Jonathan Thompson Simon Young The chapter will describe: • the importance of a detailed medication history • common therapeutic treatments for systemic disease and implications for preoperative optimisation. • the increasing use of herbal and illicit drugs and implications for perioperative care. It is important to take a detailed drug history from all patients undergoing surgery. This includes details of prescribed drugs, non-prescription medicines (for example, herbal remedies), and drugs of addiction and abuse. In general most chronic medications can be continued throughout the perioperative period, though there are some important exceptions which are detailed in this chapter. Perioperative medication may be prescribed for several reasons: • the management of co-existing medical conditions unrelated to the surgery • the medical management of surgical conditions • premedication • anaesthetic agents (general, regional, and local) and analgesics • organ support in critically ill patients • drugs administered de novo in an attempt to improve outcome. Alteration of drug therapy to optimise chronic medical conditions and the judicious use of certain additional drugs may help avoid some of the complications of surgery and anaesthesia, as well as improve patient satisfaction. In addition other factors are relevant to drug therapy in the perioperative period, including: • fasting before surgery and altered gastrointestinal function • the effects of surgery and anaesthesia on co-existing illnesses • the effects of anaesthesia and surgery on drug action, metabolism and elimination. When planning drug therapy for surgical patients, a number of specific decisions should be made: • whether to continue a drug (the usual course of action) • whether to discontinue a drug, and for how long before surgery • whether to replace one drug and/or route of administration with another • whether to prescribe additional drugs that will improve patient outcome, comfort or satisfaction • when to restart a drug following surgery (in most cases, immediately). Some of the most commonly used ‘premedications’ in anaesthetic practice are anxiolytics, analgesics and gastric acid suppression medication. Pre-emptive anti-emetic drugs may also be considered in those at high risk. Asthma and chronic obstructive pulmonary disease (COPD) are the chronic respiratory diseases most commonly encountered in surgical patients. General anaesthesia, pain that reduces vital capacity and the ability to cough, and surgery per se all cause worsening of respiratory function. This may be compounded by the effects of analgesic medication, e.g. respiratory depressants (opiates) or drugs which may exacerbate bronchospasm, e.g. non-steroidal anti-inflammatory drugs (NSAIDs). Postoperative respiratory tract infection may supervene and impair respiratory function further. It is therefore important that respiratory function is optimised before surgery and perioperative management of the respiratory system has two main aims: • treatment of acute deteriorations, and possible postponement of elective surgery until treatment is effective • assessment and optimisation of chronic respiratory disease. In general, all regular respiratory medications should be continued and with inhaled drugs this is usually straightforward. In addition regular nebulised beta2-agonists and anticholinergics can be usefully administered for a number of days before surgery, as well as being administered immediately before the operation, and in the postoperative recovery room (Table 12.1). Patients with severe airways disease may benefit from a preoperative course of double dose inhaled steroids or daily prednisolone (20–40mg) for seven days. Table 12.1 Bronchodilator pharmacology
Chapter 12 Preoperative pharmacological optimisation
SUMMARY
INTRODUCTION
Concurrent medication
Drugs acting on the respiratory system
| Dose | Timing | |
| Beta2-agonists | ||
| Salbutamol | 2.5–5mg neb | Every 15 mins as required |
| Terbutaline | 0.5mg neb | Every 15 mins as required |
| Anti-muscarinic | ||
| Ipratropium bromide | 0.5mg neb | 6 hourly |
| Non-specific phosphodiesterase inhibitor | ||
| Aminophylline | 0.5mg/kg/hr | Substitute for theophylline |
Patients who have severe airways disease may also be receiving drugs such as theophylline or leukotriene receptor antagonists (e.g. montelukast, zafirlukast). Again, every attempt should be made to ensure uninterrupted perioperative administration of these drugs. Intravenous aminophylline may be used as a substitute for oral theophylline (Table 12.1) in patients unable to take tablets; drug monitoring of plasma concentrations (therapeutic range 10–20µg ml-1) is strongly suggested.
