Paracentesis is the removal of fluid from the peritoneal cavity through the use of a needle for either therapy (to relieve patient symptoms) or diagnosis (to determine causes or complications of ascites). The procedure is generally well-tolerated and simple to perform, especially with the general availability of bedside ultrasound.
DIAGNOSTIC
![]() To analyze abnormal fluid collection in peritoneal space to determine etiology or pathologic conditions (e.g., infection). Most commonly for diagnosis of spontaneous bacterial peritonitis (SBP).
To analyze abnormal fluid collection in peritoneal space to determine etiology or pathologic conditions (e.g., infection). Most commonly for diagnosis of spontaneous bacterial peritonitis (SBP).
THERAPEUTIC
![]() To evacuate ascites for symptomatic relief, usually of shortness of breath and discomfort from abdominal distention. Paracentesis decreased in-hospital mortality 24% when done early (within 24 h of admission) as opposed to later in one large study (Orman ES et.al).
To evacuate ascites for symptomatic relief, usually of shortness of breath and discomfort from abdominal distention. Paracentesis decreased in-hospital mortality 24% when done early (within 24 h of admission) as opposed to later in one large study (Orman ES et.al).
CONTRAINDICATIONS
![]() Absolute Contraindications
Absolute Contraindications
![]() Disseminated intravascular coagulopathy
Disseminated intravascular coagulopathy
![]() Relative Contraindications
Relative Contraindications
![]() Intra-abdominal adhesions
Intra-abdominal adhesions
![]() Abdominal wall cellulitis
Abdominal wall cellulitis
![]() In second or third trimester pregnancy, an open supraumbilical or ultrasound-assisted approach is preferred
In second or third trimester pregnancy, an open supraumbilical or ultrasound-assisted approach is preferred
![]() Exercise caution in coagulopathic or renal failure patients.
Exercise caution in coagulopathic or renal failure patients.
![]() General Basic Steps
General Basic Steps
![]() Prepare patient
Prepare patient
![]() Anesthesia
Anesthesia
![]() Ultrasound
Ultrasound
![]() Perform procedure
Perform procedure
![]() Send for fluid analysis
Send for fluid analysis
LANDMARKS
![]() Preferred approach: 3 cm superior and medial to the anterior superior iliac spine
Preferred approach: 3 cm superior and medial to the anterior superior iliac spine
![]() Stay lateral to the rectus sheath to avoid the inferior epigastric artery. The abdominal wall is also thinner in this location.
Stay lateral to the rectus sheath to avoid the inferior epigastric artery. The abdominal wall is also thinner in this location.
![]() Alternative approach: 2 cm below the umbilicus in the midline. Avoid if the patient has a midline surgical scar.
Alternative approach: 2 cm below the umbilicus in the midline. Avoid if the patient has a midline surgical scar.
TECHNIQUE
![]() Supplies
Supplies
![]() Bedside ultrasound machine, if available
Bedside ultrasound machine, if available
![]() Culture bottles and tubes for cell count, Gram stain, and albumin
Culture bottles and tubes for cell count, Gram stain, and albumin
![]() Have a low threshold to send a cell count with differential, even if the tap is being performed for primarily therapeutic purposes.
Have a low threshold to send a cell count with differential, even if the tap is being performed for primarily therapeutic purposes.
![]() Commercial paracentesis kits containing rigid plastic sheath cannula, if available
Commercial paracentesis kits containing rigid plastic sheath cannula, if available
![]() If a kit is not available, then the following supplies should be obtained:
If a kit is not available, then the following supplies should be obtained:
![]() Iodine or chlorhexidine swabs
Iodine or chlorhexidine swabs
![]() Sterile 4 × 4 gauze
Sterile 4 × 4 gauze
![]() Sterile towels or fenestrated drape
Sterile towels or fenestrated drape
![]() Sterile and nonsterile gloves
Sterile and nonsterile gloves
![]() Sterile 60-cc syringes for collecting fluid sample
Sterile 60-cc syringes for collecting fluid sample
![]() 10-cc syringe for anesthesia
10-cc syringe for anesthesia
![]() 1% to 2% lidocaine (preferably with epinephrine)
1% to 2% lidocaine (preferably with epinephrine)
![]() Skin anesthesia needles
Skin anesthesia needles
![]() 25- or 27-gauge 1.5-inch needle (local anesthesia)
25- or 27-gauge 1.5-inch needle (local anesthesia)
![]() 20- or 22-gauge 1.5-inch needle (local anesthesia)
20- or 22-gauge 1.5-inch needle (local anesthesia)
![]() 18-gauge needle (inoculating specimen tubes)
18-gauge needle (inoculating specimen tubes)
![]() Paracentesis needles
Paracentesis needles
![]() 22-gauge needle for diagnostic taps, 18-gauge needle for therapeutic taps
22-gauge needle for diagnostic taps, 18-gauge needle for therapeutic taps
![]() 1.5 inch should be sufficient, may need 3.5 inch (spinal needle) for obese patients
1.5 inch should be sufficient, may need 3.5 inch (spinal needle) for obese patients
![]() Adhesive bandage
Adhesive bandage
![]() Patient Preparation
Patient Preparation
![]() Direct the patient to urinate or empty the bladder via urinary catheterization
Direct the patient to urinate or empty the bladder via urinary catheterization
![]() Ultrasonography (preferred, but not essential). Bedside ultrasonography is used to verify that the chosen site has a large fluid pocket with no bowel adhesions.
