Pediatric Emergencies: Introduction
Children constitute one of the most diverse and challenging patient populations facing the emergency physician. While comprising almost 30% of emergency department patients, critical illness and injury are present in only approximately 5%. The majority of pediatric emergency visits are evaluated not in pediatric hospitals, but community emergency departments. Early recognition and aggressive management of illnesses and injuries effecting pediatric patients is of utmost importance.
The epidemiology of pediatric emergency medicine changes with the clinical setting. In the prehospital environment, the common presenting complaints are trauma, seizures, respiratory distress, and toxicologic emergencies. In the emergency department, the most common complaints are fever, trauma, injury, respiratory distress, vomiting, diarrhea, or upper respiratory tract infection.
Assessment of the pediatric patient in the emergency department requires an age-specific approach. A calm, reassuring, and gentle manner on the physician’s part will facilitate information collection and encourage patient cooperation in examining and testing.
Knowledge of the child’s growth and development often is required for the diagnosis, management, and disposition of the pediatric patient. Severity of acute pediatric illness and injury is often difficult to discern. Recognition of anatomic and physiologic differences remind the examiner of large surface area to weight ratio leading to heat loss and trauma to internal organs may exist with little signs of external injury. Airway differences are important to understand in order to manage respiratory distress and failure. Observational methods of assessment may be more sensitive to illness and injury acuity in children taking into account such variables as quality of cry, reaction to parent stimulation, state variation, skin color, hydration status, and response social overtures such as talking and smiling. Such observations appear to be more predictive of serious illness than anatomic physical examination using standard palpation, percussion, and auscultation techniques.
Assessment and management of the distressed pediatric patient requires appropriately sized equipment. Table 50–1 provides equipment sizes for invasive procedures in children of different age groups.
| Age | Weight (Kg) | Endotrachel Tube | Laryngoscope Blade | Chest Tube (F) | Nastrostic Tube (F) | Foley Catheter (F) | Femoral IV |
|---|---|---|---|---|---|---|---|
| Premie 32 week gestation | 2 | 2.5–3.0 | 1 straight | 8 | 5 | 5 | 3 F, 8 cm |
| Newborn | 3 | 3.5 | 1 straight | 10 | 5 | 8 | 3 F, 8 cm |
| 1 month | 4 | 3.5 | 1 straight | 10 | 5 | 8 | 3 F, 8 cm |
| 3–5 months | 6–7 | 3.5 | 1 straight | 10–12 | 5–8 | 8 | 3 F, 8 cm |
| 6–11 months | 8–10 | 3.5–4.0 | 1 straight | 10–12 | 8 | 8–10 | 3 F, 8 cm |
| 1 year | 10–11 | 4.0 | 1 straight | 16–20 | 8–10 | 8–10 | 3 F, 8 cm |
| 2–3 years | 12–14 | 4.5 | 1.5–2 straight | 20–24 | 10 | 8–10 | 5 F, 15 cm |
| 4–5 years | 15–18 | 5.0 | 2 straight or curved | 20–28 | 10–12 | 10–12 | 5 F, 15 cm |
| 6–8 years | 20–28 | 5.5–6.0 | 2 straight or curved | 30–32 | 14–18 | 10–12 | 5 F, 15 cm |
| 10–12 years | 35–50 | 6.5–7.0 | 3 straight or curved | 32–38 | 18 | 12 | 5–7 F, 15–20 cm |
| 14 years | 60 | 7.0–7.5 | 3–4 straight or curved | 38–40 | 18 | 12 | 7 F, 20 cm |
Vital signs may vary by age (Table 50–2). A rapid formula for estimating normal systolic blood pressure is 80 + (2 × age [in years]). The maximum effective heart rate in infants is 200 beats/min, in young children 150 beats/min, and in school-aged children 120 beats/min. Respiratory rate decreases with advancing age (Table 50–2). The use of vital signs to assess vital functions in pediatric patients, however, is hazardous. Appropriate-sized measuring equipment is imperative, techniques must be applied carefully, and interpretation must be age-related. Furthermore, even accurately obtained, age-adjusted vital signs may be insensitive and are often affected by fever, pain, and ambient features of the emergency department environment. Instead, other measures of cardiopulmonary function, such as skin color, temperature, and capillary refill, are often better triage and assessment tools.
| Age | Mean Weight (kg) | Minimum Systolic Blood Pressure | Normal Heart Rate | Normal Respiratory Rate |
|---|---|---|---|---|
| Premature | 2.5 | 40 | 100–170 | 40–50 |
| Newborn | 3 | 50 | 90–180 | 30–50 |
| 3 months | 6 | 60 | 110–180 | 24–40 |
| 6 months | 8 | 70 | 110–17 | 24–40 |
| 1 year | 10 | 72 | 90–150 | 24–40 |
| 2 years | 13 | 74 | 90–150 | 22–30 |
| 4 years | 15 | 78 | 65–135 | 20–40 |
| 6–8 years | 20–28 | 80–86 | 60–130 | 18–24 |
| 9–10 years | 30–36 | 90 | 60–110 | 16–22 |
| 11–14 years | 50–60 | 90 | 60–110 | 14–20 |
The emergency department physician must appreciate the intimate relationship of the child to the family. Acute pediatric illness and injury are inextricably part of the family environment and dynamics. The child as well as the entire nuclear and extended family may experience major psychological, emotional, and financial consequences of pediatric emergencies. Effective care requires appropriate consideration of the child within the distressed family, enlistment of parental assistance in evaluation and management, and provision of psychological support.
Too often, the inexperienced physician neglects pain control or procedural sedation because of misunderstanding the significance of pain in the young child, unwarranted fear of addicting children to narcotic agents, or ignorance of appropriate agents. When a painful procedure is necessary, an effective approach integrates careful explanation directly to the child and enlistment of parental understanding and assistance. Whenever conscious or deep sedation procedures are performed, the emergency department physician must ensure patient’s safety by strict adherence to the guidelines of monitoring. This includes preparation for any potential airway complications, such as aspiration or apnea. In general, only previously healthy or mildly chronically ill children should be considered candidates for sedation procedures in the emergency department. Sometimes a restraint apparatus will facilitate the procedure.
The guidelines for a variety of clinical situations are given next.
| Drug | Components | Applied To | Effect (min) | Cautions |
|---|---|---|---|---|
| EMLA (Eutectic Mixture of Local Anesthetics) |
| Intact skin | 90 |
|
|
| Both intact and non intact skin | 30 |
|
| TAC |
| Both intact and nonintact skin | 15 |
|
| Viscous Lidocaine | Lidocaine 2% | Both intact and and nonintact skin | 10 | Max dose: 5 mglk Lidocaine |
The formulation LET (2% lidocaine, 1:1000 epinephrine, and 2% tetracaine) is easily applied and has a favorable safety profile. It is available as gel or solution. The onset of action is approximately 30 minutes; thus it should be applied early in the laceration evaluation process. TAC (tetracaine, adrenaline, and cocaine) is occasionally used as well; however caution should be used as seizures have been reported secondarily to systemic cocaine absorption. Any anesthetic containing epinephrine (such as LET or TAC) should be avoided on end-arterial structures, such as the ears, nose, digits, or penis. (See Table 50–3.)
