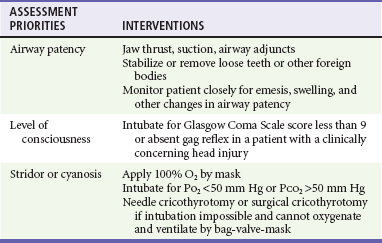
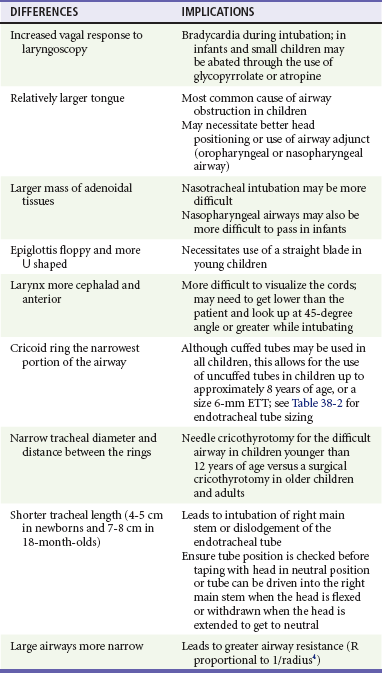
Chapter 38 Injuries to children (<18 years old) account for more than 8 million visits to emergency departments in the United States each year. More than half of all deaths in this age group are the direct result of injury, with more than 10,000 traumatic deaths annually.1 Motor vehicle collisions (MVCs) account for more than half of all pediatric traumatic deaths.1 In the United States, estimates of mortality for children hospitalized after injury are uniformly low; however, most fatalities occur in the field before arrival at a health care facility, which contributes to an underestimation of the magnitude of overall mortality figures. Multiple injuries are common in pediatric trauma patients, and the emergency physician should evaluate all organ systems in any injured child when the mechanism of injury is concerning. The most common single organ system injury associated with death in injured children is head trauma, but the great majority of pediatric trauma deaths involve multisystem injury.2 Accidental falls predominate nonfatal injuries in all pediatric age groups. Other nonfatal injuries vary by age. Young children (<4 years of age) experience higher rates of animal bites and burns. School-age children (5 to 9 years old) are more likely to experience bicycle and pedestrian injuries. Older children (>9 years) have high incidences of both fatal and nonfatal motor vehicle–related trauma, and higher incidences of suicide and self-inflicted harm. Homicide by firearm shows a fourfold and tenfold increase when the 5- to 9-year age group is compared with the 10- to 14- and 15- to 24-year age groups, respectively. Homicide by firearm is nearly 31 times more common in the 15- to 24-year age group when compared with the 10- to 14-year age group.1,2 Throughout the United States the number of children who are victims of violent acts has increased. Some children’s hospitals report that 7% of all pediatric injuries seen in emergency departments and 25 to 35% of all pediatric trauma deaths are caused by nonaccidental trauma.3 Between pediatric and adult patients, there are major anatomic and physiologic differences that play a significant role in the evaluation and management of a pediatric trauma patient (Box 38-1). Any given force is more widely distributed through the body of a child than the body of an adult, making multiple injuries significantly more likely to occur in children. The proportionately large surface area of infants and children relative to weight predisposes them to greater amounts of heat loss as a result of evaporation. During resuscitation, even mild to moderate hypothermia has direct negative effects on cardiac function, inotropy, left-ventricular contractility, catecholamine responsiveness, platelet function, renal and hepatic drug clearance, and metabolic acidemia. Therefore maintenance requirements for free water, electrolytes, and minerals are proportionally greater compared with those for adults. Oxygen extraction and consumption as well as glucose utilization are much higher per kilogram in infants and small children than in adults. These factors contribute to a significantly higher energy and caloric requirement for an injured child compared with an injured adult. A child’s physiologic response to injury is different from an adult’s response, depending on the age and maturation of the child and the severity of the injury. Children have a great capacity to maintain blood pressure despite significant acute blood losses constituting 25 to 30% of total blood volume.4 A child’s cardiac output is primarily determined by the heart rate and systemic vascular resistance. Changes in inotropy play a relatively minor role in children after trauma, compared with adults. Compensated shock should be considered and promptly addressed when a child’s heart rate is elevated, especially if the capillary refill time is delayed. Changes in heart rate, blood pressure, and extremity perfusion commonly precede cardiorespiratory failure and should not be overlooked. Initial Assessment Priorities and Primary Survey Table 38-1 describes anatomic considerations that have implications in the management of the pediatric airway. The physician assesses for possible airway obstruction or inability of the child to maintain his or her own airway. While the neck is being stabilized, the airway can be opened with a jaw-thrust maneuver. Maxillofacial trauma, loose teeth, blood, swelling, or vomitus may obstruct the airway, and efforts should be made toward clearing the oropharynx of debris. Gurgling or stridor may indicate upper airway obstruction. The physician must know normal