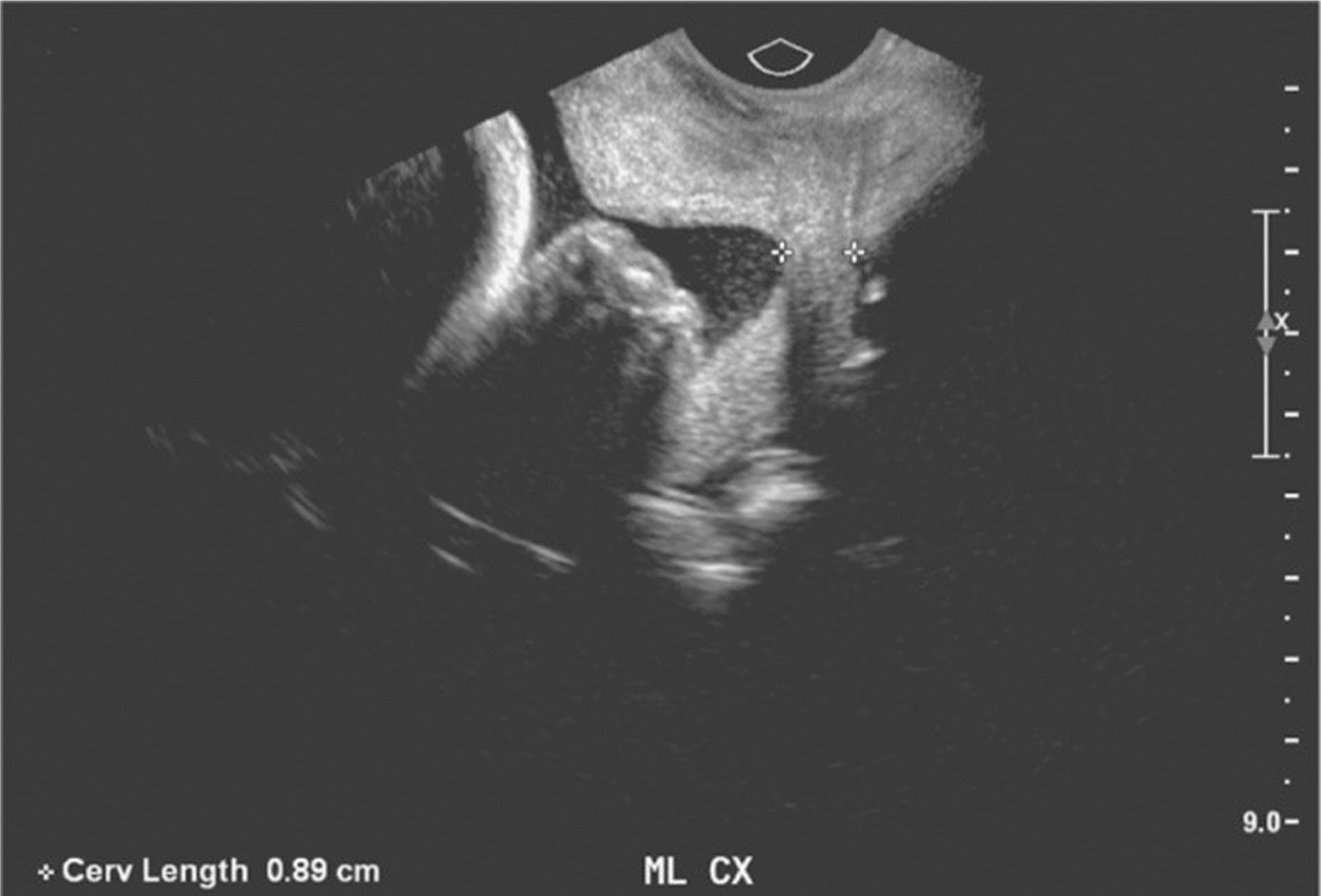
Figure 14.1 Sonographic image of shortened cervix with funneling
Source: Courtesy of Department of Radiology, Women & Infants Hospital, Providence, RI.

Full access? Get Clinical Tree