Drugs acting on the cardiovascular system
Cardiovascular disease is common in patients presenting for surgery. Many drugs that surgical patients receive will have effects on the cardiovascular system, either as a direct therapeutic aim or as a side effect. Perioperative cardiovascular morbidity (e.g. acute myocardial infarction) is uncommon, but carries a high risk of death, and may be decreased by certain therapies. Management of cardiovascular drugs covers two areas:
• optimisation of chronic disease
• specific drugs to reduce perioperative cardiovascular morbidity.
Beta-adrenoceptor antagonists (‘beta-blockers’)
Beta-blockers are commonly used in the treatment of patients with a variety of conditions including hypertension, ischaemic heart disease, cardiac dysrhythmias, congestive cardiac failure, hyperthyroidism and anxiety. Abrupt discontinuation of beta-blockers in the perioperative period can lead to rebound hypertension and tachydysrhythmias, and has been associated with perioperative cardiovascular morbidity. Exaggerated responses to anaesthetic and surgical stimuli often occur if beta-blockers have been withheld. Every effort should therefore be made to continue beta-blockers, using intravenous preparations if the oral route is not available. For example a patient normally receiving oral atenolol 25–100mg once daily could be switched to atenolol 2.5–10mg IV (administered cautiously by slow injection) once daily. Longer-acting blockers (e.g. atenolol) may confer more benefit than shorter-acting drugs (e.g. metoprolol, propranolol) in reducing perioperative cardiovascular morbidity, as the effects of mistimed or omitted doses are lessened.1,2
Renin angiotensin system modifying drugs
Angiotensin converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs) are used in the management of hypertension, ischaemic heart disease, congestive cardiac failure and renal protection in diabetes mellitus. They can be associated with profound hypotension in the perioperative period, which can be unresponsive to vasoactive drugs. Various patient and anaesthetic factors can influence the degree of hypotension. The decision to continue or discontinue ACEI/ARB should therefore be made on an individual patient basis (Table 12.2). If these drugs are to be stopped this should be considered at least 24 hours before surgery. A new class of drug has recently become available – the direct renin inhibitors (DRI), e.g. aliskiren. The therapeutic and adverse effects of these drugs are most likely similar to the ACEIs/ARBs, and until more data are available they should be treated in the same way.
Table 12.2 Considerations regarding perioperative ACEIs and ARBs
Consider continuation Critical left ventricular function Anti-hypertensive monotherapy |
Consider discontinuation Planned central neuraxial block: • particularly if using thoracic epidural analgesia (particularly a high thoracic epidural placement) • particularly if combined with general anaesthesia Anticipated large perioperative fluid shifts (major gastrointestinal, orthopaedic, thoracic surgery) Combined ACEI and ARB therapy – consider stopping at least one High risk of acute renal failure in the perioperative period Orthostatic hypotension |
Anticoagulation
Anticoagulants are used for the prevention of clotting in various situations:
• patients with prosthetic valves, vessels or stents
• patients with atrial fibrillation (AF) or dyskinetic ventricular segments (to prevent arterial embolic events, particularly stroke)
• patients at risk of, or suffering from venous embolic events, i.e. deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE).
Therapeutic anticoagulation increases surgical bleeding but the risks of this should be balanced against the risks of thrombotic events if anticoagulant therapy is discontinued. Thus it is important to understand the indications for anticoagulation, the problems it can cause, and the alternatives available. Warfarin (oral route) and the heparins (subcutaneous or intravenous routes) are the most commonly encountered anticoagulants in the UK. A detailed discussion of this topic is covered in Chapter 10, pages 202–16.
Anti-platelet drugs
Anti-platelet drugs (aspirin, dipyridamole, clopidogrel) are widely prescribed for the prevention and treatment of ischaemic heart, cerebrovascular and peripheral vascular diseases. They are associated with a slight increase in surgical bleeding but in most cases this is minor and should be balanced against the increased risks of thrombotic events if anti-platelet therapy is discontinued. In most cases therefore treatment can be continued in the perioperative period. Spinal or epidural catheter placement is considered to be safe in patients receiving low-dose aspirin or dipyridamole therapy. However in some high-risk situations, for example intracranial and vitreo-retinal surgery, the increased risks of surgical bleeding outweigh the potential antithrombotic benefits and in these situations anti-platelet drugs should be stopped.3 The effects of aspirin on platelet function are irreversible, and so if aspirin is to be stopped before surgery a period of seven days should be allowed before sufficient platelets are regenerated.