pediatric oral anatomy and tooth development to recognize the possibility of missing primary or secondary teeth. Efforts to perform cricoid pressure, or ligatures such as ties on gowns, can easily occlude the infant’s or child’s airway with as little as 0.2 pounds of direct force.5 Table 38-2 describes priorities in the assessment of the pediatric airway. Table 38-2 Airway: Assessment and Treatment O2, oxygen; PCO2, partial pressure of carbon dioxide; PO2, partial pressure of oxygen. Intubation of pediatric patients involves special considerations (see Table 38-1). In general, the orotracheal approach is recommended. In children, nasotracheal intubation can be complicated by the acute angle of the posterior pharynx, the potential for bleeding, and infection (sinusitis). Furthermore, nasotracheal intubation can cause increased intracranial pressure (ICP). In children younger than age 8, the cricoid ring is the narrowest portion of the airway. The cricoid ring may form a physiologic cuff on endotracheal tubes (ETT). However, the use of a cuffed tube allows for greater airway protection and may be considered in the injured child. Appropriate ETT size can be estimated through use of a length-based resuscitation tape or by the formulas in Box 38-2. For assessment of “ventilation,” pulse oximetry is useful; however, pulse oximetry measures adequacy of oxygenation only. The measurement of exhaled carbon dioxide (CO2) is useful to confirm ETT position. Historically, a colorimetric semiquantitative device has been used to detect the presence of exhaled CO2 in patients with perfusion. Continuous end-tidal CO2 capnography provides far more information and continues to be underused.6 In a patient with adequate perfusion, in addition to serving as an initial qualitative device to confirm successful intubation of the trachea, it may also provide an early warning of unintended extubation, tube kinking or partial occlusion, or ventilator malfunction. Continuous end-tidal CO2 capnography also characterizes the response to therapeutic maneuvers instantaneously, provides a quantitative tool to manage the ventilatory aspects of respiration, and may provide prognostic information when used in patients with cardiac arrest. It can also be used to measure the effectiveness of cardiopulmonary resuscitation (CPR). The lack of appropriate CO2 detection when the tube is in proper position often indicates poor perfusion. The use of end-tidal CO2 capnography allows better ventilatory management during head injury resuscitation, and its values can be confirmed with a single venous or arterial blood gas measurement. This can assist greatly with continuing ventilatory management without the need for recurrent blood draws and the inherent delays and discomfort of acquiring blood gases (assuming stable pulmonary function). Table 38-3 describes priorities in the assessment of breathing in pediatric trauma patients. Shock is not defined by any specific blood pressure but is, instead, a state in which the body is unable to maintain adequate tissue perfusion. Maintenance of systolic blood pressure does not ensure that the patient is not in shock. The pediatric vasculature has the ability to constrict and increase systemic vascular resistance in an attempt to maintain perfusion. Signs of poor perfusion (cool distal extremities, decreases in peripheral versus central pulse quality, and delayed capillary refill time) are signs of pediatric shock, even when blood pressure is maintained at normal levels. Palpable pulses are detectable at a systolic blood pressure greater than 80 mm Hg in children over approximately 10 years of age; however, pulses may be felt at even lower pressures in infants and younger children. Normal capillary refill time is less than 2 seconds; however, many variables affect this clinical finding. Alteration in a child’s response to the environment or interaction with caregivers may indicate respiratory failure or shock. External hemorrhage should be sought and controlled with direct pressure. The assessment of circulation in pediatric trauma patients is described in Box 38-3. For assessment of patient disability, a rapid neurologic and mental status evaluation is needed. The assessment of disability in pediatric trauma patients is described in Box 38-4. The AVPU system (Box 38-5) and the modified pediatric GCS (Table 38-4) can also be useful to the clinician. Fully undressing the patient to assess for hidden trauma is essential in injured children. Maintenance of normothermia is paramount in the undressed infant and toddler because metabolic needs are greatly increased by hypothermia. In addition to increased ambient temperature, additional warming methods