Eutectic mixture of local anesthetics (EMLA) or Elamax 4%, ethyl chloride spray preparations, J-tip lidocaine applicators have been advocated for local analgesic use on intact skin.
There are numerous agents (Table 50–4) which are useful in sedation and pain management in the pediatric patient. Familiarity with several of these is useful for the emergency physician, allowing tailoring of the most appropriate agent to the clinical situation. The most commonly used agents are discussed next.
| Commonly Used Sedative/Analgesic Agents | |||||
|---|---|---|---|---|---|
| Agent | Route | Pediatric Dose | Onset | Duration | Comments |
| Sedation | |||||
| Propofol | IV | 1 mg/kg bolus: followed by 0.5 mg/kg every 3–5 min | 30–45 s | <15 min |
|
| Ketamine |
|
|
|
|
|
| Midazolam |
|
|
|
| |
| Nitrous Oxide | Inhaled | 50–70% Concentration | 1–2 min | 5 min | Vomiting in up to 10% |
| Analagesia | |||||
| Acetaminophen |
|
| 20–40 min | 4 h |
|
| Ibuprofen | PO | 10 mg/kg | 20–30 min | 6h |
|
| Hydrocodone | PO | 0.15–0.2 mg/kg | 10–30 min | 4–6 h | |
|
|
|
|
| Maximum dose 10 mg |
| Fentanyl |
|
|
|
| Chest wall rigidity with rapid infusion |
Midazolam is a relatively fast acting benzodiazepine providing anxiolysis, sedation, and antegrade amnesia, commonly used in emergency department sedation. It is commonly used in conjunction with a narcotic analgesic such as morphine or fentanyl. Some children will have a paradoxical excitation to midazolam and will experience agitation instead of sedation. There is some evidence that this unpleasant reaction may be reversed with flumazenil. Patients may also respond favorably to additional administration of benzodiazepines.
Ketamine, IM/ may be used for procedural situations involving children of any age, especially burn debridement, foreign body removal, deep wound care, abscess incision and drainage, or orthopedic reductions. Some clinicians recommend adding atropine, 0.01 mg/kg (maximum, 0.5 mg), or glycopyrrolate, 0.005 mg/kg (maximum 0.25 mg), to avoid hypersalivation, although current literature has not demonstrated a clear benefit. Intravenous administration is better for longer procedures. Ketamine may elevate intracranial and intraocular pressure, induce emesis, and occasionally precipitate laryngospasm. Ketamine use in older children may also cause an adverse behavioral reaction upon emergence from sedation. Some clinicians recommend the concomitant use of midazolam in children over 5 years. Studies, however, have not demonstrated a clear benefit to administering midazolam with ketamine to prevent emergence phenomenon.
Propofol, 0.5–1.0 mg/kg by slow IV injection over 3–5 minutes, followed by an infusion of up to 0.5 mg/kg over 2–3 minutes with at least 1 minute between infusions. The advantage to this drug is the rapid onset of sedation and quick recovery time. Propofol is easily titrated to appropriate level of sedation. As with other agents, respiratory depression can occur and therefore ability to manage the airway and assist ventilation is extremely important when using this agent. Common uses of propofol include sedation for orthopedic reduction and suturing. Because of the potential for allergic reaction, the drug is contraindicated in patients with egg or soy allergies. Although the clinical significance of the effect is often not apparent, blood pressure frequently drops during propofol infusion. For this reason, most clinicians avoid propofol in patients who have been hypotensive and/or are significantly hypovolemic.
For individuals requiring imaging studies such as computed tomography (CT) scan or magnetic resonance imaging (MRI), pentobarbital intramuscularly, midazolam, etomidate , methohexital or dexmedetomidine are commonly and safely used with proper monitoring as for any procedural sedation.
Sedation agents should only be used by those with appropriate training and familiarity with the agents used. Proper precautions should be taken such as constant vital sign and pulse oximetry monitoring. End-tidal CO2 monitoring is advised to more closely assess the adequacy of a patient’s ventilation. Rescue airway equipment and reversal agents such as naloxone, 0.01–0.1 mg/kg IV, and flumazenil, 0.01 mg/kg IV should be readily available.
Outpatient analgesia ordinarily includes a nonsteroidal, anti-inflammatory drug such as ibuprofen, 10 mg/kg every 6–8 hours. This drug can also be used in combination with oral narcotic agents for the treatment of severe pain. Acetaminophen, 10–15 mg/kg every 4–6 hours, can also be used for the treatment of mild pain on an outpatient basis. Narcotics as hydrocodone/acetaminophen combination or codeine/acetaminophen every 4–6 hours may be used for severe pain.
All parenterally and orally administered agents should be given strictly on a per-kilogram basis, until maximum adult doses and volumes are reached. Over dosing and over hydration are dangerous errors in emergency pediatrics. Under dosing is also frequent, especially in infants and small children. Initial treatment of dehydration should include isotonic fluids (normal saline or lactated Ringer’s). Physicians and nurses should meticulously review drug and fluid orders to ensure that they are age and weight corrected.
Vascular access is often the rate-limiting step in provision of life-saving therapy to critically ill and injured children. The emergency department physician must be familiar with a variety of techniques for access into the cardiopulmonary system.
In critically ill, intubated patients, the endotracheal route is an effective conduit for administration of a variety of life-saving drugs, including epinephrine, atropine, lidocaine, naloxone, and diazepam. Epinephrine is by far the most commonly used. When administered through the endotracheal tube, higher doses, up to 10 times the IV dose, must be used to obtain adequate serum concentrations. The pharmacokinetics of endotracheal epinephrine administration may be optimized by delivery of the drug directly into the highly vascular trachea and proximal tracheobronchial tree instead of directly into the endotracheal tube. The preferred technique required is the insertion of a nasogastric tube or a size 5F umbilical catheter past the distal tip of the endotracheal tube with direct instillation of drugs through the tube. Because endotracheal drugs may be more effective if aerosolized, dilute the drug with normal saline to a maximum volume of 0.5–1.0 mL/kg, and then inject rapidly to achieve a partially aerosolized form.
In infants, the scalp is an ideal site for cannulation; use a size 24 gauge IV catheter. In children past the neonatal period, the dorsal veins of the hand, antecubital fossa, or dorsum of the foot are usually accessible with a 24 or 22-gauge IV catheter. The external jugular vein is a large vein, usually easily visualized and readily cannulated with a 20-gauge catheter if the child is properly restrained and the head is held in a dependent position.
