Changes in cardiac output through the trimesters of pregnancy
Patient posture has been found to influence cardiac output measurements during pregnancy (Figure 23.3). Measurements performed in the lateral position, to avoid aortocaval compression, demonstrate an increase in cardiac output by 5 weeks gestation.
| Position | Change in cardiac output |
|---|---|
| Supine | Baseline |
| Left lateral | ↑ by 13.5% |
| Lithotomy | ↓ by 17% |
| Steep Trendelenburg | ↓ by 18% |
A further transient rise in cardiac output occurs during labour, at delivery and in the immediate period after delivery as a result of uteroplacental transfusion of 300–500 mL of blood from the intervillous space into the maternal intravascular volume (autotransfusion). Cardiac output increases by a further 45% during contractions, a further 60% in the second stage, and up to a further 80% immediately after delivery when compared with the pre-delivery state.
Cardiac output increases throughout pregnancy, to reach a level of 50% greater than in the non-pregnant state during the last trimester.
The increase in cardiac output in pregnancy is produced by a combination of increased heart rate, reduced systemic vascular resistance (SVR) and increased stroke volume.
Heart rate and stroke volume
Heart rate (HR) is increased above non-pregnant values by 15% at the end of the first trimester. This increases to 25% by the end of the second trimester, but there is no further change in the third trimester.
Stroke volume (SV) is increased by about 20% at 8 weeks and by up to 30% by the end of the second trimester, after which it remains level until term (Figure 23.2). Stroke volume and heart rate both increase during labour and immediately post delivery.
Systemic vascular resistance and blood flow to organs
Systemic vascular resistance (SVR) is reduced during pregnancy. The average SVR in pregnancy is about 980 dyne.s.cm−5, compared with about 1150 dyne.s.cm−5 in non-pregnant women. The decrease in the SVR results from the development of a low-resistance vascular bed (the intervillous space) and vasodilatory effects of oestrogens, prostacyclin and progesterone.
Distribution of the cardiac output during pregnancy is different from that of the non-pregnant state, with increased blood flow to the uterus, kidneys and skin. Uterine blood flow varies from 500 to 700 mL min−1 (about 10–12% of the cardiac output) at term, of which > 80% perfuses the placenta. The flow to the kidneys is increased, as is the flow to the skin due to peripheral vasodilatation. Flow to the liver and brain remains unchanged.
Blood pressure
Blood pressure falls during pregnancy and returns towards the baseline near term. Systolic blood pressure is minimally affected, with a maximum decline of 8% during early and mid-gestation, returning to non-pregnant levels at term. Diastolic blood pressure falls to a greater extent, with early and mid-gestational decreases of 20–25%, and returns to normal at term. In the supine position, 70% of mothers have a fall in blood pressure of at least 10%, and 8% have decreases of 30–50%.
Aortocaval compression
Compression of the inferior vena cava (IVC) and aorta by the gravid uterus occurs during pregnancy and reduces cardiac output. The severity of this effect is dependent on:
Patient position
Gestation
Systemic blood pressure
Presence of sympathetic block
In the supine position during pregnancy, IVC obstruction occurs and venous blood bypasses this obstruction primarily via vertebral venous plexuses which empty into the azygos vein. IVC compression develops as early as 13–16 weeks gestation, causing a 50% increase in femoral venous pressures. Near term, women in the supine position may experience a 10–20% reduction in stroke volume and cardiac output. This effect becomes maximal between 36 and 38 weeks, after which it may decline as the fetal head descends into the pelvis. Moving from a supine to a lateral position reduces the femoral and IVC pressures, but these are still elevated above those of the non-pregnant woman, indicating that the compression of the IVC is not completely relieved by lateral positioning. In the supine position, 15–20% of pregnant women experience a substantial drop in blood pressure (supine hypotension syndrome), and the patients develop systemic signs of shock, i.e. pallor, sweating, nausea, vomiting and syncope.
