
PATHOPHYSIOLOGY OF ACUTE ILLNESS AND INJURY
In the setting of an acute surgical illness, the patient’s body responds to stresses resulting from tissues in distress and often from microbial invasion. This results in profound changes in the function of most organs and systems. Most of these changes are adaptive. The range and extent of the responses depend on not only the type of insult but also host factors (see Table 3.1). When excessive, the responses designed to allow the host to adapt can become dysregulated or excessive and hence maladaptive. Timely intervention can limit the untoward consequences. However, an appreciation of both the adaptive and maladaptive response can assist with care decisions that can impact patient outcomes.
TABLE 3.1
PATIENT FACTORS ASSOCIATED WITH INCREASED MORTALITY
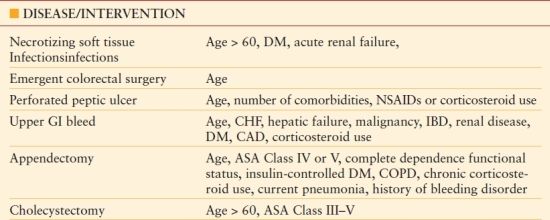
DM, diabetes mellitus; NSAIDs, nonsteroidal anti-inflammatory drugs; GI, gastrointestinal; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; IBD, inflammatory bowel disease; CHF, congestive heart failure; ASA, American Society of Anesthesiologists.
Systemic responses are secondary to a combination of factors including neurohormonal responses, release of bioactive molecules from damaged or injured tissues, or infectious organisms or elaborated products. The extent to which tissue damage and invasive infection contribute to the host response can vary considerably by the type of insult. For example, in cholangitis, minimal tissue damage occurs but bacteremia can be substantial. Likewise with gastrointestinal ulceration, a small area of tissue necrosis can result in diffuse peritonitis and sepsis if there is free perforation.
As local disease processes become more extensive, a systemic response ensues. Patients may exhibit tachycardia, tachypnea or carbon dioxide retention, or temperature elevation above 38°C or below 36°C. Complete blood counts may reveal leukocytosis of 12K white blood cells/mm3 (WBC) or higher, depression below 4K, or bandemia. Having at least two of the aforementioned physiologic changes or laboratory values defines a patient as having systemic inflammatory response syndrome (SIRS) and, in the setting of infection, defines a patient as having sepsis. However, in the clinical setting, a patient is usually referred to as being “septic” when he or she has sepsis and some form of organ dysfunction, such as altered mental status or oliguria. Patients have progressed to septic shock when they develop hypotension resistant to fluid boluses.
Along the spectrum of localized inflammation to septic shock, the surgeon must determine how well a patient is compensating and how much physiologic reserve the patient has remaining. A systematic approach to evaluating patients in acute care surgery allows for an appropriate global evaluation of the patient. Several scoring systems have been developed to estimate the physiologic status of the patient. Among the most predictive is the Acute Physiology and Chronic Health Evaluation II (APACHE II) classification system (see Fig. 3.1). Although not often calculated acutely, this classification system assesses parameters of organ and system function that should be part of the evaluation of acutely ill surgical patients.
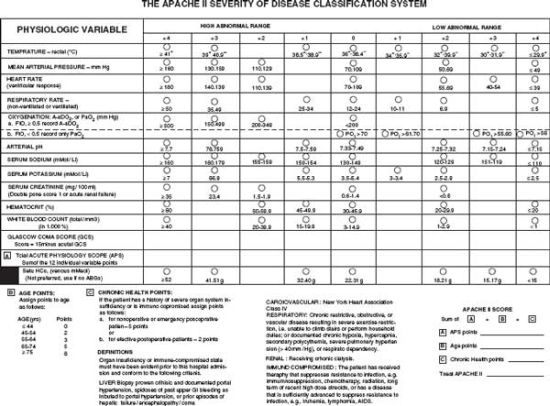
FIGURE 3.1. The APACHE II severity of disease classification system. (From Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829.)
CARDIOVASCULAR
Patients with coronary artery disease, congestive heart failure, or severe valvular problems will not tolerate drastic hemodynamic changes seen in severe systemic inflammation. With coronary artery disease, atherosclerosis prevents demand-driven vasodilation that can result in ischemia and myocardial damage in the setting of sustained tachycardia as seen with SIRS. Aside from a history of previous myocardial infarction, coronary artery bypass grafting or percutaneous coronary interventions, coronary disease should be suspected in any patient with diabetes mellitus, smoking history, hyperlipidemia, and peripheral vascular disease.
Congestive heart failure and valvular disease do not drastically change the management of patients presenting with acute surgical issues but may necessitate more invasive hemodynamic monitoring as ongoing resuscitation occurs. Resuscitation should not be limited due to these comorbidities as aggressive resuscitation will likely correct disturbances in low cardiac output. Consideration must be given to heart rate control as tachycardia can lead to inefficient cardiac contractility, pulmonary edema, and hypotension. The development of atrial fibrillation in a patient with or without a cardiac history should cue the surgeon into the fact that the heart is irritated in the current physiologic state.
In a compensated state, the cardiovascular system will maintain a sinus rhythm and an acceptable blood pressure. In states of intravascular depletion, vascular resistance will increase via increased vessel tone to maintain a mean arterial pressure for perfusion of vital organs. This attempt at compensation is seen as a narrowed pulse pressure, as the diastolic pressure is elevated from increased vascular tone and the systolic pressure drops from decreased preload. For maintenance of cardiac output with decreased preload and resultant decreased stroke volume, the heart rate will increase.
Decompensated states of the cardiovascular system can be either obvious or arbitrary. Obvious states are the development of new nonsinus rhythms (e.g., atrial fibrillation) and the occurrence of myocardial ischemia or acute coronary syndromes. Arbitrary decompsensated states lie along the same spectrum of compensated states, but occur further along, such as when a patient has a sinus tachycardia in the 160 bpm range or when mean arterial pressure drops below 55 mm Hg.
Therapeutic interventions begin with the insertion of an arterial line for continuous blood pressure monitoring, frequently followed by central venous catheterization if there is any doubt about the volume status of a patient. Pulmonary artery or Swan-Ganz catheters may be placed if large hemodynamic changes are expected in the setting of known severe aortic or mitral valve dysfunction or if the etiology of hypotension and cardiac dysfunction is unknown. Resuscitation begins with isotonic crystalloid fluids and may need to be supplemented with vasopressors depending on the degree of volume depletion (prolonged vomiting or lack of oral intake), presence of septic response (high cardiac output, peripheral vasodilation, high mixed venous oxygen saturations), and patient parameters such as high central venous pressure in the presence of low mean arterial pressure.
PULMONARY
Relevant respiratory history includes both previous and current smoking, known diagnosis of chronic obstructive pulmonary disease (COPD), pulmonary medications including inhalers or prednisone, or shortness of breath with activity. Patients with COPD may decompensate and develop hypoxemia or hypercapnia and carbon dioxide narcosis. For patients with appreciable pulmonary comorbidities, patients and their families should be aware that mechanical ventilation could be required for days to weeks while the patient’s respiratory status is optimized for extubation following surgery. Septic patients may develop acute respiratory distress syndrome and require low tidal volume ventilation and early tracheostomy.

Full access? Get Clinical Tree