(See also Chapter 8.) For patients under age 5 years in extremis and requiring life-saving drug and fluid administration, intraosseous infusion is an alternative method of administration. This method of access is also a viable alternative in older children and adults; however, successful cannulization is more difficult in this population. A short, thick needle with a trocar tip is inserted into the intramedullary space of the bone. The richly vascularized intramedullary space allows for direct entry of drugs into the central circulation through emissary veins. The easiest insertion sites are the medial proximal tibia or the distal midline femur. Intraosseous infusion is a rapid and effective technique of achieving therapeutic serum concentrations of almost all important drugs; moreover, a large fluid volume can be rapidly administered in injured or dehydrated patients. The most common complication of this procedure is osteomyelitis.
The sudden and unexpected death of an infant or child in the emergency department constitutes one of the most difficult situations in emergency practice. Chaplin and social services should be made available to aid in support to the family. Careful and compassionate dialogue between the physician and parents, and between the physician and emergency department staff, is essential to minimize chaos in the clinical setting and to reduce confusion and anger among bereaved families and department personnel. Provide the parents with a hospital contact should questions arise after their return home. Debriefing for health-care workers may also be appropriate within 48–72 hours to alleviate stress that may impair work performance or cause psychological disability.
1This chapter is a revision of the chapter by Eric Yazel, MD, & Sandra Herr, MD from the 6th edition.
Cardiovascular Emergencies
Evaluation of cardiopulmonary function in children, especially in infants and younger children, requires special techniques. Vital signs are generally insensitive and nonspecific. Blood pressure poorly reflects volume status. In children, hypovolemia triggers compensatory tachycardia and intense peripheral vasoconstriction, which effectively maintains blood pressure until volume loss exceeds about 50% of intravascular volume.
Tachycardia, while sensitive to cardiopulmonary duress, is nonspecific. Normal heart rate also varies with age, and tachycardia is a common response to many types of stress (eg, fever, anxiety, hypoxia, hypovolemia). In children, assessment of volume status should focus primarily on skin signs (temperature, color, capillary refill, turgor) in combination with heart rate. Rate of urine output may be the next best measure of core perfusion. Adequate core blood flow results in 1–2 mL/kg/h of urine production. Therefore, in the unstable child with suspected perfusion abnormalities, a urinary bladder catheter is imperative to monitor output. Also, close monitoring of mental status and interaction with the surrounding environment is important indicators of adequate cardiopulmonary perfusion.
Cardiac rhythm disturbances in children are unusual. The most common disturbance is bradycardia, usually secondary to hypoxia. Properly applied pulse oximetry, at the triage desk or part of an initial clinical assessment, is an easy and useful method for rapid evaluation of oxygen saturation in patients with slow or rapid heart rates. When a primary tachycardia occurs, it is usually supraventricular in origin. In the distressed child, ECG monitoring will assist in evaluating cardiovascular status and in judging response to therapy.
- Commonly occurs after severe or prolonged episodes of diarrhea and vomiting
- Significant signs include acute weight loss, listlessness, sunken eyes, dry mucous membranes, poor capillary refill, and tachycardia
Acute dehydration is a common pediatric emergency. Diarrhea and vomiting are the most frequent causes. Other common causes are burn wounds, open wounds, fever or hyperthermia, sweating, inadequate fluid intake, polyuria, and poisoning.
The smaller the child, the greater the risk for developing dehydration secondary to the high water body requirement resulting from their surface area/volume ratios. Clinical evaluation of the dehydrated child requires assessment of hydration status. Comparison of presenting weight with recent weights may be useful. Management is dictated by degree of acuity (mild, 3–5% weight loss; moderate, 10%; severe, 15%). Formulate initial treatment on the basis of clinical evaluation of degree of dehydration. Only three clinical signs have been found to be specific for diagnosis of 5% dehydration: prolonged capillary refill time, abnormal skin turgor, and abnormal respiratory pattern. Laboratory assessment of type of dehydration assists the physician in later strategies for specific electrolyte replacement. Serum sodium concentration is the most important laboratory parameter. Serum sodium concentration does not indicate degree of hydration but does provide a useful measure for titrating sodium repletion (ie hyponatremic, isotonatremic, or hypernatremic dehydration).
After rapid assessment of degree of dehydration, management must match severity of illness.
For severely dehydrated patients, provide supplemental oxygen, attach pulse oximeter and cardiac monitor, and establish IV or intraosseous access with one or two secure catheters.
For a severely dehydrated infant or young child, rapidly infuse a balanced isotonic solution (eg, normal saline or lactated Ringer’s). Infants and children have limited glycogen stores and are prone to hypoglycemia when stressed; rapid blood glucose analysis (eg, fingerstick blood sugar) should be performed, and glucose should be replaced if less than 60 mg/dL. Administer 5–10 mL/kg 10% dextrose in water for infants and young children and 2–4 mL/kg 25% dextrose in water for older children.
Administer an isotonic fluid bolus of 20 mL/kg, and then repeat boluses of 20 mL/kg until physical signs (heart rate, skin temperature, and capillary refill) indicate improved perfusion. After 60 mL/kg of isotonic fluid have been administered, if vital signs have not normalized, consider administration of albumin. Packed red blood cells, 10–20 mL/kg, should be considered in cases of blood loss from trauma.
After stabilizing the patient, slow IV infusion to a maintenance rate (Table 50–5) and devise a therapeutic plan. Insert a urinary bladder catheter if the child has uncertain volume replacement requirements. Send blood for complete blood count (CBC); electrolytes; and glucose, blood urea nitrogen (BUN), and creatinine measurements. Obtain a urinalysis. Blood gas determination is indicated for the child who remains unstable after 60 mL/kg of volume administration.
| Weight | Water Requirementa | Sodium Requirement | Potassium Requirementb |
|---|---|---|---|
| 1–10 kg | 100 mL/kg | ||
| 11–20 kg | 50 mL/kg + 1000 mL | 3 mEq/kg | 2 mEq/kg |
| >20 kg | 20 mL/kg + 1500 mL |
When laboratory data are available, titrate sodium and water repletion accordingly. For hyponatremic and isonatremic dehydration, replace the calculated volume deficit over 24 hours, giving 50% of the deficit in the first 8 hours and the remaining 50% over the following 16 hours. Ongoing losses and maintenance requirements must also be included. Control fever, because insensible water losses are significantly increased by temperature elevation. Add small amounts of potassium to the ongoing infusion, once urination is observed, and replace calculated potassium deficits over 48 hours. The minimum daily maintenance requirements for water, sodium, and potassium are noted in Table 50–5. For hypernatremic dehydration, divide fluid and electrolyte replacement evenly over 48 hours to avoid rapid osmolal shifts and CNS complications.
Use oral rehydration therapy (ORT) in most dehydrated patients. Children can usually take fluids by mouth. Vomiting does not contraindicate the use of ORT. Unless shock, altered mental status, or severe weakness is present, ORT may be used as part of early emergency department and inpatient management for most dehydrated patients. Other patients not requiring hospitalization can be easily rehydrated using this technique. ORT in the ED has been underutilized in favor of IV fluid therapy. Recently oral ondansetron (dose 0.15 mg/kg/dose) has been shown to reduce vomiting and facilitate successful ORT. The composition of ORT as set by the World Health Organization includes 90 mEq/L of sodium, 20 mEq/L potassium, 30 mEq/L of citrate, and 1–2% glucose concentration. Commercial preparations that provide approximately these constituents include Pedialyte®, Lytren®, and Infalyte®. Other commonly used clear liquids, such as colas, have too few electrolytes (Na, K, Cl), and their high sugar content may contribute to worsening of osmotic diarrhea. If the child can be discharged, prescribe home fluid replacement that is appropriate for the age of the child, the calculated deficit, and ongoing losses.