Obstruction of the aorta in the supine position has been demonstrated angiographically, but the higher pressures in the aorta prevent total obstruction. This does not cause maternal hypotension but causes arterial hypotension in the lower extremities and in the uterine arteries, which can lead to inadequate uterine blood flow resulting in fetal asphyxia and bradycardia.
Electrocardiogram (ECG) and echocardiogram
The ECG in pregnancy may show the following changes:
Sinus tachycardia, reduced PR interval and reduced uncorrected QT interval
Rotation of the electrical axis of the heart to the left
ST segment depression
T wave flattening
However, these changes are thought to be of no clinical significance.
Echocardiographic studies during pregnancy have shown:
Left ventricular hypertrophy from 12 weeks gestation.
A 50% increase in left ventricular mass at term. This is due to increase in the size of cardiomyocytes.
A 12–14% increase in tricuspid, pulmonary and mitral valve annular diameters. The majority of pregnant women have tricuspid and pulmonary regurgitation, and 27% have mitral regurgitation.
Studies have demonstrated a high incidence of asymptomatic pericardial effusion during normal pregnancy.
Heart sounds
The apical impulse moves to the fourth intercostal space and mid-clavicular line. Most pregnant women develop a loud and sometimes split first heart sound. A third heart sound is common, and 16% of women have a fourth heart sound. A grade I–II early to mid-systolic heart murmur is commonly heard at the left sternal edge. This may be due to tricuspid regurgitation resulting from dilatation of the tricuspid valve.
Venous pressure
In the absence of IVC compression by the uterus, central venous pressure (CVP) and venous pressure in the upper limbs are normal. However, during late pregnancy when in the supine position, IVC compression by the gravid uterus occurs and CVP may decrease dramatically. IVC compression can also cause increased venous pressure in the lower limbs.
During labour various factors can cause an increase in CVP, including:
Contractions – can increase CVP by about 5 cmH2O.
Expulsive efforts of the second stage – can create a major rise in CVP by up to 50 cmH2O.
IV ergometrine 0.25 mg after delivery of the baby can produce a rise in CVP of 8 cmH2O, which can last up to 60 minutes.
There are no observed changes in pulmonary capillary wedge and pulmonary artery pressures during pregnancy.
Haematology
The haematological changes found at term are summarised in Figure 23.4.
| Parameter | Change | |
|---|---|---|
| Blood volumes | Total blood volume | ↑ by 45% |
| Plasma volume | ↑ by 50% | |
| Blood cells | Red blood cell volume | ↑ by 18% |
| White cell count | ↑ | |
| Haematocrit | ↓ by 15% | |
| Haemoglobin | ↓ by 15% | |
| Plasma proteins | Total plasma protein | ↓ by 18% |
| Albumin | ↓ by 14% | |
| Globulin | ↓ or ↑ | |
| Plasma cholinesterase | ↓ by 20–25% | |
| Colloid osmotic pressure | ↓ by 18% | |
| Coagulation | Platelets | ↓ by 0-5% |
| Prothrombin time | ↓ by 20% | |
| Bleeding time | ↓ by 10% | |
| Partial thromboplastin time | ↓ by 20% | |
| Antithrombin III | ↓ by 10% | |
| Fibrinogen | ↑ from 2.5 to 4.6 g L−1 | |
| Fibrin degradation | ↑ by 100% | |
| Products | ||
| Plasminogen | ↑ | |
| Fibrinolysis | ↑ | |
| Thromboelastography | Hypercoagulable state | |
| Clotting factors | I | ↑ by 100% |
| VII | ↑ by 100% | |
| VIII | ↑ by 150% | |
| IX | ↑ by 100% | |
| X | ↑ by 30% | |
| XII | ↑ by 30% | |
| XI | ↓ by 40–50% | |
| XIII | ↓ by 50% | |
| Antithrombin III | ↓ by 10% | |
| II | ← → | |
| V | ← → |
Blood volume
Plasma volume (PV), total blood volume (TBV) and red blood cell volume (RBCV) all increase during pregnancy. The development of these changes through the trimesters is illustrated in Figure 23.5. Plasma volume rises by 15% during the first trimester and can reach 50% above non-pregnant values by 32 weeks; it then remains at this level unchanged. Plasma volume returns to non-pregnant levels by 6 days post delivery. There is often a sharp rise of up to 1 litre in plasma volume 24 hours after delivery. This is of significant importance in patients with cardiac disease, such as those with fixed cardiac output. Such patients may develop pulmonary oedema during this period.