Ultrasonography (preferred, but not essential). Bedside ultrasonography is used to verify that the chosen site has a large fluid pocket with no bowel adhesions.
![]() Sterilize the area where the needle will be inserted with copious povidone–iodine solution or similar surgical prep
Sterilize the area where the needle will be inserted with copious povidone–iodine solution or similar surgical prep
![]() Drape the area with sterile towels or sterile fenestrated drape
Drape the area with sterile towels or sterile fenestrated drape
![]() Patient Positioning
Patient Positioning
![]() If there is a large amount of ascites, the patient may be placed in a supine position with the head of the bed slightly elevated
If there is a large amount of ascites, the patient may be placed in a supine position with the head of the bed slightly elevated
![]() Patients with lesser amounts of ascites may be placed in a lateral decubitus position for optimal pooling of fluid. Left lateral decubitus may be ideal, as this is generally the most fluid-rich area.
Patients with lesser amounts of ascites may be placed in a lateral decubitus position for optimal pooling of fluid. Left lateral decubitus may be ideal, as this is generally the most fluid-rich area.
![]() Analgesia
Analgesia
![]() Produce local anesthesia using up to 5 mg/kg of 1% lidocaine with epinephrine
Produce local anesthesia using up to 5 mg/kg of 1% lidocaine with epinephrine
![]() Raise a subcutaneous wheal with a small-bore (25- or 27-gauge) needle, and then generously infiltrate the deeper tissues in the area of the paracentesis needle’s eventual passage using a longer, larger-bore needle
Raise a subcutaneous wheal with a small-bore (25- or 27-gauge) needle, and then generously infiltrate the deeper tissues in the area of the paracentesis needle’s eventual passage using a longer, larger-bore needle
![]() Anesthetize to the depth of the peritoneum
Anesthetize to the depth of the peritoneum
![]() Needle Insertion
Needle Insertion
![]() Standard-sized (1.5-inch) metal needle will be sufficient in most cases
Standard-sized (1.5-inch) metal needle will be sufficient in most cases
![]() A longer (3.5-inch) spinal needle may be necessary in obese patients
A longer (3.5-inch) spinal needle may be necessary in obese patients
![]() For diagnostic taps, a smaller-gauge (22–20 gauge) needle should be utilized to decrease the chance of postprocedural fluid leak
For diagnostic taps, a smaller-gauge (22–20 gauge) needle should be utilized to decrease the chance of postprocedural fluid leak
![]() For therapeutic taps, a larger (18 gauge) needle may be used to hasten fluid evacuation
For therapeutic taps, a larger (18 gauge) needle may be used to hasten fluid evacuation
![]() Attach needle to a 60-mL syringe
Attach needle to a 60-mL syringe
![]() Advance the needle in slow, controlled 5-mm increments with continuous gentle aspiration of the syringe. A “Z-tract” method may be employed to decrease the risk of postprocedural fluid leak (FIGURE 28.1).
Advance the needle in slow, controlled 5-mm increments with continuous gentle aspiration of the syringe. A “Z-tract” method may be employed to decrease the risk of postprocedural fluid leak (FIGURE 28.1).