- Altered mental status
- Tachypnea, tachycardia
- Hypotension is a late sign in children
Shock is inadequate oxygen delivery to tissues (See Chapter 11). Most causes of shock in children (eg, gastrointestinal fluid losses, burns, blood loss from acute injury) involve decreased stroke volume usually from hypovolemia (hypovolemic shock). Septic shock, a form of distributive shock, occurs usually in the patient under 2 years of age and must always be considered in the sick-appearing, febrile child. Anaphylactic shock, another form of distributive shock, may develop after bee stings or after in-hospital use of parenteral drugs or contrast agents. Cardiogenic shock is extremely rare in children but may complicate congenital heart disease or toxicologic emergencies. Neurogenic shock occurs in trauma, presenting with hypotension and bradycardia (Table 50–6).
| Hypoglycemic | ||
| A. | Hemorrhagic |
|
| B. | Nonhemorrhagic |
|
| Distributive | ||
| A. | Septic | See algorithm |
| B. | Anaphylactic |
|
| C. | Neurogenic | 20 mL/kg NS/LR as needed vasopressors |
| Cardiogenic | ||
| A. | Secondary to arrhythmia | Treat/manage the arrythymia |
| B. | Cardiomypoathy/myocarditis/congetive heart failure |
|
| Obstructive shock | ||
|
|
|
| D. | Thrombolytics |
|
Shock is not hypotension. Successful management includes early recognition of the compensated, normotensive phase of shock. During the compensated phase of hypovolemic shock, vital signs in the supine patient are usually normal, except for mild tachycardia. Skin signs of hypoperfusion are usually evident, and laboratory testing may disclose metabolic acidosis. Intervention is usually successful during this phase. When the hypotensive, de-compensated phase develops in the absence of recognition and effective treatment, irreversible shock and death may result.
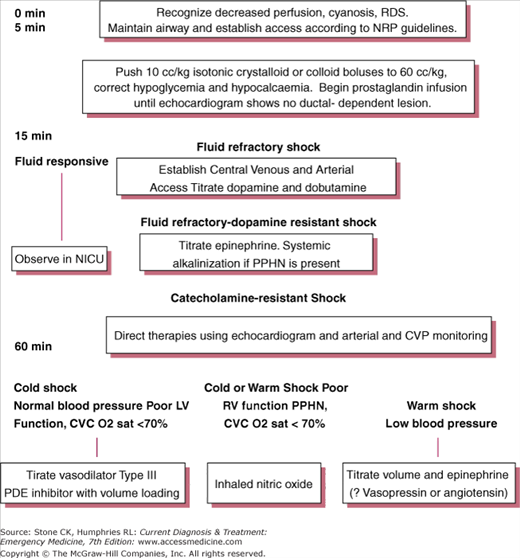
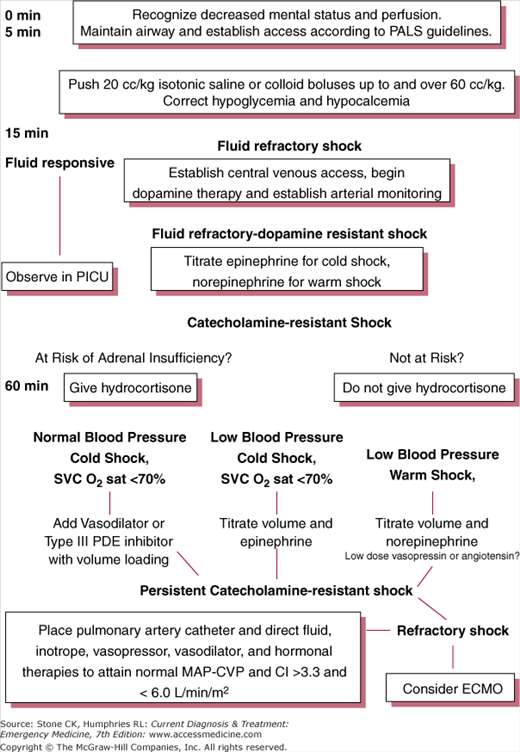
Rapid clinical assessment should disclose a shock category so that focused treatment can be immediately instituted. Failure to act expeditiously and aggressively is a common error and may significantly increase mortality risk. Figure 50–1 is an algorithm for the treatment of uncompensated shock in neonates and Figure 50–2 is an algorithm for treatment of infants and children with uncompensated shock.
Figure 50–1.
Recommendations for stepwise management of hemodynamic support in neonates with goals of normal perfusion and perfusion pressure. PDE, phosphodiesterase; PPHN, persistent pulmonary hypertension, CVCO2, central vena cava oxygen saturation. In refractory shock: rule out and correct pericardial effusion, pneumonthorax. Use hydrocortisone for absolute adrenal insufficiency and consider ECMO. (From Carcillo JA, Fields AI et al: Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med 2002;30 (6)1372.)
Figure 50–2.
Recommendations for stepwise management of hemodynamic support in infants and children with goals of normal perfusion and perfusion pressure (mean arterial pressure–central venous pressure [MAP–CVP]). Proceed to next step if shock persists. PALS, pediatric advanced life support; PICU, pediatric intensive care unit; SVC O2, superior vena cava oxygen; PDE, phosphodiesterase; CI, cardiac index; ECMO, extracorporeal membrane oxygenation. (From Carillo JA, Fields AI: American College of Critical Care Medicine Task Force Committee Members: clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med 2002;30:1370.)
Consider immediate endotracheal intubation. In the ill-appearing child with signs of shock and sepsis or the frankly hypotensive child, intubation should be accomplished either immediately or after the patient fails to respond to first-line resuscitation with oxygen and fluids. After intubation, insert a nasogastric tube.
Apply supplemental oxygen, attach pulse oximeter and cardiac monitor, establish two secure IV catheters, check fingerstick blood glucose, and insert urinary bladder catheter.
Initiate volume resuscitation. Start with 20 cc/kg of isotonic saline administered as rapidly as access will allow. The bolus may be repeated up to two times if no clinical response. If there remains no response after 60 mL/kg, consider colloid or packed red blood cell transfusion or administration of an inotropic agent. When inotropic agents are used, the intravascular volume must be adequate. Inotropic infusions used are dependent on etiology of shock. They can then be titrated at bedside, often using multiple infusions (dopamine, epinephrine, dobutamine), until perfusion is restored. Start with epinephrine at 0.1–1.0 μg/kg/min or dopamine 10–20 μg/kg/min, and then add a second inotropic agent if cardiovascular response does not occur. If physical examination is equivocal for hydration status, a chest X-ray may help: dehydration or overhydration is reflected in the appearance of pulmonary vessels.