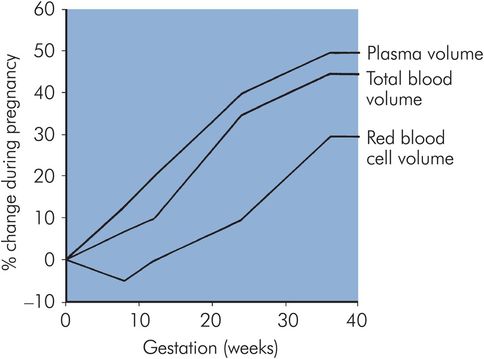
Changes in PV, TBV and RBCV through the trimesters of pregnancy
RBC volume falls during the first 8 weeks of pregnancy, increasing back to non-pregnant levels by 16 weeks and then rising to 30% above non-pregnant levels by term. This increase in RBC volume is due to raised erythropoietin levels that occur from 12 weeks gestation.
The physiological anaemia of pregnancy arises from the increase of only 30% in RBC volume, relative to an increase of 50% in plasma volume in the last trimester. This results in overall reductions of about 15% in haemoglobin (Hb) and haematocrit.
The above changes combine to give total blood volume increases of 10%, 30% and 45% at the end of the first, second and third trimester respectively (Figure 23.5). Oestrogens and progesterone appear responsible for the increase in plasma volume through their effect on the renin–angiotensin–aldosterone systems.
Immune system
The white blood cell (WBC) count rises progressively during pregnancy from non-pregnant levels to 9–11 × 109 L−1. This is predominantly an increase in polymorphonuclear cells. There is a further leucocytosis to about 15 × 109 L−1 during labour. White cell count returns to normal by 6 days post delivery. Serum levels of IgA, IgG and IgM remain unchanged.
In spite of a leucocytosis during pregnancy, depressed neutrophil chemotaxis and adherence leads to reduced polymorphonuclear leucocyte function. This may account for the increased incidence of infection during pregnancy and the reduced incidence of symptoms in women with autoimmune diseases such as rheumatoid arthritis.
Coagulation
Pregnancy is associated with enhanced platelet turnover, clotting and fibrinolysis (Figure 23.4). Thrombocytopenia (platelets < 100 × 109 L−1) occurs in 0.8–0.9% of normal pregnant women, while increases in platelet factor and β-thromboglobulin suggest elevated platelet activation and consumption. Since there is no change in platelet count in the majority of women during pregnancy, there is probably an increase in platelet production to compensate for the increased consumption. Platelet function, however, remains normal during pregnancy.
The concentrations of most coagulation factors (I, VII–X and XII) are increased, and a few (XI and XIII) are reduced. The levels of factors II and V remain the same during pregnancy. There are increases in fibrin degradation products (FDP) and plasminogen concentrations which indicate increased fibrinolytic activity during pregnancy.
Plasma proteins
The plasma concentration of albumin is reduced to 34–39 g L−1, but fibrinogen levels are increased. Globulin is reduced in the first trimester then increases to 10% above the pre-pregnancy level at term. These reductions in plasma proteins are associated with the following changes (Figure 23.4):
Total colloid osmotic pressure is reduced by 5 mmHg.
Drug-binding capacity of the plasma is altered, with consequent changes in pharmacokinetics and dynamics (e.g. a reduction in plasma α-acid glycoprotein concentration reduces the lidocaine binding capacity).
Plasma concentration of plasma cholinesterase is reduced by 20–25% at term.
Erythrocyte sedimentation rate (ESR) and blood viscosity are increased.
