Pediatric Anesthesia
I. Anatomy and Physiology
Airway. Understanding the anatomic differences between infant and adult upper airways is key to managing infants’ airways safely (Table 42-1) (Lerman J. Pediatric anesthesia. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013:1216–1256).
As a result of these anatomic features, the head in the child is naturally in the “sniffing” or flexed position.
The large tongue:mouth ratio presents difficulty if the mouth is closed during mask ventilation, particularly with the narrowed nares.
The most common airway problem in infants and young children is upper airway obstruction caused by laryngomalacia.
A number of airway anomalies may present problems during anesthesia (Table 42-2).
The cricoid ring represents the only solid cartilaginous structure in the upper airway because it is covered with pseudostratified columnar epithelium.
This epithelium is subject to swelling if irritated, swelling into the lumen and reducing the radius of the airway.
A 50% reduction in the radius of the cricoid ring increases the work of breathing, which cannot be sustained resulting in respiratory failure.
The short trachea in the infant and child facilitates accidental endobronchial intubation (persistent <85% saturation).
Cardiovascular
In the early years, the heart has limited ability to increase stroke volume, rendering cardiac output more dependent on heart rate than in the adult. (Hypotension in the child with a normal or increased heart rate is caused by hypovolemia and should be treated with volume expansion rather than vasopressors [except in children with congenital heart disease].)
Table 42-1 Anatomic Features of the Upper Airway in Infants Compared with Adults
Head
Larger occiput in the infant naturally positions the head in the “sniffing” position
Stabilize the head against lateral rotation
Obligate nose breathers for the first few months
Mouth
Relative larger tongue volume in the mouth in the infant reduces the available space for instrumentation
Edentulous
Neck
Larynx is more cephalad in the neck (C3–C4) in the infant
Epiglottis is omega shaped and longer
Vocal cords slant caudally at their insertion in the arytenoids
Narrowest part of the upper airway is the cricoid ring (a solid, conically shaped, cartilaginous structure); pseudostratified columnar epithelium covers the ring
Trachea is shorter (4–5 cm)
Tracheobronchial tree
Acute angle of the right mainstem bronchus at the carina
Turbulent gas flow until the fifth bronchial division (resistance is related inversely to the radius to the fifth power)
Systemic vascular tone is low in children up to 8 years of age, as evidenced by the lack of a change in blood pressure when caudal or epidural blocks are administered.
Both heart rate and blood pressure increase with increasing age in childhood (Table 42-3).
Table 42-2 Airway Anomalies that may Present Problems During Anesthesia
Pierre Robin syndrome (micrognathia, glossoptosis, airway distress in first 24 hrs): Typically easy intubation by 2 yrs of age
Treacher Collins syndrome (progressively more difficult airway management with increasing age)
Crouzon disease, Apert disease, and Down syndrome (difficult mask ventilation but tracheal intubation is straightforward)
Table 42-3 Normal Range of Resting Heart Rates and Blood Pressure in Children
Age
Heart Rate (beats/min)
Blood Pressure (mm Hg)
0–3 mo
100–150
65–85/45–55
3–6 mo
90–120
70–90/50–65
6–12 mo
80–120
8–100/55–65
1–3 yr
70–110
90–110/60–75
3–6 yr
65–110
95–110/60–75
6–12 yr
60–95
100–120/60–75
>12 yr
55–85
110–135/65–85
Central Nervous System
Oxygen consumption in the brains of children (5.5 mL/100 g/min) is 50% greater than that in adults (3.5 mL/100 g/min). In children 6 months to 3 years of age, the cerebral blood flow is 50% to 70% greater than in adults (50 mL/min/100 g vs. 70–110 mL/min/100 g).
Apoptosis. Most general anesthetics (with the exception of xenon, dexmedetomidine, and opioids) and sedatives, that also act on N-methyl-d-aspartic acid (NMDA) and GABAA receptors, cause apoptosis in newborn rodents and nonhuman primates after relatively prolonged exposure (>12 hours) and when administered in combination.
Brief anesthesia with ketamine (≤3 hours) or isoflurane (<2 hours) fails to induce neurocognitive dysfunction.
Whether the rodent and nonhuman primate evidence of anesthetic-induced neurotoxicity is applicable to humans remains hotly debated. (Because most anesthetics in young children last <3 hours, these data may have limited validity in humans.)
Also, the doses of intravenous (IV) anesthetics and sedatives in rodents and primates are up to 10-fold greater than in humans.
Studies in humans who received anesthesia at a young age suggested that cognitive disability in those who received anesthesia before the age of 3 years may be more prevalent than in those who did not. However, most of those studies were seriously flawed in terms of their design, and a large cohort of identical twins who were discordant for general anesthesia before 3 years of age in one study, when tested for intellectual aptitude 10 years later, were similar.
II. Pharmacology
Developmental Pharmacology
Age may have a substantial effect on the absorption of certain drugs, for example, because gastric juice is closer to neutral pH (pH ∼6) at birth and does not reach adult levels of acidity until about 3 years of age.
The albumin concentration is low in children, and α1-acid glycoprotein concentration is also reduced at birth and increases slowly with increasing age as well as during periods of stress. (Free fraction of medications such as lidocaine is greater in young infants than older children because the concentration of α1-acid glycoprotein in the former is reduced.)