Obtain arterial blood gases, CBC, electrolytes, platelets, coagulation studies, blood, urine, and spinal fluid cultures (if infection is suspected), and urinalysis. A urine drug screen may also be considered. A chest X-ray is also necessary in most cases. Administer broad spectrum antibiotics if infection suspected.
- Sweating during feeding or crying; failure to thrive
- Tachypnea, tachycardia
- Hepatomegaly
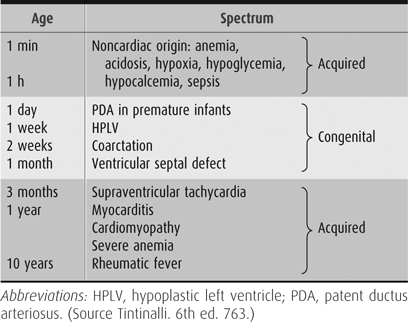
Congestive heart failure (CHF) is unusual in childhood. When it does present, it is usually as a manifestation of congenital heart disease and is seen in the first year of life. Table 50–7 lists the structural conditions causing CHF at different times during infancy. The classic triad of symptoms for pediatric CHF is tachypnea, tachycardia, and hepatomegaly. There may also be a history of poor feeding, sweating or color change with feeding, and poor weight gain. Lower extremity edema and jugular venous distention are less likely in the pediatric population.
Cyanosis in neonates is usually due to either pulmonary or cardiac disease. A CXR, ECG, and hyperoxia test should be obtained in all neonates with unexplained cyanosis. The hyperoxia test is performed by obtaining an initial ABG from the right radial artery on room air. A second ABG is obtained after 10 minutes of breathing 100% FiO2. In general, the pao2 will rise on 100% FiO2 to greater than 80 mmHg in neonates with pulmonary disease. In contrast, it will remain unchanged or only slightly increase in those with cyanotic heart disease (Table 50–8).
| Cyanotic Lesions |
|---|
|
When CHF has progressed to frank pulmonary edema, the treatment is as follows.
Apply supplemental oxygen as necessary including endotracheal intubation in the severely distressed, hypotensive, or hypoxic patient (pulse oximetry < 85% on 100% oxygen). Apply a pulse oximeter and cardiac monitor. Establish secure IV access. Insert urinary bladder catheter and check fingerstick blood sugar.
Pharmacologic treatment can be critically important for patients with left heart obstructive lesions such as hypoplastic left heart syndrome, severe coarctation of the aorta, interrupted aortic arch, and critical valvular aortic stenosis. The newborn is extremely dependent on a patent ductus arteriosus to supply systemic flow. Initial management may require administration of prostaglandin E1 (.05–0.1 μg/kg/min) if a ductal-dependent cardiac lesion is suspected. Apnea is the main side effect of prostaglandin E1; therefore consider intubation prior to transport of a patient during an infusion. In other cases, first-line pharmacologic management is furosemide, 1 mg/kg IV.
Obtain chest X-ray, ECG, CBC, and serum electrolytes, with additional studies if indicated. Consider digoxin in refractory cases. Occasionally, patients with severe pulmonary edema unresponsive to initial therapy require dopamine, dobutamine, or both.
Dysrhythmias are relatively rare in the pediatric population, with the most common being sinus tachycardia, supraventricular tachycardia, and bradycardia. Atrial flutter may be present in patients having undergone cardiac shunting surgeries (ie Fontan procedure) These can present a diagnostic challenge to the emergency physician as vague and nonspecific symptoms may be the rule. Evaluation of dysrhythmias includes a rapid cardiopulmonary assessment and ECG interpretation using a systematic approach and comparison with age-specific norms.
See Table 50–9.
| Rhythm | Rate/min | QRS | Initial Treatment | Drug Therapy |
|---|---|---|---|---|
| Narrow complex tachycardia’s | ||||
| 1. Sinus tachycardia | 100–250 | <0.10 | Oxygen, fluids, warmth, calm manner | Treatment of primary condition |
| 2. Atrail flutter | 300–500 | <0.10 |
|
|
| 3. Atrail fibrillation | Ventricle response 60–90 irregularly Irregular | <0.10 |
|
|
| 4. Supraventricular Wolf-Parkinson-White | 120–300 | <0.10 |
| Adenosine 0.1 mg/k rapid IV push max 6 mg single first dose if unaffective repeat at 0.2 mg/kg (max 12 mg) |
| Wide complex tachycardias | ||||
| 1. Ventricular tachycardic | 150–260 | >0.10 |
|
|
| 2. Wolff- Parkinson White | 150–300 | >0.10 | As for ventricular tachycardia | As for ventricular tachycardia |
| Ventricular fibrillation | 300–500 | Variable |
|
|
| Torsades de points | 300–500 | Variable | Magnesium sulfate: 25–50 mg/kg (max 2 grams) | |
| Bradycardia | ||||
| 1. Sinus | Age-related | <0.10 | Oxygen, airway management stimulation |
|
| 2. AV-V block | Age-related | Variable | Oxygen if unstable transcutaneous pacing | as for sinus brady cardia |
Apply supplemental oxygen; attach pulse oximeter and cardiac monitor. Establish a secure IV line. Obtain an ECG.
Unstable patients with tachydysrhythmias require immediate electrical cardioversion or defibrillation. Unsynchronized mode is recommended for ventricular fibrillation and pulseless ventricular tachycardia, synchronized for the remaining rhythms. Exact energy levels are dictated by the nature of the dysrhythmia (see Table 50–9).
Ensure that paddles are held firmly against chest wall and a good conductive agent is employed. If standard 4.5-cm pediatric paddles are unavailable for sternoapical placement, use adult paddles in an anteroposterior configuration.
Pretreat conscious patients requiring cardioversion with light sedation, and be prepared to perform endotracheal intubation and full cardiopulmonary resuscitation if necessary.
Respiratory Distress
In children, normal ventilation and oxygenation occurs with minimal visible effort. Evaluation of respiratory function includes assessment of rate, work of breathing, skin and mucous membranes color, and mental status. Respiratory rate alone is an insensitive means of evaluating for respiratory distress. Rates vary greatly with age, anxiety, excitement, or fever, and interobserver reproducibility is often poor. Tachypnea may be an early manifestation of respiratory distress, or it may result from respiratory compensation for metabolic acidosis caused by shock, diabetic ketoacidosis, inborn errors of metabolism, salicylism, or chronic renal insufficiency. A slow respiratory rate may indicate impending respiratory failure.
Observation alone will usually disclose distress or increased work of breathing. Increased work of breathing is also evidenced by nasal flaring and by suprasternal, intercostal, and subcostal retractions. Retractions become more pronounced cephalad to caudad with increasing hypoxia. Grunting is produced by premature glottic closure and usually represents alveolar collapse and loss of lung volume, which develops in patients with pulmonary edema, pneumonia, or atelectasis. Auscultation will provide further differentiation of disease possibilities. Wheezing, rales, or decreased breath sounds may be present. Cyanosis, when present, represents severe distress and is best seen on mucous membranes of the mouth and nail beds. Peripheral cyanosis is more likely due to circulatory failure than a primary pulmonary source. Finally, mental status changes may be a clue to gas exchange abnormalities. Hypoxic patients are restless and agitated; hypercapnic patients are drowsy or even comatose.
