Chapter 54
Pericardial Tamponade
Function of the Pericardium
The function of the pericardium remains a puzzle, and the congenital absence of the pericardium has no adverse effect on survival or exertional capacity. A number of roles have been suggested, including prevention of excessive dilatation of the heart, prevention of adhesions to surrounding chest structures, and maintenance of the heart in a stable geometric position within the chest. Although the pericardium does prevent distention of the heart under artificial fluid loading conditions in animals, the relevance of this to humans is questionable. An additional proposed role may be to maintain a stable diastolic coupling between the left and right ventricles over a range of hemodynamic states.
Causes of Pericardial Effusion
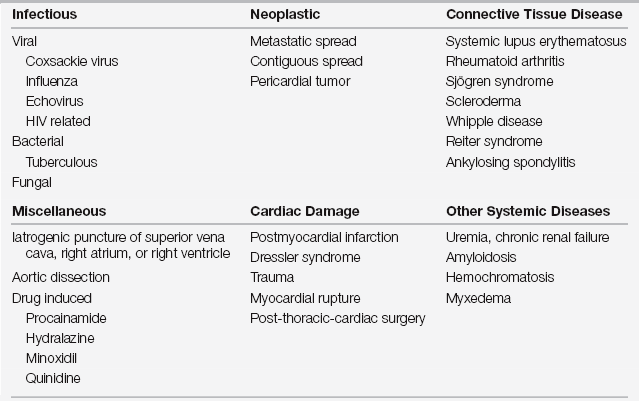
Fluid accumulation within the pericardial space is a prerequisite for the development of cardiac tamponade with rare exception, such as massive pleural effusions, tension pneumothorax, or pneumopericardium. Because the native pericardium is generally stiff and noncompliant, in the acute setting as little as 100 to 200 mL of fluid can cause tamponade. In the chronic setting, pericardial effusions may contain up to 2 L of fluid without tamponade, owing to slow distention of the fibrous sac. Fluid may accumulate within the pericardium as a result of infection or inflammation of the pericardium (serositis, pericarditis) or from neoplastic disorders. Iatrogenic causes include hemopericardium caused by central venous catheter perforation, a puncture of the right atrium or ventricle by a pacemaker wire, or a prior endomyocardial biopsy. Purulent pericarditis results from bacterial infection of the pericardium and is characterized by a syndrome of fever, chest pain, and a pattern often suggestive of pericarditis on the electrocardiogram. Blood or thrombus in the pericardium after trauma or thoracic surgery may also result in tamponade (Table 54.1).
Diagnosis
Tamponade should be suspected in any patient with unexplained hypotension. A change in mental status or the onset of oliguria may be early signs of systemic hypoperfusion. An enlarged cardiac silhouette on chest radiograph or changes consistent with pericarditis on the electrocardiogram (ECG) may be early clues, which, although nonspecific, should prompt the clinician to exclude tamponade as a contributing etiology.
Physical Examination
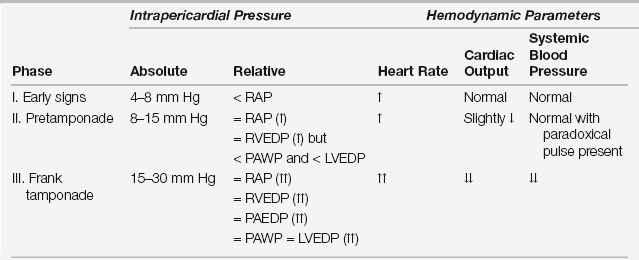
Early signs of increased intra-pericardial pressure include tachycardia without hypotension and a slightly increased respiratory rate (Table 54.2). Paradoxical pulse (pulsus paradoxus) develops later and refers to a decline in systolic blood pressure of more than 15 mm Hg on inspiration. In the setting of tamponade the heart has a “fixed volume,” such that inspiratory-driven increases in venous return to the right ventricle reduce left ventricular outflow via compression of the left ventricle between the septum and pericardial fluid. Though highly sensitive for cardiac tamponade, pulsus paradoxus is not a specific finding and occurs with other common intensive care unit (ICU) conditions such as advanced obstructive airway disease or positive pressure ventilation.
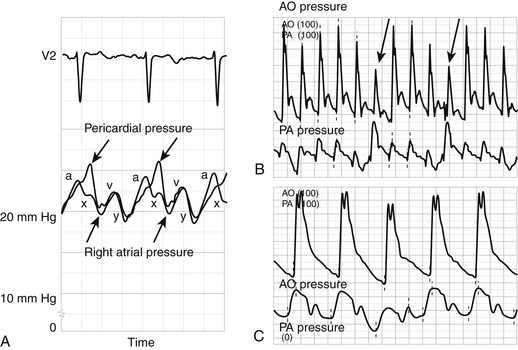
Jugular venous distention is a nearly constant finding with cardiac tamponade, but it is also evident in other conditions frequently encountered in the ICU. Although subtle, identifying the contour of the jugular venous pulse should be attempted, as the attenuation (or absence) of the y descent is an early sign of impaired diastolic filling (Figure 54.1). The heart sounds may be muffled but are usually audible, and a pericardial friction rub may be heard or palpated.
< div class='tao-gold-member'>

Full access? Get Clinical Tree