Clopidogrel is a highly potent anti-platelet drug. Its action is also irreversible and if it is to be stopped this should be done at least seven days before planned surgery or spinal/epidural anaesthesia.4 Recent developments in cardiology have included the widespread introduction of intravascular stenting for coronary artery disease. In the early weeks and months after stent placement the patient is at increased risk of potentially fatal stent thrombosis,5,6 and it is recommended that clopidogrel is continued for one year after placement of a drug-eluting stent.7 Clearly some of these patients will present for surgery within this time. If surgery cannot be postponed, most patients with recent coronary artery stents would benefit from continuing their dual anti-platelet therapy perioperatively, accepting that surgical blood loss will be increased, and that epidural or spinal anaesthesia should be avoided.8 This approach may be inappropriate in situations where bleeding could be catastrophic (neurosurgery, vitreo-retinal surgery, major cardiac or hepatic surgery) in which case clopidogrel therapy may be stopped but aspirin continued.
Anti-dysrhythmic drugs
Cardiac output may be compromised by tachycardia (heart rate > 90bpm) and uncoordinated cardiac contractions (e.g. atrial fibrillation or other cardiac dysrhythmias). Anaesthesia and surgery can predispose patients to new dysrhythmias, or pre-existing benign dysrhythmias may develop into malignant dysrhythmias. Mechanisms involved include perioperative electrolyte imbalances, autonomic reflexes, or the administration of certain drugs used during anaesthesia. It is therefore very important to continue any rate-controlling drugs (e.g. digoxin, beta-blockers) and rhythm-controlling drugs (e.g. amiodarone, flecainide) in the perioperative period. In patients unable to absorb oral medication intravenous preparations of these drugs are available. In patients receiving digoxin for atrial fibulation, poor heart rate control, major surgery and critical illness would be indications for therapeutic drug monitoring of serum digoxin concentrations (usual range 1.0–2.5nmol l-1 or 0.5–2.0ng ml-1). Optimisation of serum potassium and magnesium levels is also important. Anxiolytic premedication (e.g. benzodiazepines) may also be helpful.
Diuretics
Many patients receive diuretic medication for the management of hypertension and fluid retention, caused by congestive heart failure or chronic kidney disease. If continued during the perioperative period these can cause electrolyte disturbance and dehydration. However, withholding diuretics may worsen congestive heart failure. The decision as to whether to continue with diuretics is complex, but if large fluid and electrolyte shifts are expected (e.g. major bowel surgery) it may be prudent to withhold them.
Nitrates
Nitrates are used for symptom control in angina pectoris. Abrupt discontinuation of nitrates is unwise and additional nitrates may be useful if angina is associated with preoperative anxiety. The patient’s own modified-release nitrate (e.g. isosorbide mononitrate) or a topical nitrate patch can be administered perioperatively. Topical nitrate patches are available (GTN in 5mg, 10mg and 15mg preparations) which deliver their dose over 24 hours. Anxiolytic premedication can also help reduce symptoms of angina.
Calcium channel blockers
Calcium channel blockers (CCBs) are primarily used to treat hypertension, angina pectoris and tachydysrhythmias. Sudden withdrawal of CCBs may be associated with exacerbations of angina and it is therefore prudent to continue these drugs during the perioperative period.
Drugs used for hypertension
Chronic hypertension is a sustained increase in blood pressure over 140/90mmHg,9 as measured in the clinic or general practice setting. The British Hypertension Society guidelines9 suggest drug treatment for the following patients:
• Stage I hypertension (SBP 140–159 or DBP 90–99) if associated with organ damage, or in the elderly
• Stage II hypertension (SBP ≥ 160 or DBP ≥ 100).
