Fig. 26.1
The Cierny classification of adult osteomyelitis
The osteomyelitis patient according to Cierny et al. can be staged by combining the type of osteomyelitis (I–IV) with the host comorbidities. For example, a patient with diabetes and a full-thickness but isolated cortical defect of the tibia would be a stage III B patient. An otherwise healthy patient with an infected nonunion of the tibia with full-thickness permeating circumferential bone involvement is a stage IV A patient.
For the purpose of simplicity, acute osteomyelitis will be defined as an infected fracture with some degree of bone involvement and extends up to 3 months from the traumatic event. Generally speaking, acute fracture infections and acute osteomyelitis are synonymous terms. On the other hand, chronic posttraumatic osteomyelitis develops over time allowing the infection to permeate deeply into the substance of the bone. It often results from the infection of necrotic bone in the acute phase or the lack of removal of metal associated with biofilm. A section of avascular necrotic bone forms the sequestrum, which harbors bacteria and prevents antibiotic penetration.
The Cierny classification is useful to the treating surgeon because it provides an anatomic road map and helps guide the surgical debridement of necrotic bone. Although the original intent of the classification did not define acute from chronic posttraumatic osteomyelitis, the timing of the infection often plays a role in the type of osteomyelitis. For example, an acute intramedullary nail infection is a type I infection because it involves the intramedullary canal but has not penetrated the cortex. Acute open fracture infections, which have incomplete cortical penetration, may be best described as type II infections. Many chronic infection trauma cases have converted to type III or IV as the bacteria penetrate the full depth of the cortex. Most chronic infected nonunions are defined as type IV osteomyelitis because the infection penetrates both sides of the nonunions and complete radical removal of both sides of nonunion is required to eliminate the infection.
26.2 The Causes of Posttraumatic Infections
Fractures become infected for a variety of reasons but can be broken down to five basic causes:
1.
Infection occurs when bacteria quantity exceeds the ability of immune system to eradicate it. This may seem obvious, but can be prevented by thorough excisional debridement at the time of open fracture surgery. The understanding of when to delay closure or close primarily is also important. This may be best addressed by the protocols seen at most level one trauma centers. The time between the injury and admission to the definitive level one trauma center was an independent predictor of the likelihood of infection by the LEAP study group [3]. No significant differences were found between patients who had development of an infection and those who did not when the groups were compared with regard to the time from the injury to the first debridement or the time from admission to the first debridement. Preoperative antibiotics are important in the prevention of infection, but the length of treatment of 24 h in open fractures was found just as effective when compared to 2–3 days, 4–5 days, or >5 days [4]. Greater length of treatment of antibiotics did not show any significant differences in the infection risk. The duration of surgery in closed ankle fractures of greater than 90 min was found to be a predictor of infection [5], which suggests more bacterial contamination with extended time of fracture exposure.
2.
Infection occurs when the soft tissue damage results in poor blood supply and delayed soft tissue healing. The most direct example of this is revealed in the data produced in combat injuries with infections after damage-controlled orthopedics and delayed IM nailing [6]. Forty percent of the nails became infected at an average of 15 days post nailing. Ninety-one percent of the infections were in soldiers with blast injuries as apposed to non-blast injuries, highlighting the importance of healthy soft tissue and local blood supply in the prevention of fracture site infections.
3.
Infections occur when the general health of the patient cannot adequately resists infection. This occurs in patients with diabetes, preexisting vascular disease, smoking history, malnutrition, etc. Bowen et al. [7] evaluated 174 patients with open long bone fractures and divided patients into three categories based on their comorbidities. Class A had no comorbidities, class B one to two, and class C patients three or more. The types of fractures were similar in all groups, but the infection rates were 4 % for class A, 15 % for class B, and 30 % for class C patients based solely on their general health status pre-injury.
4.