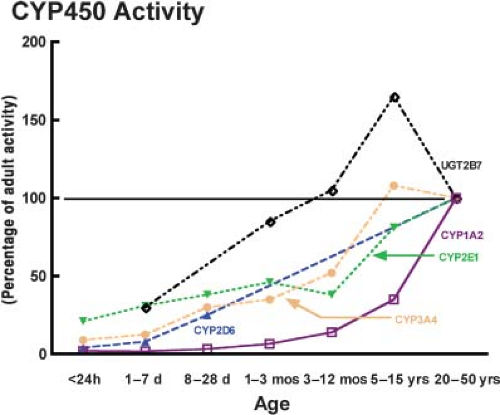
Apart from a few enzyme systems that hold importance in fetal life (CYP450 3A7), the activities of the vast majority of CYP450 enzyme systems (CYP450 3A4, 2E1, and 2D6) increase with age from birth but at divergent rates (Fig. 42-1).
Table 42-4 Factors Increasing the Washin of Inhalatonal Anesthetics in Children Compared with Adults
Alveolar ventilation: FRC ratio (5:1 in infants vs. 1.5:1 in adults)
Greater distribution of cardiac output to the vessel-rich group in infants (vessel-rich group comprises 18% of the body weight in infants compared with 8% in adults)
Reduced tissue solubility in infants
Reduced blood solubility in infants
FRC = functional residual capacity.
The glomerular filtration rate is markedly reduced in neonates but matures throughout childhood, reaching adult rates by 5 to 15 years of age.
Inhalational Anesthetics
The widespread appeal of the current inhalational anesthetics may be attributed to their physicochemical properties, which provide a rapid onset and offset of action, cardiorespiratory homeostasis, and limited metabolism and toxicity (Table 42-4).
Sevoflurane is the induction agent of choice in infants and children. Desflurane offers the most favorable pharmacokinetic and in vivo metabolic characteristics in terms of its minimal blood and tissue solubilities and resistance to metabolism, although its use as an induction agent in children is proscribed because it irritates the upper airway.
Pharmacokinetics
The greater ratio of alveolar ventilation to functional residual capacity (FRC) in infants and children compared with adults speeds the equilibration of inspired to alveolar anesthetic partial pressures. The net effect of a greater ventilation: FRC ratio is a reduction in the time constant, from 0.7 in adults to 0.2 in infants, which explains the speed of equilibration (sudden and rapid responses observed to inhalational anesthetic in infants and children compared with adults).
The greater cardiac output in infants speeds the equilibration of alveolar to inspired anesthetic partial pressures in the vessel-rich group, which takes up most of the anesthetic during the first couple of hours of anesthesia.
The solubility of all inhalational anesthetics is reduced in tissues in infants compared with adults, including in the brain, muscle, and heart.
Pharmacodynamics
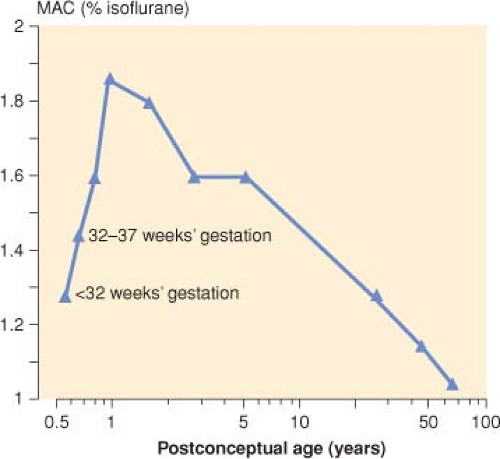
As a fetus matures and reaches birth, the minimum alveolar concentration (MAC) increases, peaking in infants 1 to 6 months of age isoflurane and then decreases steadily thereafter with increasing age (Fig. 42-2). (The reason for the age-dependent differences in MAC is unclear.)
The MAC of desflurane in adult redheads is 20% greater than in nonredheads; the same response would be expected in children of similar genetic predisposition.
III. Respiration
All anesthetics, when administered in the absence of surgical stimulation, depress respiration and minute ventilation in a dose-dependent manner by decreasing tidal volume and increasing respiratory rate.
Airway resistance increases during desflurane anesthesia and decreases during sevoflurane anesthesia. (In children with asthma, the former is best avoided, and the latter is preferred.)
Upper airway responses to inhalational anesthesia (by mask) depend on both the concentration and the particular anesthetic administered. (Whereas sevoflurane does not trigger these reflex responses, isoflurane and desflurane are most irritating to the airway, particularly at >1 MAC concentrations.) The package insert for desflurane cautions against using it for inhalational inductions in children.
IV. Cardiovascular
Inhalational anesthetics depress the heart in a dose-dependent manner.
In the past, anticholinergics were commonly used to prevent bradycardia and arrhythmias in children given halothane; however, this practice is no longer necessary with the newer ether anesthetics that infrequently cause arrhythmias.
Sevoflurane maintains or increases heart rate during induction of anesthesia in most instances likely because of withdrawal of vagal tone. Desflurane and isoflurane tend to increase the heart rate.
Cardiac output in young children is dependent on heart rate.
Peripheral vascular resistance is very low in children as evidenced by the absence of a change in blood pressure when a caudal/epidural block is administered.
V. Central Nervous System
All inhalational anesthetics decrease cerebral vascular resistance and the cerebral metabolic rate for oxygen.
Autoregulation of cerebral blood flow in children of all ages is similar to that in adults, although it occurs at greater blood flow rates. The lower limit of autoregulation in children of all ages appears to be similar (60 mm Hg mean arterial pressure).
Bispectral index readings are imprecise in children < 5 years of age.
VI. Renal
Inhalational anesthetics do not exert substantive effects on the kidneys in children except through their metabolism, with the kidneys being a site of degradation of inhalational anesthetics.
VII. Hepatic
VIII. In Vivo Metabolism
Degradation of inhalational anesthetics in the presence of carbon dioxide absorbents has been the subject of intense research and concern in both adults and children.

Full access? Get Clinical Tree