Although uncontrolled hypertension has traditionally been viewed as a reason to cancel elective surgery, recent data suggest that some of the risks may have been over-emphasised.10,11 Patients with severe hypertension are at increased risk of perioperative swings in blood pressure, dysrhythmias and myocardial ischaemia and specific additional interventions or monitoring may be required. However, there is limited evidence to prove that postponing surgery in order to control blood pressure improves overall outcome.11 Nonetheless every effort should be made to optimise blood pressure in elective patients prior to surgery. Eight weeks is ideally required to allow stabilisation on a particular anti-hypertensive agent. Blood pressure control should be complemented by assessment of overall cardiovascular risk, with consideration given to starting anti-platelet and statin therapy as well.
Reducing perioperative cardiovascular morbidity in non-cardiac surgery
There has been much interest recently in using beta-blockers to reduce cardiovascular complications and mortality in patients undergoing major surgery. Recent guidelines12 recommend that patients scheduled for major vascular surgery, and who have inducible myocardial ischaemia on cardiac stress testing, should receive beta-blockers before and after surgery (Table 12.3). Beta-blockers should also be considered in patients with documented coronary artery disease or multiple cardiac risk factors undergoing other high-risk surgery, though the evidence in these groups is less conclusive. There is an increased risk of perioperative bradycardia and hypotension requiring treatment in the beta-blocked patient.13
Table 12.3 Beta-blocker therapy recommendations12
• Start several days or weeks before surgery if possible. • Aim for a resting preoperative heart rate of 50–60bpm, and an intraoperative and postoperative heart rate of less than 80bpm. • Use cardioselective (beta1-antagonists) agents, e.g. atenolol, metoprolol, esmolol. • Every effort should be made to continue beta-blockade uninterrupted throughout the perioperative period. • Use long-acting agents where possible, to minimise rebound effects, if administration is interrupted.2 |
There is growing evidence that patients undergoing major vascular surgery benefit from long-term statin (HMG-CoA reductase inhibitor) therapy (e.g. simvastatin 20–40mg daily), starting as early as possible before surgery,14,15 and continuing for life. Even in patients having non-vascular surgery, statin therapy may reduce perioperative cardiac morbidity. Certainly statins should not be withdrawn in patients already taking them, and they should be re-introduced as soon as possible postoperatively.15
Endocrine system
Diabetes mellitus
Diabetes mellitus (DM) can be broadly classified as Type 1 (insulin-dependent) DM and Type 2 DM (diet-controlled, tablet-controlled, or insulin-requiring). Tight control of blood glucose concentrations can improve wound healing and reduce morbidity and mortality.16 Guidelines vary but a target blood glucose concentration of less than 10mmol l-1 provides a compromise between practical glycaemic control and avoidance of dangerous hypoglycaemia.17
Oral hypoglycaemic agents either promote the release of insulin, or improve its action in the peripheral tissues. They can be safely omitted on the day of surgery, although stopping Metformin may require specialized advice before surgery or in the critically ill. Some patients with Type 2 DM who do not normally require insulin may need to be given insulin perioperatively, and patients who usually receive subcutaneous insulin may need ‘tighter’ glycaemic control through the use of intravenous insulin. Most hospitals have guidelines in place for the perioperative management of patients with diabetes.
Corticosteroid supplementation
The need for steroid replacement or supplementation is determined by the dose of steroid taken regularly, the extent of surgery, and the duration of perioperative fasting. Patients regularly using lower dose inhaled steroids do not require additional steroid replacement. If high inhaled doses are being taken, perioperative steroid supplementation should also be considered (Table 12.4).18
Table 12.4 Perioperative corticosteroid supplementation guidelines18
| Prednisolone | Surgery | Additional steroid cover |
| ? 10mg d-1 | Usually not needed | |
| > 10mg d-1 | All | 25mg hydrocortisone IV at induction |
| Plus postoperative dosing as follows: | ||
| Minor | No postoperative steroids | |
| Intermediate | Hydrocortisone 100mg d-1 IV for 24 hrs | |
| Major | Hydrocortisone 100mg d-1 IV for 48–72 hrs | |
| ‘High’ daily doses of inhaled corticosteroids for asthma and COPD26 | |
| Fluticasone propionate | 400 micrograms or over |
| Beclometasone dipropionate | 800 micrograms or over |
| Budesonide | 800 micrograms or over |
Notes:
If patient stopped chronic steroids less than three months ago, treat as if still on steroids. Postoperative hydrocortisone should ideally be administered as a constant infusion to minimise swings in blood glucose concentrations; alternatively hydrocortisone 25mg IV qds can be given.