Infections occur when the bone remains unstable. Stability of the fracture site allows the soft tissue to heal and reestablish a vascular supply to the area and permits the patient’s immune system to resists infection locally. Basic science research has demonstrated that lab hamsters with bacterially contaminated femurs developed infection at a much lower rate if they underwent IM nailing of femurs when compared to hamsters with non-stabilized similarly contaminated femur fractures [8]. Temporizing external fixator for pilon and plateau fractures stabilizes the bone and soft tissue without compromising the soft tissue envelope. This allows the soft tissue to heal and has clearly reduced the risks of infection when definite surgical stabilization is performed [9, 10].
5.
Infections occur when internal hardware becomes exposed to bacteria. Studies have shown that the minimal infective dose is 10,000 times lower in the presence of metal [11, 12]. A glycocalyx from the bacteria forms a biofilm or slime layer on the implant. Once the biofilm is formed, the implant must be removed or the infection cannot be eradicated [13, 14].
26.3 Acute Posttraumatic Osteomyelitis
The physical exam findings of acute posttraumatic infection (less than 3 month) are erythema at the fracture site, continued drainage over an extended time, additional tissue necrosis, increased warmth, lymphadenopathy, unexpected increased in pain, and elevated body temperature. In many aggressive bacterial infections, like Staphylococcus aureus, the clinical symptoms of acute infection are obvious. However, in less aggressive bacteria, the signs and symptoms can be subtle. Radiographic findings may be helpful. The lack of any callus formation along with radiolucency around screws can be suggestive of infection. Hardware, particular non-locking screws, loosens and even back out around the fracture (Fig. 26.2). Medullary osteolysis around an intramedullary nail with pain extending to the insertion site is a typical finding. Screws are sometimes pushed out of the nail (Fig. 26.3). Previous x-rays should be used in the comparison. The erythrocyte sedimentation rate and the C-reactive protein are independently accurate predictors of infection [15]. An additional use of the white blood cell/sulfur colloid scan was not found to be predictive for infection. It is also not cost-effective.
Fig. 26.2
(a) Midshaft tibia plating. (b) Loosening of screws in early infection. (c) Clinically infected at 6 weeks
Fig. 26.3
(a) Three months after nailing in open tibia fracture in B host with diabetes, now with distal radiolucency and screw backing out due to gross infection. (b) Nail removed, canal reamed, and antibiotic nail placed. (c) Antibiotic nail removed at 5 months and tibia was healed
The diagnosis of acute and chronic infection can be made with the evaluation of symptoms, physical exam, radiograph comparison, ESR, and CRP alone 90 % of the time. Complex secondary studies are rarely needed but can be helpful in borderline cases. SPET/CT is useful in differentiating between soft tissue infection and osteomyelitis as well as between cortical, medullary, and subperiosteal infections [16]. Sensitivity ranges from 90 to 100 % and specificity from 80 to 90 % for diagnosing osteomyelitis. The most sensitive and specific test for pure osteomyelitis is the gadolinium MRI scan. Unfortunately, most posttraumatic cases have retained metal making MRI much less helpful.
The true diagnosis of acute or chronic infection requires multiple cultures (at least three) from deeply around or part of the bone in a patient off antibiotics for at least 1 week. Soft tissue or fistula specimens are much less reliable for diagnosis of the true infection [17]. Biopsy of the bone can be diagnostic for osteomyelitis, and excised bone should always be sent to pathology for permanent sections (Fig. 26.4). This can be very valuable in a patient that has been partially treated with antibiotics and the cultures may be negative. Once the diagnosis of acute osteomyelitis or infected fracture has been made, the treatment requires surgical debridement along with appropriate long-term, generally 6 weeks, IV antibiotic treatment for all A and B hosts. Most of the examples of acute osteomyelitis can be classified as type I (intramedullary) or type II (partial cortical). The volume of bone involved (osteomyelitis) varied mainly with the length of time that had elapsed before diagnosis and treatment [18]. The real question the surgeon needs to ask is “How aggressively should we treat an infected fracture?”