Rapid evaluation of respiratory function is imperative in all distressed pediatric patients. Respiratory failure and respiratory arrest due to a wide spectrum of causes (eg, head trauma, coma, poisoning, pneumonia, asthma, foreign body aspiration) are the most common causes of cardiac arrest in childhood. Timely, aggressive intervention in the early stages as well as meticulous respiratory monitoring by means of pulse oximetry and continuous observation will avert preventable adverse patient outcomes. Children with respiratory distress should not be sent for imaging studies without qualified personnel in attendance. Early hospital admission is usually warranted for such patients.
Pulse oximetry should be used liberally in the emergency department setting in order to disclose undetected oxygen desaturation states. Pulse oximetry is noninvasive, simple, and reasonably accurate. Readings may be difficult to obtain in patients with poor perfusion or cold sites of placement. In selected patients, especially those with significant tachypnea or work of breathing, pulse oximetry may underestimate degree of distress, and it provides no indication as to the adequacy of ventilation. In such patients, it may be necessary to obtain arterial blood gas levels to help measure the severity and nature of the ventilation or oxygenation disturbance.
Apnea is defined as an unexplained episode of cessation of breathing for 20 seconds or longer, or a shorter respiratory pause associated with bradycardia, cyanosis, pallor, and/or marked hypotonia. Ordinary sleep will sometimes cause breathing irregularities easily confused with apnea. There are two classifications of apnea: central and obstructive. Central apnea is characterized by an absence of respiratory effort secondary to diminished muscular activation. It occurs in newborn infants, most commonly in preterm infants. Infection, metabolic abnormalities, anemia, hypoxia, or CNS injury may be associated with newborn apnea. Obstructive apnea occurs in later infancy and childhood and is related to obstructive upper airway conditions. This results in cessation of airflow despite respiratory effort, as can be seen with chest and abdominal movement. Apnea may be accompanied by color change, marked change in muscle tone (usually limpness), choking or gagging which is frightening to the observer. This is the definition for apparent life-threatening event (ALTE).
Apnea in infants may be symptomatic of life-threatening illness. Such patients ordinarily require hospital admission for observation and full workup for infections and for CNS, metabolic, and feeding problems. Initial management in the emergency department is discussed here.
Place child on supplemental oxygen, and apply pulse oximeter and cardiac monitor or apnea monitor.
If evidence of dehydration is present, establish IV access and replete with an isotonic fluid bolus.
Obtain blood for CBC with differential, electrolytes, BUN, creatinine, ionized calcium and magnesium, and cultures. Obtain urinalysis and urine cultures as well as toxicology studies. CT of the head should be strongly considered for evaluation of any infant with abnormal mental status, bulging fontanelle, or focal neurological examination. Spinal fluid analysis should also be considered in any lethargic- or toxic-appearing infant.
Admit for observation and further evaluation on an apnea monitor.
Obstructive apnea may be serious. Focus evaluation on obstructive upper pharyngeal lesions such as tonsillitis and pharyngitis or laryngomalacia. Chest X-ray and lateral neck films are often necessary. Emergency department evaluation may be insufficient to exclude a serious diagnosis, such as airway masses, and hospital admission may be indicated.
The evaluation for ALTE is primarily dependent upon the history and physical exam. Currently, in-hospital observation and monitoring remain an accepted treatment, especially in infants less than 48 weeks postconceptional age.
- Inspiratory stridor
- Suspect foreign body aspirations if symptoms develop rapidly without associated signs of infection
- Anteroposterior and lateral neck X-rays are helpful to differentiate croup from epiglottitis and foreign body
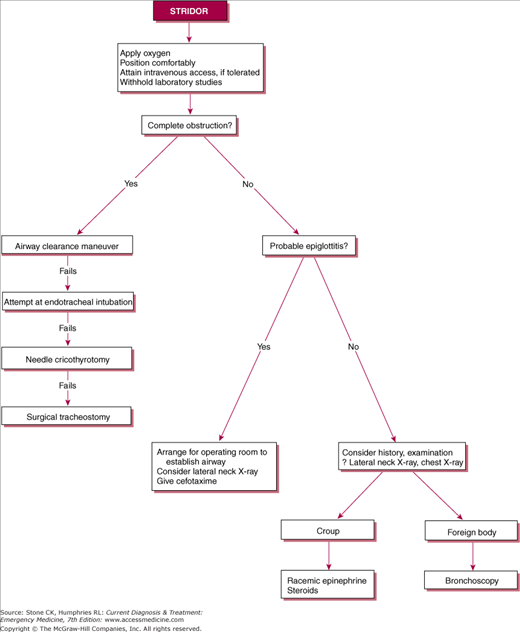
Upper airway obstruction is usually readily apparent. Inspiratory stridor is the hallmark. The child is dyspneic and shows signs of respiratory distress, including tachypnea, nasal flaring, and supraclavicular, intercostal, and subcostal retractions. Ventilation and oxygenation abnormalities are sometimes present. If obstruction is severe, hypercapnia will be present, usually along with depressed mental status, cyanosis, and decreased air movement. Arterial blood gases will demonstrate carbon dioxide retention and often hypoxemia. Pulse oximetry will be abnormal in most advanced cases but normal in typical cases (see Figure 50–3).
In children, the common causes of stridor and upper airway obstruction are croup, epiglottitis, and foreign body aspiration (see Table 50–10). Other less common conditions producing stridor are bacterial tracheitis (usually Staphylococcus aureus, Streptococcus pneumoniae, or Haemophilus influenzae), retropharyngeal or peritonsillar abscess, trauma, caustic ingestions, neoplasm, or angioneurotic edema.
| Croup | Epiglottitis | Foreign Body | |
|---|---|---|---|
| Age | 6 months to 3 years | 2–5 years | Under 3 years |
| Cause | Parainfluenza | Strep. pyogenes, Strep. pneumoniae, Staph. aureus, H. influenzae (rare) | Foreign body |
| Season | Fall or winter | Any | Any |
| Time of day | Night or morning | Any | Daytime |
| Illness features | |||
| Onset | Slow | Abrupt | Abrupt |
| Upper respiratory infection | Yes | No | No |
| Fever | Generally low grade | High | None |
| Toxic | Mild | Yes | No |
| Pharyngitis | Possible | Yes | No |
| Drooling | No | Yes | No |
| Stridor | Inspiratory + expiratory | Inspiratory | Inspiratory + expiratory |
| Position | Variable | Sitting | Variable |
| Hoarseness | Yes | Rare | No |
| Ancillary tests | |||
| White blood count | Normal | High | Normal |
| Chest X-ray | Steeple sign | Normal | Hyperinflation |
| Lateral neck | Normal | Swollen epiglottis, “thumbprint sign” | May show radiopaque body |
Clear the airway using procedures recommended in Table 50–11 for the patient with complete airway obstruction. Avoid airway clearance maneuvers in the patient with partial airway obstruction as this may result in further progression to a complete obstruction. Allow the child to adopt a position of comfort, usually on a parent’s lap. Apply supplemental oxygen, and attach pulse oximeter and cardiac monitor. Avoid procedures or interventions that cause agitation or worsening symptoms.
