Pain of Cranial Nerve and Cervical Nerve Origin Other Than Primary Neuralgias
Nikolai Bogduk
C2 OR C3 NERVE COMPRESSION
International Headache Society (IHS) code and diagnosis: 13.12 Constant pain caused by compression, irritation, or distortion of cranial nerves or upper cervical roots by structural lesions
WHO code and diagnosis: G44.848
Short description: Headaches caused by a lesion that compresses or otherwise compromises the C2 or C3 spinal nerves or their roots. The majority of reported cases, however, have involved the C2 nerve.
Other terms: C2 neuralgia
ANATOMY AND PATHOLOGY
The C3 spinal nerve occupies a typical intervertebral foramen and is vulnerable to any of the causes of foraminal stenosis: disc herniation, spondylosis, zygapophysial osteoarthrosis, etc. However, such disorders are relatively uncommon at the C2 to C3 level.
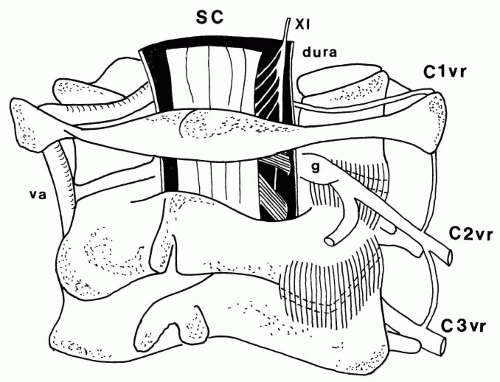
The C2 spinal nerve is relatively immune to entrapment or compression because, unlike the typical spinal nerves, it does not run in an intervertebral foramen. Consequently, it is not subject to the hazards of intervertebral disc herniation or spondylosis. Nor is it vulnerable to compression during extension injuries of the neck because the height of the articular pillars of C1 and C2 protects it from compression by the posterior arch of the atlas (6). The C2 nerve runs behind the lateral atlantoaxial joint, resting on its capsule (7,8) (Fig. 126-1). Inflammatory or other disorders of the joint may result in the nerve becoming incorporated in the fibrotic changes of chronic inflammation (40,64).
Otherwise, the C2 spinal nerve and its roots are surrounded by a sleeve of dura mater and a plexus of epiradicular veins, lesions of which can compromise the nerve. These include meningioma (51) and neurinoma (40), but most reported cases have involved vascular abnormalities ranging from single or densely interwoven dilated veins surrounding the C2 spinal nerve and its roots (39) to U-shaped arterial loops or angiomas compressing the C2 dorsal root ganglion (31,39,40). Nerves affected by vascular abnormalities exhibit a variety of features indicative of neuropathy, such as myelin breakdown, chronic hemorrhage, axon degeneration and regeneration, and increased endoneurial and pericapsular connective tissue (39). It is not clear, however, whether the vascular abnormality causes these neuropathic changes or is only coincident with them.
PATHOPHYSIOLOGY
The pathophysiology of C2 neuralgia is unknown, but the neuralgic quality of pain strongly implies a neurogenic basis. Ectopic, nociceptive impulses could be generated by ischemia or mechanical compression of the dorsal root ganglion.
CLINICAL FEATURES
IHS diagnostic criteria for compression of cervical nerves (Revised International Classification of Headache Disorders [ICHD II]) (30)
A. Constant and/or jabbing pain in the territory supplied by a cervical nerve, fulfilling criteria C and D.
B. Evidence of compression, irritation, or distortion of the appropriate nerve.
C. Pain and compression, irritation, or distortion occur simultaneously and correspond in location.
D. Pain is relieved by removal of the cause of compression, irritation, or distortion.
C2 neuralgia is a distinctive condition characterized by intermittent, lancinating pain in the occipital region
associated with lacrimation and ciliary injection. The pain typically occurs in association with a background of dull occipital pain and dull, referred pain in the temporal, frontal, and orbital regions. Most often, this latter pain is focused on the frontoorbital region but encompasses all three regions when severe. The distinguishing feature of this condition is a cutting or tearing sensation in the occipital region, which is the hallmark of its neurogenic basis.
associated with lacrimation and ciliary injection. The pain typically occurs in association with a background of dull occipital pain and dull, referred pain in the temporal, frontal, and orbital regions. Most often, this latter pain is focused on the frontoorbital region but encompasses all three regions when severe. The distinguishing feature of this condition is a cutting or tearing sensation in the occipital region, which is the hallmark of its neurogenic basis.