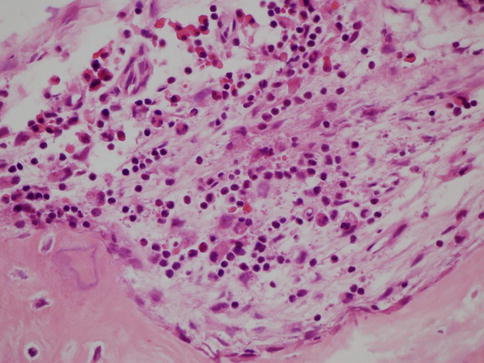
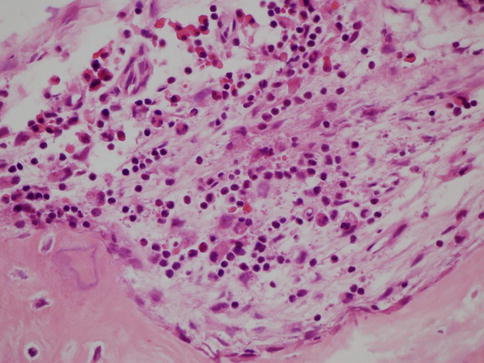
Fig. 26.4
Microscopic specimens demonstrating the invasion of acute and chronic inflammatory cells confirming infiltrating osteomyelitis
The answer is that almost all acute posttraumatic infections require surgical debridement along with appropriate, culture-directed antibiotics. Unless you have proven this to be cellulitis ONLY (very rare) or the patient has turned into a C host, antibiotics alone are generally not the best therapy. It appears that surgical debridement and retention of hardware are warranted up to 6 weeks post-op. The success rate of a healed fracture and no infection after this technique is approximately 70 % [19, 20]. High failure rates were seen in patients with open fracture, IM tibia nails, smokers, and pseudomonas infections. In these later cases, the surgeon may consider removing the hardware with debridement even before 6 weeks. After 6 weeks from the definitive internal fixation, the infection has most likely produced a biofilm on the hardware and retention will most likely not cure the problem. The hardware needs to be removed, the infection of the bone debrided, and the bone somehow stabilized in a different manner.
In the case of infected IM tibia nails (type I osteomyelitis), there are several ways of dealing with this problem. Some have recommended exchanged nailing acutely, reaming, and renailing [18]. This works because reaming debrides the intramedullary bone infection and the biofilm is eliminated by the removal of the original nail. Others have recommended removal of the nail, reaming, and external fixation [21]. Still others have recommended removal of the nail, reaming, placement of temporary antibiotic rod, and renailing at the second stage [22, 23] (Fig. 26.5). All these techniques have excellent results if the patient has not progressed to type III or IV osteomyelitis at the original fracture site. Permeative osteomyelitis (III, IV) tends to occur in chronic situations and is the most common reason exchange nail fails with reinfection at times. Renailing DOES NOT adequately debride permeative osteomyelitis at the fracture site in type III or IV osteomyelitis. Radical excisional debridement and bone transport are required for these more extensive infections (see Chronic Infected Nonunions).
Fig. 26.5
(a) Grade III open midshaft tibia fracture. (b) IM nail placed and infected at 8 weeks. (c) Nail removed, canal reamed, and antibiotic nail placed. (d) Renailed at 16 weeks
At the site of an open tibia fracture, when the soft tissue fails acutely and is not replaced, the bone can develop partial cortical involvement (type II osteomyelitis) requiring direct and aggressive debridement at the fracture site. This must include partial cortical debridement to eliminate the exposed boney surface infection. Some of the bone fragments that were left during the original excisional debridement may not be viable and have developed partial-thickness osteomyelitis. In those cases the deep fragments are removed. If the original trauma or debridement creates a significant bone defect, antibiotic methyl methacrylate beads or calcium sulfate (absorbable) beads can be used to dispense local antibiotics and produce a space filler [24]. The most important additional component of successful treatment is to provide adequate soft tissue coverage [25]. The muscle flap provides not only protection from outside contamination and recontamination, but increases the local blood supply (antibiotics) and a reliable surgical window for future bone grafting. The soft tissue covering the area of bone trauma must heal or the existing bone infection will persist or the patient will have new bone infections develop [26]. A clinical example would be an acute infected proximal tibia fracture that was plated 10 weeks early, requiring removal of hardware, partial cortical debridement (type II osteomyelitis), gastrocnemius rotational muscle flap, and definitive ring fixator for stability (Fig. 26.6).