| Status | Infant (up to age 1 year) | Child (1–8 years) |
|---|---|---|
| Conscious |
|
|
| Unconscious |
|
|
Anaphylaxis is a life-threatening manifestation of immediate hypersensitivity. It is an IgE-mediated reaction that occurs after re-exposure to an antigen. Symptoms develop within 30 minutes of exposure to the inciting agent. Manifestation may be mild, demonstrating urticaria or severe involving upper airway obstruction resulting from edema of the larynx, epiglottis, and surrounding structures. Hypotension, secondary to profound vasodilatation and seizures may occur.
Management consists of maintenance of airway and oxygenation. Attach a pulse oximeter and cardiac monitor. Initial pharmacologic management consists of administration of epinephrine (1:1000), 0.01 mL/kg (max 0.5 mL) IM. For bronchospasm (wheezing), administer albuterol by metered-dose inhaler (MDI) or nebulizer. For stridor, racemic epinephrine 2.25% solution dosed 0.05 mL/kg (max 0.5 mL) diluted with normal saline to volume of 3 mL for nebulization. For hypotension, administer 20 mL/kg bolus isotonic fluids with the addition of inotropic agents if needed. Other therapies include: H-1 receptor-blocking antihistamines, such as diphenhydramine (1 mg/kg) IV/PO/IM; corticosteroids (1–2 mg/kg methylprednisolone IV, max 125 mg, or oral prednisone 1–2 mg/kg (max 80); H-2 receptor-blocking antihistamines such as cimetidine (5 mg/kg, max 300 mg) or ranitidine (1–2 mg/kg, max 50 mg) work synergistically with H-1 blocking antihistamines. Children with airway involvement should be monitored for 24 hours. Discharge instructions must involve instruction and dispension of epinephrine auto-injector use.
Epiglottitis has become much less common since the introduction of the H. influenzae type B vaccine. The epidemiology has now changed to more commonly involve older children and adolescents, with Staphylococcus and Streptococcus being the most common etiologic agents. The patient often presents with dysphonia and dysphagia and sits in the sniffing position. The findings on oropharyngeal examination are typically unimpressive. However, the patient may rapidly progress to stridor and complete airway obstruction. In such cases, early airway management is essential, preferably in the operating room. In the meantime, minimize all invasive procedures in order to avert patient agitation and potential precipitous airway obstruction, and ensure that equipment for airway management is readily available. The patient should not be left unattended at any point.
Once the airway is secured, obtain blood and throat cultures and begin antibiotic therapy with second or third generation cephalosporins plus coverage for the treatment of possible methicillin-resistant Staphylococcus with vancomycin.
In a patient with a lower likelihood of epiglottitis, a soft tissue lateral film of the neck may be useful to help demonstrate the swollen epiglottis (Figure 50–4).
Bacterial tracheitis is also known as psuedomembranous croup, is characterized by prodromal viral upper respiratory symptoms with low grade fever, cough, and stridor similar to croup. Unlike epiglottis, a cough may be present. Typically, the child is without drooling and may be comfortable lying flat. Routine laboratory data are not indicated. The diagnosis is made endoscopically by visualizing normal supraglottic structures with prominent subglottic edema, ulcerations, and copious purulent secretion. Patients with severe distress are best managed in the operating suite for endoscopic diagnosis and intubation. If emergency department intubation is required, an endotracheal tube smaller that the calculated size for the patient may be necessary. Antibiotic coverage should be initiated with a third generation cephalosporin plus vancomycin.
Croup is infection and inflammation of the subglottic airway causing upper airway obstruction. It is characterized by barking cough, hoarseness, and inspiratory stridor. The physician must note that symptoms are typically more severe at night; thus the presentation may not be as impressive in daytime hours. Therapy includes the following:
Attach pulse oximeter and cardiac monitor. Keep the child in a position of comfort, usually on the parent’s lap. Cool humidified mist, although frequently administered, has not been shown to be effective in improving clinical symptoms in children presenting to the ED.
Give glucocorticoids to any child who presents with croup symptoms and demonstrates increased work of breathing. Give PO/IM/IV dexamethasone, 0.6 mg/kg (max 10 mg) once. In more severe cases, nebulized epinephrine should be considered. This can provide immediate improvement though reduction in edema and secretions. Dosage for nebulization is 0.5 mL/kg (maximum of 5 mL) of 1:1000 preparation of epinephrine, or racemic epinephrine 2.25% is dosed at 0.05 mL/kg (maximum 0.5 mL) diluted with normal saline to a total volume of 3 mL. In severe croup, consider administration of heliox (a mixture of helium and oxygen). In patients unresponsive to nebulized epinephrine, steroids or heliox, endotracheal intubation and ventilation may be necessary. Using a tube with a diameter smaller than recommended for patient age and size should be used.
For the minimally distressed child, treatment with steroids may be adequate. For patients who receive nebulized epinephrine, caution must be taken because the clinical effects of epinephrine wane after 2 hours. All patients should be monitored during this time period for worsening or return of symptoms. Those who remain without stridor or hypoxia, appear comfortable, and tolerating oral fluids may be discharged with a reliable parent. All others should be hospitalized for observation and further treatment.
Foreign body aspiration can have a constellation of physical findings depending on the degree of occlusion of the airway. The presentations can range from a complete obstruction managed by the Heimlich maneuver to a protracted course of wheezing not responsive to bronchodilators. The history can be highly suggestive, with a brief asymptomatic interval followed by severe dyspnea, coughing, and gagging, after the child has handled a small object. In 20% of cases, the object is in the upper airway; in 80% it is in the main-stem or lobar bronchus. Stridor is present if the object is lodged high, at the level of the larynx; wheezing and decreased breath sounds occur if it is lodged below the larynx. Mild tachypnea may be the only clinical sign in some instances. Useful X-ray views include the lateral neck, chest, and bilateral lateral decubitus end-expiratory chest, which may show hyper-inflation in the affected lung.
If obstruction is complete and airway clearance maneuvers (see Table 50–11) fail, perform laryngoscopy immediately, and attempt to remove the foreign body with Magill forceps under direct visualization. After removal of a foreign body, insert a properly sized endotracheal tube to prevent later inflammatory obstruction.
In most patients, obstruction is partial. Apply supplemental oxygen, and attach pulse oximeter and cardiac monitor. Allow the patient to assume a position of comfort, usually on parent’s lap. Obtain airway and chest X-rays. Maintain constant observation of the patient by nurse or physician. Arrange for rigid bronchoscopy, under general anesthesia, to remove the foreign object.
