Fig. 87.1
Chest X-ray on admission showing cardiomegaly without significant pulmonary congestion
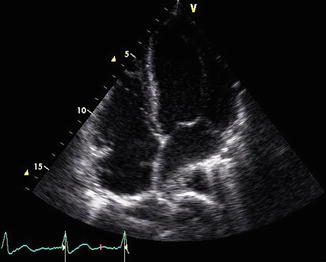
Fig. 87.2
Trans-thoracic echocardiogram 4-chamber view showing enlargement of both left and right ventricles consistent with a dilated cardiomyopathy
The patient was discharged to a skilled nursing facility. Guideline directed medical therapy was optimized as an outpatient as tolerated based on heart rate and blood pressure measurements. Transthoracic echocardiogram repeated 3 months post hospitalization revealed normal left ventricular dimensions, only mildly reduced left systolic function (LVEF 50 %), mildly reduced right ventricular systolic function, no significant valvular disease, and borderline elevated pulmonary pressures of 40 mmHg.
Question
What is her diagnosis and her treatment regimen?
Answer
Peripartum Cardiomyopathy
Peripartum cardiomyopathy (PPCM) is defined as (1) the new development of cardiomyopathy in a previously healthy woman in the final month of gestation or up to 5 months postpartum; (2) demonstration of left ventricular systolic dysfunction (ejection fraction < 45 %, and/or fractional shortening < 30 %, end-diastolic dimension > 2.7 cm/m2) and; (3) the absence of an identifiable cause or any prior heart disease [1]. The overall incidence is relatively low, less than 0.1 % of pregnancies, and the majority of patients present in the first 4 months postpartum and are in the upper or lower end of the child bearing age. The etiology of PPCM may be multi-factorial and it remains a diagnosis of exclusion. A familial predisposition has been reported. Viral myocarditis has been proposed and supported by findings of myocyte edema, necrosis, fibrosis and lymphocytic infiltration on myocardial biopsy. A pathologic immune response to fetal cells in the maternal myocardium after delivery (micro-chimerism), exaggerated mal-adaptive hemodynamic response during pregnancy characterized by increased cardiac output, decreased afterload, left ventricular hypertrophy and dysfunction, excessive secretion of prolactin, increased pro-inflammatory cytokines, mal-nutrition and selenium deficiency, and prolonged use of tocolytic drugs have all been proposed as mechanisms contributing to the development of PPCM [2].
Symptoms of PPCM include progressive dyspnea, orthopnea, cough, unintentional weight gain or retention of weight post-partum, and peripheral edema. If mild, these same symptoms may be attributed to physiological changes of pregnancy resulting in a delay in the diagnosis. One series demonstrated a significant correlation between major adverse event rates and several weeks’ delay in diagnosis; therefore heightened awareness is crucial [3]. Chest discomfort and palpitations are common and may be due to dysrhythmias. There is a higher incidence of systemic embolization in PPCM. Historical clues indicative of thromboembolic phenomena include transient loss of vision, aphasia, dysphagia, asymmetric lower extremity edema, digital cyanosis, abdominal pain and decreased urine output.
Risk factors associated with the development of PPCM include African American race, advanced maternal age, multiparity, multigravidity, tocolysis, gestational hypertension or preeclampsia [3, 4]. Major adverse events are more common in non-Caucasian women, initial left ventricular ejection fraction ≤25 % and delay in diagnosis, and are attributed to the development of left ventricular thrombus, ventricular arrhythmias, and refractory heart failure [3]. Complications and long term effects include cardiac arrest, thromboembolic events, limb ischemia, neurological deficits, and use of temporary or permanent mechanical circulatory support devices, death, and heart transplantation (Table 87.1). Patients who have suffered a neurological insult have residual long-term morbidity [3–5].
Table 87.1
Maternal risk factors and adverse events in PPCM
Maternal risk factors | Major adverse events | Long term effects of major adverse events |
|---|---|---|
Advanced maternal age African American race Non-Caucasian ethnicity Multiparity Multigravidity Twin pregnancy Poor socioeconomic status Gestational Hypertension Pre-eclampsia | Cardiopulmonary arrest Refractory heart failure Atrial fibrillation or flutter Ventricular Arrhythmia Cerebrovascular accident Limb ischemia | Death Permanent pacemaker Implantable cardioverter defibrillator Temporary mechanical circulatory support Left ventricular assist device Heart transplantation Neurologic deficits |
PPCM patients who recover their left ventricular systolic function have a good prognosis. Evidence suggests that 30–50 % of patients can fully recover left ventricular function on optimal medical therapy. There is a risk for recurrence of PPCM among these patients with subsequent pregnancies [6]. The precise risk is difficult to predict, and there are no guidelines on this issue. PPCM patients with persistent left ventricular dysfunction are clearly at risk for recurrence with subsequent pregnancies. They are also at high risk for premature births and spontaneous abortions. These patients should be strongly counseled against future pregnancies. Patients who fully recover their cardiac function have a 20 % risk of relapse with subsequent pregnancies. Patients who have a normal cardiac contractile reserve on an exercise echocardiogram may be at an even lower risk for relapse with subsequent pregnancy. These patients could undergo another pregnancy under careful monitoring with serial echocardiograms, and NT pro-BNP measurements without a relapse of PPCM. It is also not clear if women who fully recover their cardiac function can safely discontinue their heart failure therapy without the risk of decline in their LVEF. In the absence of guidelines, most physicians tend to continue medical therapy in recovered patients. Reported mortality worldwide in PPCM ranges between 5 and 32 % [7, 8]. Patients who present in severe heart failure or shock have a higher mortality. Mortality is also threefold higher in patients who have a fractional shortening of <20 % and a left ventricular end-diastolic dimension of >6 cm at initial presentation. Mortality rates have improved in recent years with early diagnosis and implementation of guideline based medical therapy.
