Chapter 106 Paediatric cardiopulmonary resuscitation
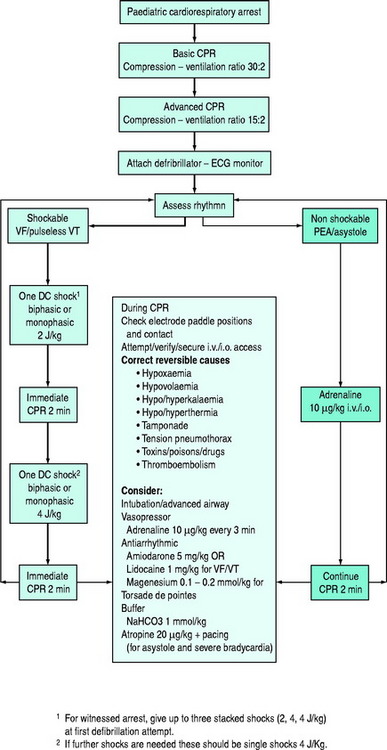
This chapter concerns basic and advanced cardiopulmonary resuscitation (CPR) for infants and children (Figure 106.1). The essentials of resuscitation of the ‘newly-born’ (at birth) infant are also provided (Figure 106.2). The recommendations are based on guidelines published by several authoritative resuscitation organisations1–3 which are in turn derived from an extensive evaluation of the science of resuscitation conducted by the International Liaison Committee on Resuscitation.4
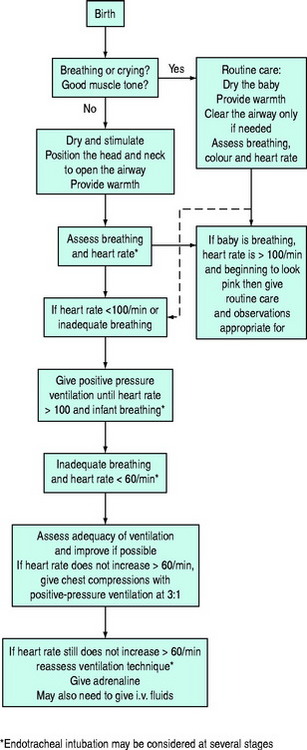
Figure 106.2 Newly-born infant resuscitation.
(Reproduced with permission from the Australian Resuscitation Council, Melbourne.)
BASIC LIFE SUPPORT
RESCUE BREATHING (EXPIRED AIR RESUSCITATION)
If inadequate breathing is present, rescue breathing (expired air resuscitation) or bag-valve-mask ventilation should be commenced immediately. There is no evidence to dictate the number of initial breaths. However, at least two breaths are recommended by all resuscitation organisations, with some stating up to five. While maintaining the airway, slow breaths over 1–1.5 seconds should be given with enough air to achieve adequate chest inflation. In children of all sizes, a mouth-to-mouth technique is possible by pinching the nostrils closed. In newly-born and infants, a mouth-to-mouth-and-nose technique is recommended, but if the rescuer has a small mouth, a mouth-to-nose technique is an alternative. Lack of chest rise may signify obstruction of the airway requiring repositioning of the head and neck.
RATES OF COMPRESSION AND RATIO OF COMPRESSION TO VENTILATION
For infants and children, compressions should be delivered at a rate of 100/min, i.e. one compression every 0.6 seconds or approximately two per second. This does not mean that 100 actual compressions are given each minute. When ventilation is interposed between compressions, the actual compressions delivered will be less than 100 each minute.