such as warmed humidified oxygen, warmed fluids, warmed blood, head wraps, and convective warmers or radiant heat sources should be used as soon as possible. Preventing and treating hypothermia is not a matter of comfort for traumatized infants and children but, instead, one of survival. The exposure phase of the survey is often a good time to concurrently begin imaging and further diagnostic testing (Table 38-5). The focused assessment with sonography in trauma (FAST) can be a very useful examination in injured children.7 Bedside ultrasound evaluates for traumatic free fluid in the peritoneum (hepatorenal, perisplenic, and retrovesicular views) and pericardial space. In hemodynamically unstable children, a FAST may point to hemorrhage in the abdomen or the pericardial space and the need for intervention. In hemodynamically stable children, the FAST examination may indicate the need for computed tomography (CT) imaging, closer observation, repeat abdominal examinations, or repeat ultrasound examinations. After completion of the primary survey and requisite procedures, the secondary survey is performed. The secondary survey is an organized, complete assessment to detect additional injury not found on the primary survey. A more complete and detailed history is obtained at this time. Features of the history that need to be obtained can be remembered by the mnemonic AMPLE (Box 38-6). Ongoing assessment of the patient occurs after the secondary survey, and key points are summarized in Box 38-7. All pediatric patients who have sustained major trauma should be placed on a cardiac monitor; receive supplemental oxygen; and have constant reassessment of vital signs, oximetry, and end-tidal CO2 monitoring. Vascular access is best obtained by accessing the upper extremity for the establishment of two large-bore intravenous lines. In the absence of available upper extremity peripheral sites, lower extremity sites can be used. Many clinicians favor the femoral vein as a safe site for insertion of a central line by use of a guidewire technique. A guide to suggested sizing of femoral catheters is shown in Box 38-2. Most hypovolemic pediatric trauma patients respond to 20-mL/kg boluses of isotonic crystalloid solutions. If 40 mL/kg has not reversed systemic signs of hypoperfusion, an additional 20-mL/kg bolus of crystalloid may be given, but the infusion of packed red blood cells at 10 mL/kg should be considered. In patients in decompensated hemorrhagic shock or cardiopulmonary failure secondary to severe anemia, crystalloid and blood products may be prudently administered simultaneously. With massive transfusion (>1 blood volume = approximately 80 mL/kg), it is important to add additional blood products to correct coagulopathy. Some experts now recommend (based predominantly on adult studies) that blood and fresh frozen plasma (FFP) be given in a near 1 : 1 ratio if massive transfusion is expected. Other experts believe a ratio closer to 2.5 : 1 may suffice and may decrease the risk of multiorgan failure. In general, FFP should be administered at 15 to 25 mL/kg. Platelet transfusion dosage can be very confusing. Practically all platelet units currently used are apheretic platelets from a single donor. Each apheretic unit roughly equates to six of the older concentrate units (a “six-pack” of platelets). The usual dose in trauma is 10 mL/kg; however, the response may be quite variable (i.e., it can vary by more than a factor of two) owing partly to the heterogeneity of the concentration of platelets between apheretic units. A general goal in trauma patients is to raise the platelet count above 50 × 109/L. The platelet count should be rechecked at 1 and 24 hours after transfusion, or more often if the patient has ongoing difficulties with hemostasis or need for recurrent transfusion of red blood cells. The primary goal of giving cryoprecipitate is to increase the fibrinogen to levels of 1 to 1.5 g/dL, especially after central nervous system trauma. Although dependent on the fibrinogen concentration in the individual cryoprecipitate bags, the dose is typically 0.1 to 0.2 bags/kg. Each bag of cryoprecipitate contains approximately 150 mg of fibrinogen and 80 units of factor VIII.8 A rectal examination is not required in all cases of pediatric trauma and should be performed only when its result has a reasonable chance of meaningfully changing the patient’s treatment.9,10 A rectal examination may provide information on sphincter tone in possible spinal injury and the presence of blood in penetrating trauma. Unfortunately, the rectal examination lacks sensitivity. Its findings, when negative, are often misleading, and additional workup should be considered. Reexamination