CHAPTER 81
Phimosis and Paraphimosis
Presentation
Phimosis is the inability to retract the foreskin over the glans and is usually the result of a contracted preputial opening (Figure 81-1). Patients with phimosis may seek acute medical care when they develop signs and symptoms of infection, such as pain and swelling of the foreskin and a purulent discharge. Pediatric patients with acute phimosis are either fussy or complain of penile pain over hours to days. Children also may develop hematuria or urinary retention because of obstruction or dysuria. On physical examination, the physician discovers a tender foreskin that is not easily retracted.
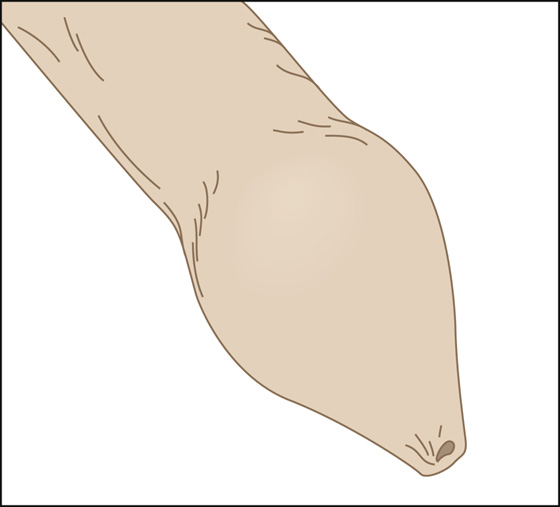
Figure 81-1 Phimosis.
Paraphimosis occurs when a tight foreskin cannot be re-placed into its normal position after it is retracted behind the glans. The tight ring of preputial skin (phimotic ring), which is caught behind the glans, creates a venous and lymphatic tourniquet that leads to edematous swelling of the foreskin and glans. It usually presents as a swollen tender penis with a large ventral penile-skin bulge and multiple folds just under the glans (Figures 81-2 and 81-3).
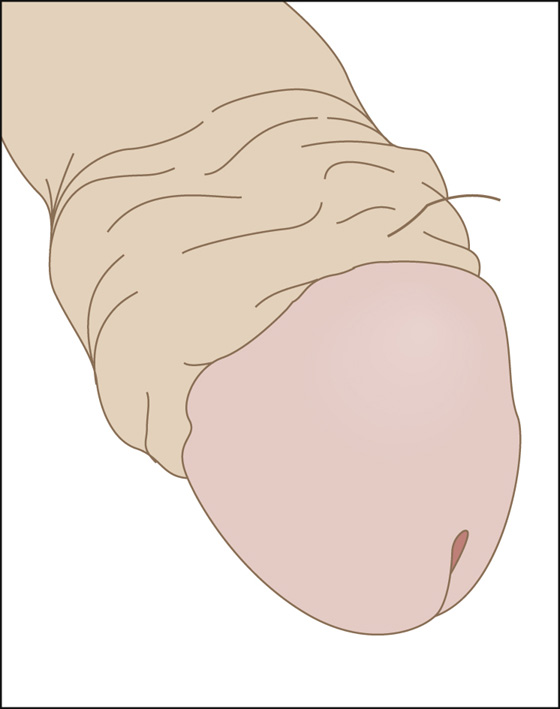
Figure 81-2 Paraphimosis.

Figure 81-3 Paraphimosis. (Adapted from McGrath N, Howell JM, Davis JE: Pediatric genitourinary emergencies. Emerg Med Clin North Am 29:655-666, 2011.)
What To Do:
 When either of these conditions becomes painful, provide adequate analgesia with oral or parenteral medication. A penile nerve block may be required. Using a 30-g needle, inject 1% lidocaine (Xylocaine) approximately 1 cm distal to the base of the penis, where it exits beneath the pubic arch at the 10-o’clock and 2-o’clock positions of the dorsum of the penis. Use caution not to inject intravascularly. If this does not provide adequate anesthesia, a ring block can be performed around the entire circumference of the base of the penis.
When either of these conditions becomes painful, provide adequate analgesia with oral or parenteral medication. A penile nerve block may be required. Using a 30-g needle, inject 1% lidocaine (Xylocaine) approximately 1 cm distal to the base of the penis, where it exits beneath the pubic arch at the 10-o’clock and 2-o’clock positions of the dorsum of the penis. Use caution not to inject intravascularly. If this does not provide adequate anesthesia, a ring block can be performed around the entire circumference of the base of the penis.
 For paraphimosis, squeeze the glans firmly for at least 10 minutes to reduce the edematous swelling. Wrap the shaft and swollen glans with a gauze pad followed by a 2-inch elastic bandage to produce constant, gentle compression. After 10 to 15 minutes, remove the bandage, push the glans proximally, and slide the prepuce back over the glans (Figure 81-4). An alternative approach for reducing the swelling is to apply an ice-filled surgical glove for 5 minutes.
For paraphimosis, squeeze the glans firmly for at least 10 minutes to reduce the edematous swelling. Wrap the shaft and swollen glans with a gauze pad followed by a 2-inch elastic bandage to produce constant, gentle compression. After 10 to 15 minutes, remove the bandage, push the glans proximally, and slide the prepuce back over the glans (Figure 81-4). An alternative approach for reducing the swelling is to apply an ice-filled surgical glove for 5 minutes.
