CHAPTER 175
Pityriasis Rosea
Presentation
Patients with this rash often seek acute medical help because of the worrisome sudden spread of a rash that began with one local skin lesion. This “herald patch” may develop anywhere on the body, but it is typically on the trunk and appears as an ovoid, 2 to 6 cm in diameter, mildly erythematous and slightly raised scaling plaque with a collarette of scale at the margin (Figure 175-1). There is no change for a period of several days to a few weeks; then the generalized rash appears, composed of crops of small (0.5 to 2 cm), pale, salmon-colored, oval, raised macules or plaques with a coarse surface surrounded by the same rim of fine scales as the herald patch (Figure 175-2). The distribution is usually truncal (face, hands, and feet being spared), with the long axis of the oval lesions running in the planes of cleavage of the skin (Langer lines, which are parallel to the ribs), giving it a typical “Christmas tree” appearance and making the diagnosis (Figure 175-3).

Figure 175-1 Herald patch on the arm with a collarette of scale at the margin. (From White G, Cox N: Diseases of the skin, ed 2. St Louis, 2006, Mosby.)

Figure 175-2 Pityriasis rosea with herald patch and subtle smaller spots on trunk.
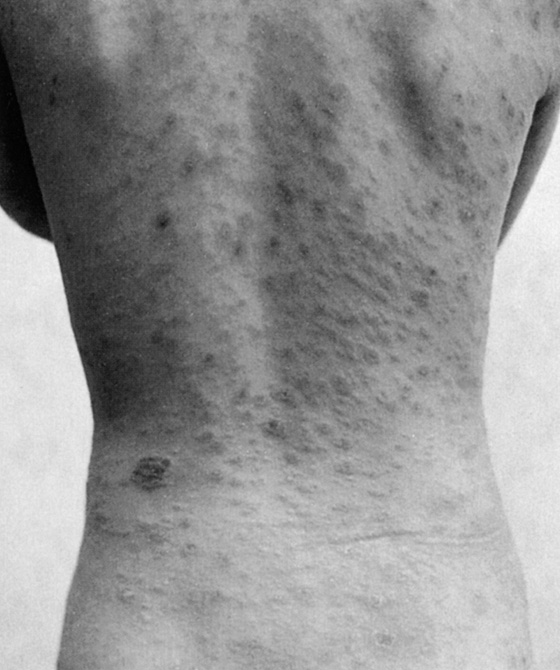
Figure 175-3 Typical “Christmas tree” pattern of pityriasis rosea. (From Leung AKS, Wong BE, Chan PYH: Pediatrics review. Resident Staff Physician 43:109, 1997.)
The condition may be asymptomatic or accompanied by varying degrees of pruritus (25% of patients have mild to severe itching). No systemic symptoms typically are present during the rash phase of pityriasis rosea (PR). The lesions will gradually extend in size and may become confluent with one another. The rash persists for 6 to 8 weeks and then completely disappears. Transient worsening of the rash or a second wave of lesions is not uncommon until eventual spontaneous resolution of the eruption. Recurrence of the condition later in life is rare.
Pityriasis rosea can have a distinctly different appearance on patients with brown skin or dark skin. The herald patch, as well as the diffuse rash that follows, may have a gray, dark brown, or even black appearance. There may be either hypopigmented or hyperpigmented areas visible after the lesions resolve.
What To Do:
 After performing a careful history and physical examination, reassure patients about the benign self-limited nature of this disease. Be sympathetic, and let them know that it is understandable how frightening it can seem. Inform them that the rash will last for 6 to 8 weeks. In addition, inform them about the need to contact their physician if the rash or pruritus lasts more than 3 months.
After performing a careful history and physical examination, reassure patients about the benign self-limited nature of this disease. Be sympathetic, and let them know that it is understandable how frightening it can seem. Inform them that the rash will last for 6 to 8 weeks. In addition, inform them about the need to contact their physician if the rash or pruritus lasts more than 3 months.
 Encourage sun exposure, because it hastens resolution of individual lesions.
Encourage sun exposure, because it hastens resolution of individual lesions.
 Acyclovir may be effective in the treatment of pityriasis rosea, especially in patients treated within the first week of onset of the generalized rash. Prescribe acyclovir (Zovirax), 800 mg given five times daily for 7 days. This dosage hastened the clearance of lesions in one placebo-controlled study. A single patient has been reported, however, who developed PR while taking low doses of acyclovir. Early high doses of acyclovir should probably be prescribed in pregnancy to prevent miscarriage or premature births, especially when PR develops during the first weeks of gestation, when the lesions have an unusual extension and long duration, and when constitutional symptoms are present. At the moment, however, no treatment can be recommended on the basis of evidence-based medicine.
Acyclovir may be effective in the treatment of pityriasis rosea, especially in patients treated within the first week of onset of the generalized rash. Prescribe acyclovir (Zovirax), 800 mg given five times daily for 7 days. This dosage hastened the clearance of lesions in one placebo-controlled study. A single patient has been reported, however, who developed PR while taking low doses of acyclovir. Early high doses of acyclovir should probably be prescribed in pregnancy to prevent miscarriage or premature births, especially when PR develops during the first weeks of gestation, when the lesions have an unusual extension and long duration, and when constitutional symptoms are present. At the moment, however, no treatment can be recommended on the basis of evidence-based medicine.
 If the diagnosis is uncertain, especially if the palms and soles are affected and the patient is sexually active, draw blood for serologic testing for syphilis (e.g., rapid plasma reagin [RPR], Venereal Disease Research Laboratory [VDRL]). Secondary syphilis can mimic pityriasis rosea. Make a note to track down the results of the test.
If the diagnosis is uncertain, especially if the palms and soles are affected and the patient is sexually active, draw blood for serologic testing for syphilis (e.g., rapid plasma reagin [RPR], Venereal Disease Research Laboratory [VDRL]). Secondary syphilis can mimic pityriasis rosea. Make a note to track down the results of the test.