of trauma patients throughout their time in the emergency department is of utmost importance to ensure that their condition has not changed, that their pain is controlled, and that no injuries are overlooked. Up to 70% of injuries with delayed diagnosis in pediatric trauma are orthopedic in nature.11 In patients with hypovolemic shock, the hemoglobin alone is unreliable because equilibration will not have occurred at the time of presentation to the emergency department.12 Serial hemoglobin measurements may be useful to assess the possibility of ongoing bleeding.13 Chest and pelvic radiographs can assess for causes of respiratory failure, sites of blood loss, and causes of shock. In stable, alert children without distracting injuries, the pelvic film may be eliminated if no suggestion of sacral or pelvic fracture is found on thorough clinical examination. The following seven criteria are required to rule out any relevant pelvic fracture: patient age older than 3 years, no impairment of consciousness, no other major distracting injury, no complaint of pelvic pain, no signs of fracture on inspection, no pain on iliac or pubic symphysis compression, and no pain on hip rotation or flexion.14–16 In patients with remarkable sacral tenderness and negative plain radiographs, a CT scan should be strongly considered. Sacral fractures can be difficult to discern reliably on plain films. Each year, more than 500,000 children (ages 0 to 14 years) visit emergency departments in the United States after head injury.17 Falls account for 50.2% of pediatric head injuries. On an age-related basis, infants and toddlers are more prone to falls from their own height, school-age children are involved in sports injuries and MVCs, and children of all ages are subject to the sequelae of abuse. Although MVCs account for only 6.8% of pediatric head injuries, they represent more than 30% of fatal head injuries.17 The prognostic significance of vomiting after pediatric head trauma is unclear. There is no adequate study defining an acceptable time frame in which vomiting after head injury is benign in nature. Vomiting appears to be more strongly correlated to personal or familial tendency to vomit than to intracranial injury; however, recurrent vomiting is commonly seen in patients with significant head injury and is often considered in the decision to obtain a CT study.18 The development of seizures after head trauma has been well studied.19 A brief seizure that occurs immediately after an insult (with rapid return to normal level of consciousness) is commonly called an impact seizure. This type of seizure is not usually associated with intracranial parenchymal injury. A CT scan is not necessary if the only concern is the impact seizure; the decision to scan should take into account the mechanism of injury and current neurologic status of the child. An isolated impact seizure does not require anticonvulsant therapy. Seizures that occur later (more than 20 minutes after the insult) portend the greater possibility of traumatic brain injury and the development of seizures at a later date. A CT scan is indicated for these later post-traumatic seizures. These patients may benefit from treatment with anticonvulsants, benzodiazepines for sedation if intubated, or both as the seizure threshold is generally lower in children. Having one later seizure (nonimpact) raises the risk of subsequent additional seizure, and seizure activity raises ICP while often decreasing oxygenation and ventilation. Children who experience later seizures often require neurosurgical evaluation. Several methods are available for evaluating the mental status of head-injured patients, including the AVPU system and the GCS. A commonly used modification of the GCS for children is shown in Table 38-4. Although the pediatric GCS is widely used, none of the pediatric modifications of the GCS has the inter-rater reliability or predictive validity of the adult GCS. Even children with low initial GCS scores can have favorable outcomes and neurologic status. The important message is that no matter what the patient’s neurologic presentation, all efforts should be initiated to ensure survival and maintain stable neurologic status in the emergency department. Examining a brain-injured child involves mental status testing, cranial nerve testing, motor testing, sensory testing, and memory testing. The evaluation of cranial nerve function is essentially no different from that in an adult. The most important aspect of motor and cranial nerve evaluation involves ruling out the presence of increased ICP. Common symptoms and signs of increased ICP in infants and children should be sought (Boxes 38-8 and 38-9).