Thyroid disorders and the perioperative period
Patients with thyroid disease should be clinically euthyroid (i.e. displaying neither symptoms nor signs of hyper- or hypothyroidism) and free from any adverse effects of thyroid medication. Thyroid over-activity can cause tachycardias and a hypermetabolic state (a thyroid ‘storm’), whereas under-activity can lead to bradycardia, hypotension and prolonged recovery. In emergency situations the effects of hyperthyroidism can be attenuated by administration of beta-blockers, potassium iodide and carbimazole. Thyroxine is available as an intravenous preparation, liothyronine, but is seldom needed as patients can usually safely omit thyroxine for a number of days. The exception is the critically ill patient who requires thyroxine to aid recovery. The dose of intravenous liothyronine is one-fifth that of oral levothyroxine, i.e. 10–40micrograms.
Neuro-psychiatric disorders
Anti-epileptic medication
Anti-epileptic medication should be continued throughout the perioperative period to reduce the risks of seizures. Particular attention should be paid to the formulations of anti-epileptic drugs. Many are available in modified release formulations, which should not be interchanged with the standard release formulations. Some (e.g. phenytoin and sodium valproate) can be administered by intravenous infusion if gastrointestinal absorption is impaired. Changing to alternative routes of administration or alternative medications should only be undertaken with specialist advice, as interactions between these drugs are complex and toxicity common.
Anti-Parkinsonian medication
Anti-Parkinsonian drugs should be continued regularly (via gastric or jejunal tube if necessary), to ensure avoidance of distressing dyskinesis. In exceptional circumstances a subcutaneous infusion of apomorphine, a short-acting dopamine agonist, may be used during waking hours as a temporary replacement of normal oral therapy.19,20 Newly available transdermal patch formulations (e.g. rotigotine, a dopamine agonist) may provide an alternative route of administration. Expert advice should be sought when changing formulations.
Anti-depressants, anti-psychotics and anxiolytics
Most drugs in these categories should be continued in the perioperative period. The possible exceptions to this are the mono-amine oxidase inhibitors (MAOI) and lithium. MAOI may interact unpredictably with some anaesthetic drugs and for this reason some authorities recommend their discontinuation two weeks before surgery. However, these drugs are usually prescribed for severe depressive illness and discontinuation may have serious repercussions; continuation is sometimes the best course of action. Lithium should be stopped 24 hours before major surgery as electrolyte derangements can occur, but can be continued for minor surgery.
Inflammatory conditions and immunosuppressants
In general, conditions with inflammatory components (e.g. inflammatory bowel diseases, arthritis, skin conditions) can worsen if medications are withheld. Immunosuppressants and corticosteroids are the agents most commonly used, and consideration should be given to switching to intravenous preparations if the enteral route will be unavailable for any length of time. In particular, in patients with a transplanted organ where immunosuppression is vital to the preservation of organ function, medication should not be interrupted.
Premedication
This section will deal with pharmacological management of the following perioperative concerns, which can be managed, at least in part, by medication:
• anxiety
• gastric acid suppression
• pre-emptive analgesia
• management of nausea and vomiting.
Anxiety management
Many patients are anxious about forthcoming anaesthesia and surgery. Common fears include pain, nausea and vomiting, awareness under anaesthesia, and even death. Often patients will be reluctant to voice their fears directly. Much patient anxiety can be allayed by explanation of the process of anaesthesia, analgesia, surgery and the postoperative course.
Despite reassurance, some people understandably remain anxious about forthcoming anaesthesia and surgery. Apart from the psychological upset caused by anxiety, physiological manifestations can be troublesome. Tachycardia, hypertension, hyperventilation, and gastrointestinal upset are all common in the anxious patient. Activation of the sympathetic nervous system (the ‘fight or flight’ response) can be harmful. For example, the patient who has chronic hypertension may develop dangerously high blood pressure, the patient with atrial fibrillation may become tachycardic, or the patient with angina may develop chest pain and shortness of breath. Anxiolytic or sedative medication can reduce both psychological stress and the associated pathophysiological effects.