 Microscopy with potassium hydroxide (KOH) preparation may be helpful to distinguish a herald patch from a tinea infection.
Microscopy with potassium hydroxide (KOH) preparation may be helpful to distinguish a herald patch from a tinea infection.
 Provide relief from pruritus by prescribing hydroxyzine (Atarax), 25 to 50 mg q6h, or an emollient, such as Lubriderm. Tepid cornstarch baths (1 cup in ½ tub of water) may also be comforting.
Provide relief from pruritus by prescribing hydroxyzine (Atarax), 25 to 50 mg q6h, or an emollient, such as Lubriderm. Tepid cornstarch baths (1 cup in ½ tub of water) may also be comforting.
What Not To Do:
 Do not have a biopsy performed when findings are typical for pityriasis rosea. A biopsy is not indicated.
Do not have a biopsy performed when findings are typical for pityriasis rosea. A biopsy is not indicated.
 Do not routinely use topical or systemic steroids. These are effective only in the most severe inflammatory varieties of this syndrome. Topical steroids may cause the eruption to generalize to erythroderma.
Do not routinely use topical or systemic steroids. These are effective only in the most severe inflammatory varieties of this syndrome. Topical steroids may cause the eruption to generalize to erythroderma.
 Do not send off a serologic test for syphilis without ensuring that the results will be seen and acted on.
Do not send off a serologic test for syphilis without ensuring that the results will be seen and acted on.
Discussion
Pityriasis rosea (PR) is a common, acute exanthem of uncertain cause. PR most commonly affects adolescents, with a concentration of cases in the 10- to 35-year-old age range, peaking in persons 20 to 29 years of age. PR occurs in pregnancy more frequently than in the general population (18% vs. 6%). The diagnosis of PR can usually be made based on the appearance of the lesions and the history. It has been described in the medical literature for more than 200 years but was given its current name by Camille Gilbert in 1860. Viral and bacterial causes have been sought, but convincing answers have not yet been found. PR shares many features with the viral exanthemas of childhood, and cases tend to cluster in the fall and winter.
Recently, an increasing number of studies have focused on human herpes virus 6 (HHV-6) and, primarily, on HHV-7 as causative agents. The skin lesions would not be a result of a direct infection of skin cells but, rather, would occur as a reactive response to the systemic HHV-6 and HHV-7 replication, alone or through the interaction with other viruses. The higher proportion of pregnant women with PR is probably related to the altered maternal immunity, the innate proinflammatory immune responses being tightly regulated to prevent immunologic rejection of the fetal allograft. In fact, HHV-6 reactivation seems common during pregnancy, and this fact may be one of the causes of spontaneous abortions.
Results of a controlled trial (neither randomized nor double-blind) with oral acyclovir suggest that early treatment with this antiviral is justified, because it apparently reduces the duration and severity of symptoms.
Up to 69% of patients with PR have a prodromal illness before the herald patch appears. Malaise, nausea, loss of appetite, headache, difficulty in concentration, irritability, gastrointestinal and upper respiratory symptoms (up to 69%), joint pain, swelling of lymph nodes, sore throat, and mild fever are often, although inconsistently, reported.
The herald patch often is misdiagnosed as eczema. PR is difficult to identify until the appearance of the characteristic smaller secondary lesions. When these secondary lesions are not on the patient’s back, where they form the typical “Christmas tree” pattern, the lesions follow the cleavage lines in the following patterns: transversely across the lower abdomen and back, circumferentially around the shoulders, and in a V-shaped pattern on the upper chest.
The “herald patch” may not be seen in 20% to 30% of cases, and there are many variations from the classic presentation described. Atypical cases make up 20% of the total and occur more commonly in children. Lesions can exhibit urticarial, vesicular, pustular, or purpuric characteristics. Infrequently, oral lesions will accompany the skin rash and resolve along with it: These include punctate hemorrhages, erosions, ulcerations, erythematous macules, annular lesions, and plaques.
There are no noninvasive tests that confirm the diagnosis of PR. Other diagnostic considerations besides syphilis include tinea corporis, seborrheic dermatitis, guttate psoriasis, and tinea versicolor.
Numerous drugs have been implicated in a severe prolonged exanthem that resembles PR. Some of the medications that have been associated with a PR-type rash include bismuth, bacillus Calmette-Guérin (BCG) vaccine, captopril, clonidine, diphtheria toxoid, gold, isotretinoin, ketotifen, metronidazole, and omeprazole.
Persistence of a rash beyond 3 months should prompt a clinician to reconsider the original diagnosis, to consider biopsy to confirm the diagnosis, and to check for the use of medications that may cause a rash similar to that of PR.

Full access? Get Clinical Tree