Lower airway disorders are a disparate group of conditions with varying clinical presentations that may affect oxygenation and ventilation. Lower airway disease includes both obstructive conditions and parenchymal or alveolar disease. The clinical hallmarks are dyspnea and tachypnea, often with cough. Wheezing denotes an obstructive process.
In children, the most common causes of lower airway obstruction are bronchiolitis, asthma, and foreign body obstruction. In infants, congenital abnormalities of the airway (tracheal web, cysts, vascular rings, lobar emphysema) must also be considered. Pneumonia is the most frequent pediatric alveolar disorder, although pulmonary edema, pneumonitis, inhalation injury, and cystic fibrosis must also be excluded.
Bronchiolitis is a clinical syndrome characterized by the acute onset of respiratory symptoms in a child younger than 2 years of age. The typical course consists of an upper respiratory tract infection progressing within 4–6 days to involve the lower respiratory tract with the onset of cough and wheezing. Respiratory syncytial virus (RSV) is the most common underlying viral infection. More than half of the affected children are between 2 and 7 months of age. Clinical signs of respiratory distress are variable. The white blood cell (WBC) count may be slightly elevated or normal. Hyperinflation, patchy infiltrates, and atelectasis may all be seen on chest X-ray.
Supportive care is the mainstay of therapy. Ensure hydration, oxygenation, and clearing of secretions with nasal suction. Intubation may be required for respiratory failure. Attach pulse oximeter, apply supplemental oxygen for saturations < 92%.
There is conflicting evidence as to the efficacy of bronchodilator therapy in bronchiolitis.
If wheezing is present, a trial of nebulized epinephrine or albuterol can be considered. Bronchodilators should be continued only if there is a documented clinical response. Deep nasal suctioning is helpful. Nebulized 3% hypertonic saline seems to provide a beneficial effect as an adjunct to aid in clearance of thickened secretions. Recent reviews recommend that steroid therapy not be given. Heliox (a mixture of helium and oxygen), high flow nasal oxygen, or nasal continuous positive airway pressure (CPAP) may be trialed prior to intubation for severe or refractory disease.
Obtain a chest X-ray and consider a nasopharyngeal swab for RSV viral testing.
Infants younger than 2 months of age, former premature infants, any history of apnea or cyanosis, and those with underlying chronic medical conditions or congenital abnormalities should be strongly considered for admission, as well as any patient with persistent tachypnea, hypoxia, or toxic appearance.
Asthma is one of the most common diseases of childhood and accounts for over 15% of all emergency department visits. It is characterized by bronchial hyperreactivity, airway inflammation, and reversible airway obstruction. The overall prevalence of asthma is increasing. Despite significant efforts in treatment and management, mortality rates have not improved, especially in urban areas.
Pulmonary function tests are also of great importance in assessing the severity of an exacerbation. Peak flow testing is relatively easy to perform and has been shown to be relatively successful even in young children. The patient’s baseline value is especially useful, if known; otherwise comparison can be made with the patient’s predicted value. Chest X-rays are usually not indicated in afebrile patients with known disease, but may be of assistance when the etiology is unclear. Arterial blood gas is indicated in more severe exacerbations. Close monitoring of pco2 should occur as normalization or elevation can indicate impending respiratory failure.
When a patient presents during and asthma exacerbation, important historical information includes recent steroid use, prior intensive care unit admissions, prior intubations secondary to asthma, preceding triggers, medications and frequency of their use, and baseline peak expiratory flow rates (PEFRs).
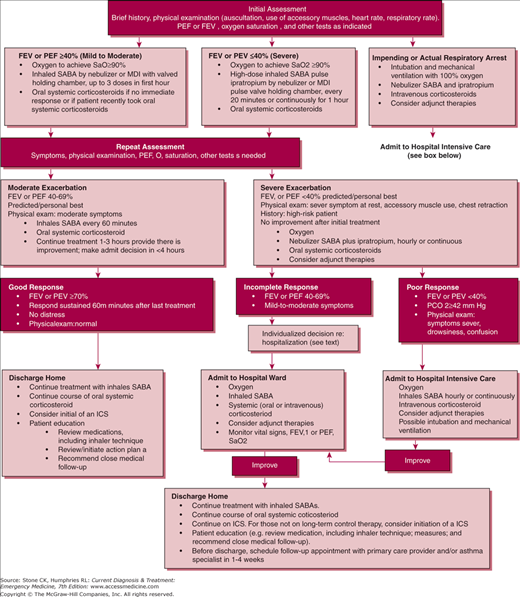
See Figure 50–5.
Figure 50–5.
Management of asthma exacerbation: emergency department and hospital-based care. Key: FEV1, forced expiratory volume in 1 second: ICS, inhaled corticosteroid; MDI, metered-dose inhaler; pco2, partial pressure carbon dioxide; PEF peak expiratory flow; SABA, short-acting β2-agonist; SaO2, oxygen saturation. (Reproduced from National Institutes of Health: National Asthma Education and Prevention Program. Expert Panel 3: guidelines for the diagnosis and management of asthma. August 2007. NIH publication no 07-4051.)
Attach pulse oximeter, provide supplemental oxygen therapy, if required.
These are the first-line agents for the treatment of the acute asthma exacerbation, causing the rapid relaxation of bronchial smooth muscle. Albuterol is typically the agent used (0.15 mg/kg; maximum 5 mg). Both metered dose inhaler and nebulizer have been shown to be equally efficacious. Nebulizer is the method of choice in young children who may have difficulty with proper inhaler use.
Glucocorticoids are indicated for all children with asthma who present in an acute exacerbation. The initial dose of prednisone is 1–2 mg/kg, with a maximum of 60 mg. Oral and IV routes have been shown to be equivalent.
Ipratropium is used as an adjuvant therapy to β-agonist therapy. It has been shown to decrease ED treatment time and improve pulmonary function testing. Dosing is 250 mcg per nebulized treatment for patients’ weights less than 15 kg and 500 mcg for weights greater than 15 kg.
In severe exacerbations where nebulizer or MDI treatments may not be tolerated or rapid decompensation occurs, subcutaneous epinephrine or terbutaline (0.01 mg/kg up to 0.3–0.5 mg) or IV terbutaline (10 μg/kg over 10 minutes followed by infusion of 0.4 μg/kg/min) may be considered.
Several conflicting studies exist but data have been shown that magnesium sulfate has improved pulmonary function and reduce hospitalizations in certain subgroups. Dosage is 25–50 mg/kg (maximum of 2.0 g) over 20 minutes. Close monitoring for hypotension is indicated.
Bi-level positive airway pressure (BiPaP) in treating pediatric status asthmatics is safe and effective with resulting prevention of intubation.
Ketamine intravenous infusions have also been controversial in the management of severe asthma exacerbations. However, infusion at a bolus dose of 0.2 mg/kg followed by an infusion of 0.5 mg/kg was not found beneficial.

Full access? Get Clinical Tree