Pediatric Trauma
Perspective
Principles of Disease
Clinical Features
A—Airway and Cervical Spine Stabilization
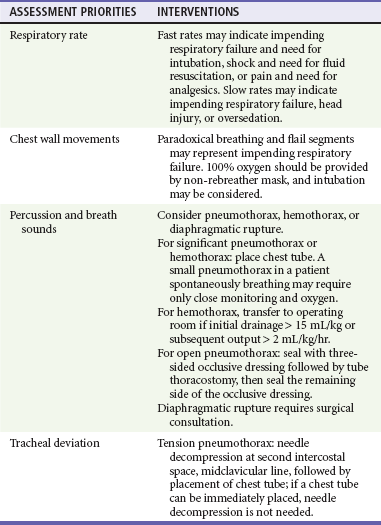
B—Breathing and Ventilation
C—Circulation and Hemorrhage Control
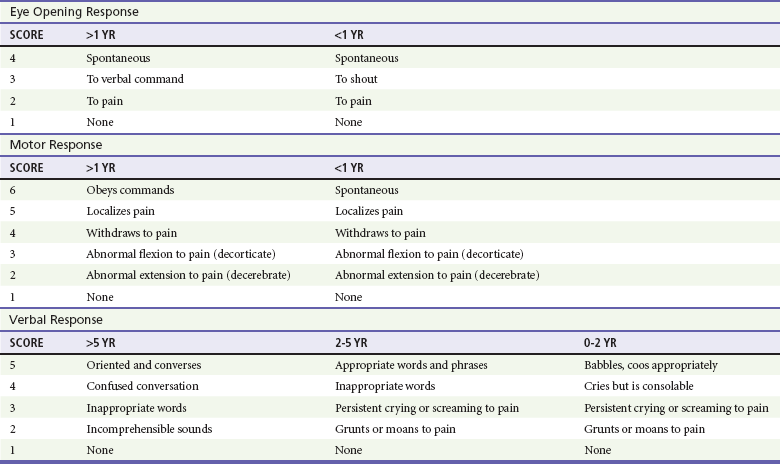
D—Disability Assessment (Thorough Neurologic Examination)
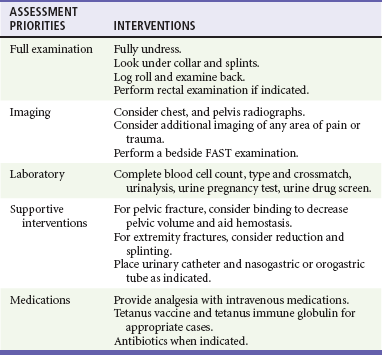
E—Exposure and Thorough Examination
F—FAST and Family
Secondary Survey
Management and Diagnostic Strategies
Physical Examination
Diagnostic Evaluation
Radiology
Specific Disorders and Injuries
Perspective
Clinical Features

Full access? Get Clinical Tree


Pediatric Trauma

 kg+ = 3-3.5 mm
kg+ = 3-3.5 mm