Fig. 26.6
(a, b) AP and lateral x-rays of tibial plateau fracture, B host. (c) Open reduction and internal fixation. (d) Infected at 3 months but not healed. (e, f) All hardware removed, fracture debrided, and TSF applied for type II osteomyelitis. (g, h) Healed plateau fracture at 6 months, no infection. (i) Clinical result and alignment
The static wire fixator is an important tool in the treatment of acute osteomyelitis, particularly after 6 weeks when the hardware often needs to be removed; yet the fracture still needs stability. The ring fixator (particularly Taylor Spatial Frames) can extend into the metaphysis, provide compression in the oblique plane (compress fractures), can be stable enough for definitive treatment, and does NOT add additional metal directly into the infected area. On the other hand, if the patient had an infected IM nail after 6 weeks, with type I or II osteomyelitis, my preferential treatment strategy is to remove the nail, debride the bone, and use the antibiotic nail temporary for stability, followed by second stage renailing when the infection has been eliminated. Healing and complete elimination of infection should be pursued in the most direct, expedient, and cost-effective strategy possible in acute osteomyelitis. This is a surgical disease and requires a surgical treatment (along with antibiotics) to appropriately address the problem and reduce the risk of the development of chronic osteomyelitis.
26.4 Chronic Posttraumatic Osteomyelitis
Posttraumatic osteomyelitis is an unfortunate consequence of injuries resulting from the treatment of open fractures and open treatment of closed fractures, which develops after at least 3 months. Often the soft tissue envelope is significantly compromised, producing poor blood supply and limiting surgical access to the bone. Cierny et al.’s [1, 2] type III (complete single cortex) and stage IV (permeative) are most often seen. Type IV osteomyelitis is by far more common because it is seen, but not limited to, patients with infected nonunions.
The basic steps to treating patients with chronic osteomyelitis are debridement of infected bone, obliteration of dead space, restoration of the blood supply, obtaining adequate soft tissue coverage, stabilization of the bone, and reconstruction of the defect.
Patients with type III can be treated without segmental reconstruction because the osteomyelitis has only penetrated one cortex and into the medullary canal (Figs. 26.7a, b). The illustrated case demonstrates removal of the affected cortex, collection of deep culture, and debridement into the canal until the bone bleeds. A positive “paprika sign” demonstrates punctate bleeding of the edges of the cortical bone after resection indicating the surgeon has achieved viable bone margins at the resection [2]. This can be done with a high-speed burr and irrigation to prevent thermal necrosis. Antibiotic beads are placed into the defect, the soft tissue is closed primarily (Fig. 26.7c), and monolateral external fixator is added to protect the remaining cortex. Adjunctive IV antibiotics are given for 6 weeks and the simple external fixator allows some weight bearing.
Fig. 26.7
(a) Midshaft tibia AP x-ray of radiolucent osteomyelitis. (b, c) Surgical dissection of type III osteomyelitis and placement of antibiotic beads. (d) AP x-rays of antibiotic beads and external fixator in place. (e) After fixator removed, defect bone grafted and tibia healed
Stage two occurs when the antibiotic course is complete, the site looks noninfective, and the acute phase reactants have normalized. Stage two consists of removal of the beads, re-culturing, and placement of iliac crest bone graft (ICBG) into the defect (Fig. 26.7d). Additional antibiotics are given if the cultures are positive. As a technical note, the ICBG should NOT be contaminated by the osteomyelitis debridement, assuming the osteomyelitis defect may still be infected. This will keep the ICBG site from being infected by osteomyelitis. If the surgeon chooses to harvest the ICBG first, before opening the defect, this is not a problem. However, from time to time, the surgeon may open the defect and find gross pustulant tissue, with the ICBG already harvested. If this should occur, it is recommended that the ICBG be frozen, the defect is redebrided, new antibiotic beads are placed, and the ICBG be saved for another surgical day.

Full access? Get Clinical Tree