The anxiolytic medications most commonly used in anaesthesia are the benzodiazepines, which also have sedative and amnesic effects. Benzodiazepines act by potentiating the action of the inhibitory neurotransmitter γ–amino-butyric acid (GABA) on neuronal GABAA receptors. Various different types of benzodiazepine are available (Table 12.5), and the choice of drug depends mainly on the duration of anxiolysis required.
The use of benzodiazepines can lead to prolonged sedation postoperatively. This may be undesirable in certain situations, such as day case or intracranial surgery. The metabolism of many benzodiazepines can also be significantly prolonged in the elderly, and the sedative effects can last for days, leading to postoperative delirium and somnolence. Repeated doses of benzodiazepines can lead to significant accumulation of these drugs.
When using these sedative drugs, particular thought should also be given to the potential for respiratory depression and hypoxaemia. Supplemental preoperative oxygen is indicated for any patient who may be at increased risk of respiratory depression, or when the higher doses of benzodiazepine are used. Flumazenil is a benzodiazepine antagonist that can be used in emergency situations where over-sedation has occurred.
Table 12.5. Oral benzodiazepines for premedication
| Drug | Dose | Before surgery | |
| Short-acting (30–60 mins) | Midazolam | 0.5mg kg-1 | 30 mins |
| Intermediate (2–4 hrs) | Temazepam Diazepam | 10–40mg 5–10mg | 30–60 mins 1–2 hrs |
| Long-acting (4–8 hrs) | Lorazepam | 1–4mg | 1–2 hrs |
Gastric acid suppression
In the perioperative period, gastrointestinal dysfunction and impairment of airway reflexes can increase the risk of inhaling gastric contents, leading to aspiration pneumonitis. Reduction of gastric fluid volume or acidity can lessen this risk. Drugs that suppress gastric acid fall into to two groups:
• drugs that reduce acid secretion by the gastric parietal cells
• drugs that neutralise acid already produced and present in the stomach.
Acid-secretion inhibitors are commonly used drugs with relatively few side effects. If a patient is already taking these drugs it is wise to carry on their normal prescription uninterrupted. In some institutions the H2-antagonist ranitidine (150mg PO or 50mg IV) is routinely prescribed the night before, and the morning of surgery.21 Other available acid-secretion inhibitors include the proton pump inhibitor (PPI) class of drugs (e.g. omeprazole 40mg PO or IV). In obstetric practice, the administration of sodium citrate (30ml 0.3m PO) is advocated immediately before general anaesthesia to neutralise residual stomach acid.
Pre-emptive analgesia
There is evidence that prevention of pain (by analgesics or local anaesthesia before surgery) can reduce both the stress response to surgery and postoperative pain. This is termed pre-emptive analgesia and can be used alone or as an adjunct to intraoperative analgesia. It often takes the form of simple oral analgesics, which can be given to the patient whilst awake prior to general anaesthesia. The type of analgesic considered depends on a number of factors:
• routes of administration available
• allergies to, or intolerance of, a particular drug
• perceived severity of pain to be encountered
• presence of co-morbid disease (respiratory, cardiac, renal, hepatic).
The continuation of analgesics already being taken by the patient is important, with further breakthrough analgesia being added to these medicines in the perioperative period. Wherever possible, chronic pain medications should be continued uninterrupted. Discontinuation can lead to extreme pain, anxiety and agitation. Chronic opiate therapy is a case in point – if unable to take oral medication, a continuous IV morphine background infusion (equivalent in rate to the 24-hour dose of opiate normally taken) can be prescribed, with a patient-controlled bolus for breakthrough pain postoperatively. Bolus doses of morphine for breakthrough pain may sometimes have to be increased dramatically in opioid-tolerant patients. Opioid patches (e.g. fentanyl and buprenorphine) may be continued as normal throughout the perioperative period, with breakthrough analgesia prescribed in addition to the patch. Absorption from patches may, however, be unpredictable if there are alterations in skin blood flow.