The frequency of attacks varies from four to five per day to two to seven per week, alternating with pain-free intervals of days, weeks, or months (39,40). Approximately 75% of patients suffer the associated features of ipsilateral conjunctival and ciliary injection and lacrimation (39,40). Blurred vision, rhinorrhea, and dizziness are less common accompaniments. Neurologic examination is normal. In particular, hypoaesthesia in the territory of the trigeminal or cervical nerves is not present.
C2 neuralgia is distinguished from occipital neuralgia and referred pain from the neck by its neurogenic quality, its periodicity, and its association with lacrimation and ciliary injection. The latter association has attracted the appellation of clusterlike headache (51).
The cardinal diagnostic feature is complete relief of pain following local anaesthetic blockade of the suspected nerve root, typically the C2 spinal nerve, but occasionally the C3 nerve. These blocks are performed under radiologic control and employ discrete amounts (0.6 to 0.8 mL) of long-acting local anaesthetic to block the target nerve selectively (40).
Plain radiographs, computed tomography (CT), myelo-CT, or myelography reveal no suggestion of these lesions. No provocative test reveals arterial lesions (39), but in most patients with venous lesions, challenge with 0.8 mg nitroglycerin provokes an attack of pain, and conversely, inhalation of 100% O2 at 10 L/min for 5 minutes relieves the pain (39).
MANAGEMENT
There is no evidence that C2 neuralgia responds to pharmacotherapy (39). Surgery appears to be the only definitive means of treatment. Nerves entrapped by scarring may be liberated (64); meningiomas may be excised (51). With respect to vascular lesions, resection of the vascular abnormality alone does not reliably relieve the pain; resection or thermocoagulation of the nerve appears to be necessary to guarantee relief of pain (39). However, data on long-term outcomes after thermocoagulation have not been published.
ACUTE HERPES ZOSTER
IHS code and diagnosis: 13.15.1 Head or facial pain attributed to acute herpes zoster
WHO code and diagnosis: G44.881
Short description: pain in the head or face associated with acute herpes zoster infection
EPIDEMIOLOGY
ANATOMY AND PATHOLOGY
Herpes zoster is a disease of dorsal root ganglia characterized by a vesicular eruption in the affected dermatome. It is a reactivation of a latent infection by the varicella virus (58,66). The thoracic nerve roots are most commonly affected (66), but about 12% of presentations involve the cervical spinal nerves, and 13% involve the trigeminal nerve (68). The ophthalmic division is affected in 80% of trigeminal presentations. The pathology of the disease involves inflammation, hemorrhage, and necrosis of the affected ganglion and dorsal horn, with intranuclear inclusion bodies in satellite cells and ganglion cells (58). Pathologic changes may extend from the dorsal root ganglion into the spinal cord or into the peripheral nerve (98).
PATHOPHYSIOLOGY
The mechanism of pain is unknown but possibly involves ectopic discharges from the affected dorsal root ganglion cells (66).
CLINICAL FEATURES
IHS diagnostic criteria for herpes zoster (ICHD-II) (30)
A. Head or facial pain in the distribution of a nerve or nerve division and fulfilling criteria C and D.
B. Herpetic eruption in the territory of the same nerve.
C. Pain precedes herpetic eruption by <7 days.
D. Pain resolves within 3 months.
The onset of acute herpes zoster is usually heralded by pain that precedes the vesicular eruption by a few days. When the trigeminal or C2 ganglion is affected, the pain occurs in the forehead or occipital region; however, no practical method has been found to establish the diagnosis when pain is the only feature. The condition declares itself once the vesicular eruption occurs. In rare instances the geniculate ganglion can be affected, presenting with otalgia or facial pain before the eruption of vesicles in the external auditory meatus and palate (34).
PROGNOSIS
The usual course of herpes zoster infection is that the vesicles dry out within about 1 week and heal within about 1 month (58,66). When the nasociliary nerve is affected, uveitis, keratitis, and iridocyclitis are complications that may threaten vision as well as cause ocular pain.