Principles of Management
Diagnosis
Initially, the clinician must to perform a careful bedside clinical assessment looking for signs of hypoperfusion or signs of congestion that will help to identify the hemodynamic profile of the patient [9]. Signs of hypoperfusion include: cool extremities, altered mental status, decreased pulse pressure and renal insufficiency, while signs of congestion include: jugular venous distention, lower extremity edema, rales on auscultation. In most cases, the clinical evaluation will be enough to define the hemodynamic profile of the patient. However, sometimes invasive monitoring with pulmonary artery catheterization may be necessary to make the diagnosis and guide therapy, although there are no studies that compare invasive hemodynamic monitoring plus treatment versus standard of care alone in this population [10]. Once the hemodynamic profile of the patient has been established, the therapy will be guided to relieve congestion and/or improve cardiac output.
Initial assessment in PPCM should include transthoracic echocardiography to evaluate cardiac size and function, and investigate the presence of a left ventricular thrombus which is not uncommon [1]. Cardiac magnetic resonance (CMR) provides a more accurate measurement of both ventricular volumes, ejection fraction, and has a higher sensitivity for the detection of a left ventricular thrombus. Late gadolinium enhancement and T2 weighted imaging can provide important diagnostic information regarding inflammation or myocarditis and fibrosis. Depending on concomitant co-morbidities and maternal age, assessment for ischemia should be made with coronary angiography or stress testing.
Electrocardiogram findings include sinus tachycardia, left ventricular hypertrophy and ST-T wave repolarization abnormalities [11]. Patients may present with supraventricular or ventricular arrhythmias or cardiac arrest, as observed in patients with any form of cardiomyopathy. The electrocardiogram can help differentiate other causes of acute heart failure, including myocardial infarction or ischemia, cardiac tamponade, pulmonary embolus, mitral stenosis, or hemodynamically significant dysrhythmias.
Laboratory investigation includes measurement of NT-pro brain natriuretic peptide (NT-proBNP) or brain natriuretic peptide (BNP). The median serum levels of NT-proBNP observed in the first week postpartum after a normal pregnancy is typically about 100 ng/mL but can reach levels up to 700 ng/mL. This is attributed to increased venous return and preload after decompression of the IVC at childbirth [12–14]. However, in peripartum cardiomyopathy NT-proBNP levels are significantly higher with levels in the range of nearly 1000–3000 ng/mL [14].
Differential diagnoses should guide other diagnostic investigations including left heart catheterization and cardiac biomarkers if there is a suspicion of pregnancy-associated myocardial ischemia or infarction, ventilation-perfusion scanning or CT pulmonary angiogram and D-dimer if pulmonary embolus is suspected, and checking HIV assays as a potential cause for non-dilated cardiomyopathy [5]. Ultimately imaging modalities and laboratory data are complementary to a thorough physical examination and invasive hemodynamic assessment may be needed for directed therapeutic approach (Table 87.2).
Table 87.2
Diagnosis of PPCM
Clinical suspicion | Symptoms and signs | Diagnostic studies |
|---|---|---|
Previously healthy woman with new onset heart failure in the last month of gestation or first 4 months post-partum Risk factors for PPCM Family History | Dyspnea at rest or exertion Fatigue Exercise intolerance Edema Chest pain Palpitations Cough Weight gain Weakness Jugular venous distension Tachycardia S3 or S4 gallop | Complete blood count and differential Complete chemistry BNP or NT-proBNP Cardiac troponin-T (if needed) Chest X-ray (if needed) EKG Transthoracic echocardiogram CMR Endomyocardial biopsy (if indicated) |
Standard Medical Therapy for Heart Failure
The medical therapy for acute decompensated heart failure in peripartum cardiomyopathy is the same as to those patients with acute systolic heart failure from other etiologies (Table 87.3). In general, oxygen should be administered to patients with oxygen saturations lower than 90 %. If the patient is in distress, they should be promptly intubated and placed on mechanical ventilation to reduce the work of breathing. For patients with pulmonary congestion, especially those who present with pulmonary edema, the use of intravenous diuretics will help with immediate relief of the symptoms. Loop diuretics should be used cautiously in the antepartum period as precipitous decreases in blood pressure from a large diuresis can compromise placental blood flow. Thiazide diuretics may be a useful alternative in these patients. Vasodilators like, nitroglycerine, nitropusside and nesiritide can be used in combination with diuretic therapy and will help to decrease preload and afterload in those patients who present with elevated blood pressures. However, these medications should be avoided in patients with systolic blood pressure less than 100 mmHg. Inotropes like dobutamine and milrinone are indicated in patients who present with decreased perfusion or in cardiogenic shock in order to improve the cardiac output and maintain adequate organ perfusion. Other inotropic drugs like levosimendan, although used extensively in other countries, are not approved in the United States [5]. The use of vasopressors like norepinephrine, epinephrine and dopamine is associated with an increase in afterload and a subsequent decrease in the cardiac output and their use should be restricted to patients with marked hypotension despite adequate filling pressures and cardiac output.