Opiate dependence, including prescribed methadone, can also lead to significant opiate tolerance, and vastly increased requirements for opiates should be anticipated. Methadone administration should be continued as usual, or replaced with parenteral opiate if the patient is unable to absorb orally. In patients who are recovering opiate addicts, it is advisable to clarify their feelings about the use of opiates in the perioperative periods, as they may wish to try and avoid them. It is often helpful to involve the hospital’s acute or chronic pain team in the management of opiate-dependent patients.
Anti-emetic medication
Postoperative nausea and vomiting (PONV) is common and unpleasant, and may cause significant psychological distress, physical damage and prolong hospitalisation. Risk factors for PONV are listed in Table 12.6.
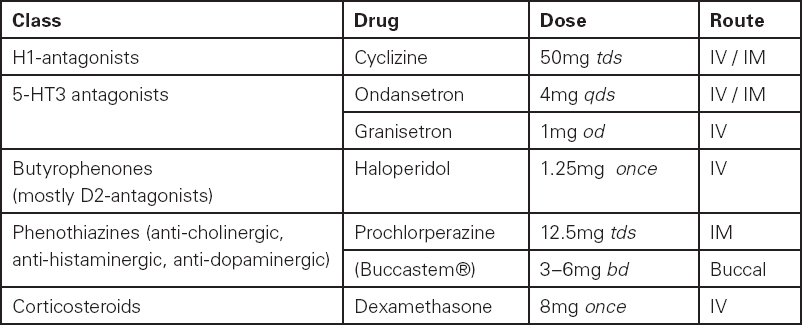
Low-risk patients do not require anti-emetic therapy unless they would suffer significant sequelae from vomiting as a result of the type of surgery they have undergone, for example, oesophageal surgery or jaw wiring. Monotherapy is indicated for patients with a moderate risk. A multi-modal approach (two or three agents) is of benefit in the prevention of PONV in high-risk patients.22 Various classes of drugs acting on different receptor systems can be utilised (Table 12.7). Pre-emptive anti-emetic therapy may have a role in patients at high risk of PONV. In addition certain patients may find non-pharmacological interventions for PONV (e.g. acupressure bracelets) helpful.
Table 12.6 Risk factors for postoperative nausea and vomiting
Patient factors Female Non-smoker History of PONV/motion sickness Children age 2 to puberty (increasing with age) |
Anaesthetic factors Intra- and postoperative opiate use Administration of volatile anaesthetic agents and nitrous oxide |
Surgical factors Prolonged surgery Type of surgery (laparoscopy/laparotomy, abdominoplasty, ENT, ophthalmic, neurosurgery, breast, plastic, gynaecological) |
Table 12.7 Anti-emetic medication
Substance dependence
Nicotine replacement
Patients should be strongly discouraged from smoking tobacco in the perioperative period, as it increases airway sensitivity, respiratory secretions, blood carbon monoxide levels, and decreases oxygen-carrying capacity. However, withdrawal from nicotine can cause anxiety and agitation in certain patients and nicotine replacement therapy may be useful. Options available include patches, gum, lozenges and nasal spray. Up to 80mg of nicotine can be administered in a 24-hour period.
Non-prescription drug use and abuse
Consumption of non-prescription substances (e.g. alcohol or tobacco, cannabis, cocaine, ecstasy) can cause a number of problems in the perioperative period. Issues arise with both acute intake and intoxication with these substances, and with long-standing repeated use.
Acute intoxication with alcohol or psychoactive drugs is a contra-indication to surgery unless the condition is immediately life- or limb-threatening because of the risks of airway compromise, pulmonary aspiration, respiratory depression, cardiovascular instability, altered consciousness and aggression, and disrupted body temperature control.
Chronic drug misuse, in particular excessive alcohol consumption, is common world-wide. Specific problems that may influence the perioperative course include:
• chronic lung disease caused by exposure to tobacco, cannabis and other inhaled substances
• vascular disease, cardiomyopathy, hypertension
• malnutrition, muscle wasting
• liver dysfunction
• increased or decreased tolerance to sedative medications
• psychiatric illness (depression, anxiety, psychoses) and neurological disease (e.g. peripheral neuropathy, cerebellar ataxia)
• acute withdrawal syndromes (best characterised by delirium tremens with alcohol withdrawal), agitation and aggression
• increased pain experience with tolerance to analgesics.