MANAGEMENT
The mainstay of treatment has become the administration of oral antiviral agents, such as acyclovir, valacyclovir, or famciclovir. All three drugs reduce acute pain, speed rash healing, shorten the period of viral shedding, and shorten the duration of pain, compared with placebo (22,38,43, 44,103). Guidelines recommend that these drugs be used in patients of any age presenting with ophthalmic involvement within the first 72 hours after onset of rash, and in any patients with active zoster affecting the neck, limbs, and perineum (41,45). A newer agent, brivudine, has proved superior to acyclovir in reducing the period of new blister formation and shortening the period of acute pain (67).
Antiviral therapy also decreases the subsequent incidence of postherpetic neuralgia by about 80% (22,38,43, 44,103). Nevertheless, despite adequate therapy, 20% of patients continue to suffer pain (44).
Simple analgesics are not of proven benefit for the relief of pain (58,66). Tramadol, however, was superior to placebo in a controlled study (9), and tricyclic antidepressants can relieve residual pain when added to a regimen of antiviral agent (42). Furthermore, amitriptyline reduces the incidence of postherpetic neuralgia (10). Finally, systemic steroids have been used for acute herpes zoster, particularly ophthalmic herpes, but they have no demonstrable effect on reducing pain, although they do seem to help in improving quality of life (22,44,100,102).
Sympathetic nerve blocks are advocated by some, but the literature is devoid of sufficiently powerful controlled trials and remains divided (2,41,42,58,66,105). For patients with severe pain, one study has shown that epidural infusion of bupivacaine and methylprednisolone over 7 days is more effective than intravenous acyclovir combined with prednisolone (63). Epidural therapy also reduces the incidence of postherpetic neuralgia.
POSTHERPETIC NEURALGIA
IHS code and diagnosis: 13.15.2 Postherpetic neuralgia
WHO code and diagnosis: G44.847
Short description: Postherpetic neuralgia is a neuralgic pain that persists in the affected dermatome long after the vesicular eruption of acute herpes zoster has healed.
EPIDEMIOLOGY
About 16% of patients continue to have pain at 6 months after the onset of herpes zoster, and between 5 and 10% still have pain at 12 months (42,43,81). Risk factors for postherpetic neuralgia are severe or prolonged prodromal pain, moderate to severe acute pain, severe rash, and advanced age (11,43,44). More than 60% of patients older than 60 years develop pain, and up to 50% or more suffer pain lasting more than 1 year (66,96).
ANATOMY AND PATHOLOGY
The pathology of postherpetic neuralgia involves atrophy of the dorsal horn and cell loss, axon loss, and demyelination with fibrosis in the dorsal root ganglion (98). These changes appear to be specific for patients with pain, whereas demyelination and axon loss in the affected
peripheral nerve occur in patients both with pain and without pain (98).
peripheral nerve occur in patients both with pain and without pain (98).
PATHOPHYSIOLOGY
The pathophysiology of postherpetic pain is unknown but may involve central deafferentation rather than mechanisms in the peripheral nerves or sensory ganglia (66).
CLINICAL FEATURES
IHS diagnostic criteria for chronic postherpetic neuralgia (ICHD-II) (30)
A. Head or facial pain in the distribution of nerve or nerve division and fulfilling criteria C and D.
B. Herpetic eruption in the territory of the same nerve.
C. Pain precedes herpetic eruption by <7 days.
D. Pain persists after 3 months.
The pain is archetypical of neuralgia, characterized by constant burning and aching with superimposed jabs of shooting or lancinating pain. The skin of the affected dermatome is hypoaesthetic but may involve zones of hyperaesthesia from which attacks of pain may be triggered by light touch or brushing (96). Midthoracic dermatomes and the first-division trigeminal nerve are most commonly affected (96).
MANAGEMENT
Amitriptyline and related tricyclic antidepressants (nortriptyline, desipramine) have been the most widely used and most thoroughly studied agents for the treatment of postherpetic neuralgia. The odds ratio for these drugs having a beneficial effect is 0.15 (92), and the number needed to treat is between two and four (44). The recommended regimen (for amitriptyline) is to start with 10 mg at bedtime and progress to 25 mg to 150 mg as needed (5). However, only between 47% and 67% of patients respond (5,47,74).

Full access? Get Clinical Tree