Respiratory system
Anatomical changes
Capillary engorgement and oedema of the mucosa of nasal cavity, pharynx and larynx begin early in the first trimester. This may explain why many pregnant women complain of difficulty in nasal breathing, have more episodes of epistaxis and experience voice changes. The thoracic cage increases in circumference by 5–7 cm because of the increase in both the anteroposterior and transverse diameters from flaring of the ribs. Flaring of the ribs begins early in pregnancy, and is therefore not entirely due to pressure from the enlarging uterus. The enlarging uterus displaces the diaphragm upwards in the later weeks of pregnancy, but the internal volume of the thoracic cavity remains unchanged (Figure 23.6).
| Parameter | Change | |
|---|---|---|
| Anatomy | Capillary engorgement | ↑ |
| Upper airway | ↑ swelling | |
| Airways | Dilated | |
| Diaphragm | Elevated | |
| Thoracic circumference | ↑ by 5–7cm | |
| Lung volumes | Tidal volume | ↑ by 45% |
| Inspiratory reserve volume | ↑ by 5% | |
| Expiratory reserve volume | ↓ by 25% | |
| Residual volume | ↓ by 20% | |
| Functional residual capacity | ↓ by 30% | |
| Total lung capacity | ↓ by 0–5% | |
| Vital capacity | Nil | |
| Closing capacity | Nil | |
| Ventilation | Minute ventilation (MV) | ↑ by 50% |
| Alveolar ventilation (AV) | ↑ by 70% | |
| Respiratory rate (RR) | ↑ by 0–15% | |
| Dead space | ↑ by 45% | |
| Lung mechanics | Diaphragm movement | ↑ |
| Chest wall movement | ↓ | |
| Total pulmonary resistance | ↓ by 50% | |
| Lung compliance | nil | |
| FEV1 | nil | |
| FEV1/VC | nil | |
| Flow volume loop | nil | |
| Arterial blood gases | PaCO2 | ↓ to 3.7–4.2kPa |
| PaO2 | ↑ to 13.3–14.6 kPa | |
| pH | ↑ to 7.44 | |
| HCO3 | ↓ to 18–21 mmol L−1 |
Lung mechanics and volumes
Inspiration is mainly as a result of diaphragmatic movement, since flaring of the ribs reduces chest wall movement. Bronchial smooth muscle relaxation decreases airway resistance but lung compliance remains unchanged. Factors contributing to airway dilatation include direct effects of progesterone, cortisone and relaxin.
Forced expiratory volume at 1 second (FEV1), the ratio of FEV1 to forced vital capacity (FVC), and the flow–volume loop remain unchanged, demonstrating that large airway function is not impaired during pregnancy.
The following changes in lung volumes occur during pregnancy, relative to non-pregnant values:
Tidal volume (TV) increases steadily from the first trimester, by up to 45% at term (Figure 23.7).
Functional residual capacity (FRC) is decreased by 20–30% at term due to reductions of 25% in expiratory reserve volume (ERV) and 15% in residual volume (Figure 23.6).
Closing capacity can encroach on FRC, increasing ventilation/perfusion mismatch and leading to the ready occurrence of hypoxia, particularly in supine and Trendelenburg positions.
Inspiratory capacity increases by 15% at term due to increases in inspiratory reserve and tidal volumes.
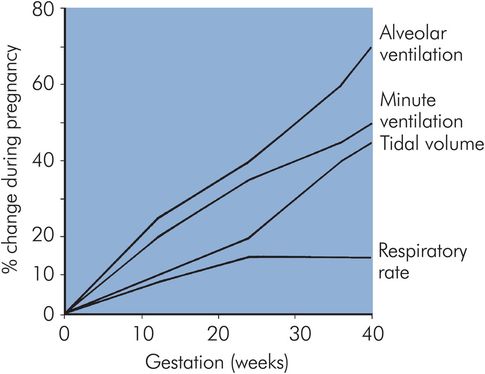
Progression of AV, MV, TV and RR changes through the trimesters of pregnancy

Full access? Get Clinical Tree