In the case of chronic alcohol misuse, the administration of vitamin supplements (oral thiamine and B12 Co-strong, or the intravenous vitamin preparation Pabrinex) is recommended in the perioperative period, starting as long as is feasible prior to major surgery.
Delirium tremens (DT) is a potentially fatal condition of physical and psychological withdrawal in patients with alcohol dependence syndrome. Table 12.8 reproduces a well-validated assessment tool (CIWA-Ar, the Clinical Institute Withdrawal Assessment Regime) for assessing the risk of developing DT, as well as stratifying the severity of DT. Pre-emptive use of benzodiazepine drugs (e.g. chlordiazepoxide or diazepam) is recommended for patients at risk of developing DT perioperatively, and many hospitals have their own guidelines in place.2
Table 12.8 Alcohol withdrawal assessment scale
| Nausea and vomiting Ask ‘Do you feel sick in the stomach? Have you vomited?’ Observation 0 No nausea and no vomiting 1 Mild nausea with no vomiting 2 3 4 Intermittent nausea, with dry retching 5 6 7 Constant nausea, frequent dry retching and vomiting | Tactile disturbances Ask ‘Have you any itching, pins and needles sensations, any burning. any numbness or do you feel bugs crawling on or under your skin?” Observation 0 None 1 Very mild itching, pins and needles, burning or numbness 2 Mild itching, pins and needles, burning or numbness 3 Moderate itching, pins and needles, burning or numbness 4 Moderately severe hallucinations 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations |
| Tremor Arms extended, elbows slightly flexed and fingers spread. Observation 0 No tremor 1 Not visible, but can be felt fingertip to fingertip 2 3 4 Moderate 5 6 7 Severe, even with arms not extended | Auditory disturbances Ask ‘Are you more aware of sounds around you? Are they harsh? Do they frighlen you? Are you hearing anything that is disturbing to you? Are you hearing things you know are not there?’ Observation 0 Not present 1 Very mild sensitivity 2 Mild sensitivity 3 Moderate sensitivity 4 Moderately severe hallucinations 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations |
| Paroxysmal sweats Observation 0 No sweat visible 1 2 3 4 Beads of sweat obvious on forehead 5 6 7 Drenching sweats | Visual disturbances Ask ‘Does the light appear to be too bright? Is its colour different? Does it hurt your eyes? Are you seeing things you know are not there?’ Observation 0 Not present 1 Very mild sensitivity 2 Mild sensitivity 3 Moderate sensitivity 4 Moderately severe hallucinations 5 Severe hallucinations 6 Extremely severe hallucinations 7 Continuous hallucinations |
| Anxiety Ask ‘Do you feel nervous?’ Observation 1 MiIdly anxious 2 3 4 Moderately anxious or guarded so anxiety is inferred 5 6 7 Equivalent to acute panic states as seen In severe delirium or acute schizophrenic reactions | Headache, fullness in the head Ask ‘Does your head feel different? Does it feel as though there is a band around your head?’ Do not rate for dizziness or light headedness. Otherwise rate severity. Observation 0 Not present 1 Very mild 2 Mild 3 Moderate 4 Moderately severe 5 Severe 6 Very severe 7 Extremely severe |
| Agitation Observation 0 Normal activity 1 Somewhat more than normal activity 2 3 4 Moderately fidgety and restless 5 7 Paces back and forth during most of the Interview or constantly thrashes about | Orientation and clouding of sensorium Ask ‘What day is this? Where are you? Who am I?’ Observation 0 Orientated and can do serial additions Ask person to perform serial addition of 3s up to 30, e.g. 3.6.9… 1 Cannot do serial addition or is uncertain about date 2 Disorientated for date by no more than 2 calendar days 3 Disorientated for date by more than 2 calendar days 4 Disorientated for place and/or person |

Full access? Get Clinical Tree