![]() Overlying skin is pulled by an assistant or by the non–needle bearing hand 2 cm in the caudal direction
Overlying skin is pulled by an assistant or by the non–needle bearing hand 2 cm in the caudal direction
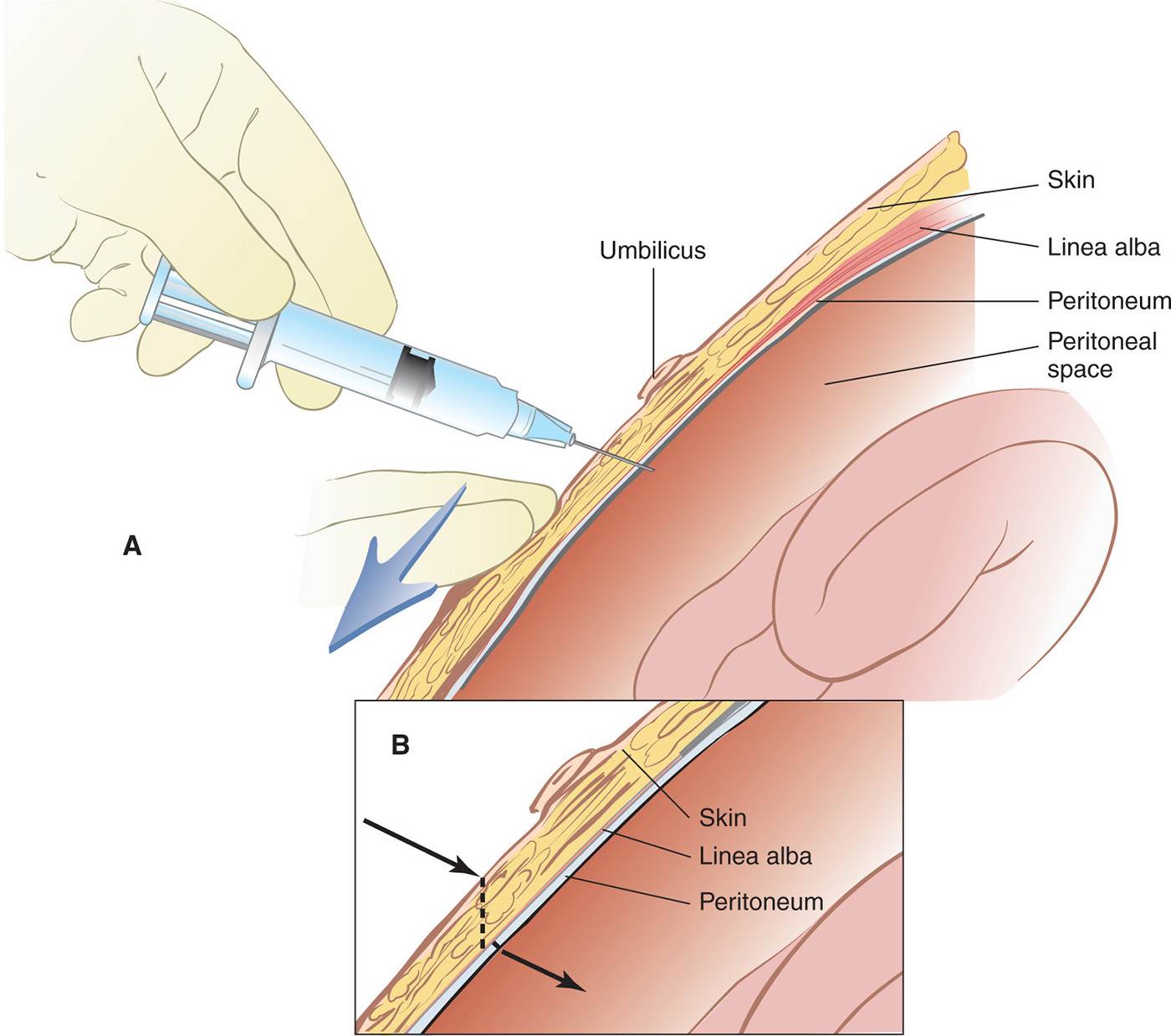
FIGURE 28.1 Z-track formation and controlled removal of ascetic fluid. A: Needle insertion with caudal traction on overlying skin. B: Z-track formation after release of skin and removal of needle. (From Lane NE, Paul RI. Paracentesis. In: Henretig FM, King C, eds. Textbook of Pediatric Emergency Procedures. Philadelphia, PA: Williams & Wilkins, 1997:924, with permission.)

Full access? Get Clinical Tree