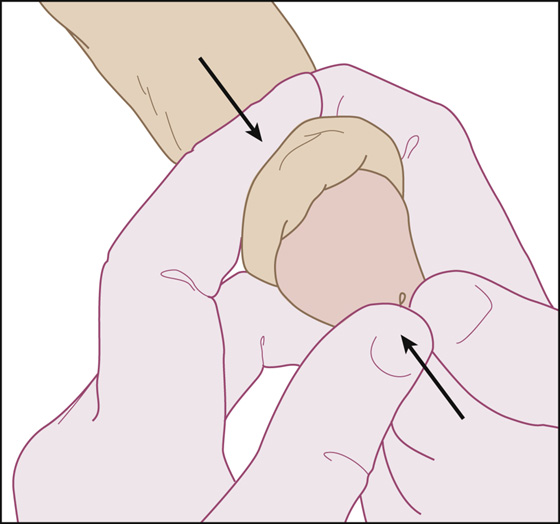
Figure 81-4 Manual reduction of paraphimosis by counter pressure between thumbs and fingers.
 If manual reduction fails and the penis does not regain its normal uncircumcised appearance, anesthetize the dorsal foreskin and carefully grasp the foreskin with nonserrated clamps and pull it over the glans penis. If this is unsuccessful, crush the dorsal foreskin with a straight hemostat along the midline and then make a linear incision through this crushed skin track. This incision will relieve the constricting band. The foreskin is then repositioned over the glans and, when possible, sutured in place.
If manual reduction fails and the penis does not regain its normal uncircumcised appearance, anesthetize the dorsal foreskin and carefully grasp the foreskin with nonserrated clamps and pull it over the glans penis. If this is unsuccessful, crush the dorsal foreskin with a straight hemostat along the midline and then make a linear incision through this crushed skin track. This incision will relieve the constricting band. The foreskin is then repositioned over the glans and, when possible, sutured in place.
 If the phimosis patient has secondary urinary obstruction, catheterize the urethra with a small-gauge catheter. If you cannot find the urethral meatus, try using a small nasal speculum or hemostat to widen the opening or anesthetize the dorsal foreskin, and carefully incise the constricting tissue with a vertical incision (dorsal slit) to allow retraction.
If the phimosis patient has secondary urinary obstruction, catheterize the urethra with a small-gauge catheter. If you cannot find the urethral meatus, try using a small nasal speculum or hemostat to widen the opening or anesthetize the dorsal foreskin, and carefully incise the constricting tissue with a vertical incision (dorsal slit) to allow retraction.
 Treating phimosis usually involves the management of acute infection. Frequent hot compresses or soaks are needed, along with antibiotics. Topical antibiotics, such as mupirocin (Bactroban), may be adequate when poor hygiene leads to infection in the pediatric patient. Sexually transmitted diseases should be suspected and treated appropriately in adolescents and adults (see Chapter 83). Candidal infections, with their typical white cheesy exudate, are often associated with diabetes mellitus and can be treated with a single dose of fluconazole (Diflucan), 200 mg PO.
Treating phimosis usually involves the management of acute infection. Frequent hot compresses or soaks are needed, along with antibiotics. Topical antibiotics, such as mupirocin (Bactroban), may be adequate when poor hygiene leads to infection in the pediatric patient. Sexually transmitted diseases should be suspected and treated appropriately in adolescents and adults (see Chapter 83). Candidal infections, with their typical white cheesy exudate, are often associated with diabetes mellitus and can be treated with a single dose of fluconazole (Diflucan), 200 mg PO.
 When infection is not a problem, phimosis can be successfully treated with a steroid cream (0.1% triamcinolone or 0.6% betamethasone), 4 times daily, with a gentle stretch on the foreskin for 2 to 6 weeks. After the phimosis resolves, the foreskin should be retracted daily to prevent recurrence.
When infection is not a problem, phimosis can be successfully treated with a steroid cream (0.1% triamcinolone or 0.6% betamethasone), 4 times daily, with a gentle stretch on the foreskin for 2 to 6 weeks. After the phimosis resolves, the foreskin should be retracted daily to prevent recurrence.
 Instruct parents in the technique and importance of proper cleaning of their son’s prepuce. Have them place him in a tub of warm water to alleviate dysuria.
Instruct parents in the technique and importance of proper cleaning of their son’s prepuce. Have them place him in a tub of warm water to alleviate dysuria.
 In both paraphimosis and phimosis, follow-up care should be provided. When swelling and inflammation subside, circumcision should be considered.
In both paraphimosis and phimosis, follow-up care should be provided. When swelling and inflammation subside, circumcision should be considered.
What Not To Do:
 Do not confuse paraphimosis with, or overlook, a circumferential foreign body (such as a hair or rubber band).
Do not confuse paraphimosis with, or overlook, a circumferential foreign body (such as a hair or rubber band).
 Do not attempt forced retraction when treating phimosis. Forceful retraction causes future adhesions and strictures.
Do not attempt forced retraction when treating phimosis. Forceful retraction causes future adhesions and strictures.
 Do not obtain unnecessary studies. Diagnosis is made by history and physical examination, although a radiograph may be useful if a constricting foreign body is suspected.
Do not obtain unnecessary studies. Diagnosis is made by history and physical examination, although a radiograph may be useful if a constricting foreign body is suspected.
Discussion
Poor hygiene and chronic inflammation are the usual causes of stenosing fibrosis of the preputial opening. It can be normal for boys up to 5 years of age not to be able to retract the foreskin completely. Repeated inflammation, even through tension on a minimally restrictive aperture from normal erections, may exacerbate the fibrosis and lead to phimosis. Vitamin E cream and topical steroid ointments may help soften a phimotic ring. When phimosis results in acute urinary retention, the tip of a hemostat can be inserted into the scarred end of the foreskin and gently opened, allowing the patient to void satisfactorily until urologic consultation can be obtained.
In the case of neglected paraphimosis, arterial occlusion may supervene, and ischemia, skin necrosis, and, eventually, gangrene of the glans develop. One common iatrogenic cause of paraphimosis is negligence in reducing the foreskin after retracting it to clean the glans and insert a Foley catheter.

Full access? Get Clinical Tree



