Chapter 2 Outreach
CRITICAL CARE OUTREACH
A key innovation in critical care has been the development of dedicated outreach and medical emergency/rapid response services aiming ‘to ensure equity of care for all critically ill patients irrespective of their location’.1
Outreach is multidisciplinary ‘collaboration and partnership between critical care and other departments to ensure a continuum of care for patients and to enhance the skills and understanding of all staff in the delivery of critical care’.2 Outreach services primarily focus on patients with potential or actual critical illness on general wards. They are not a substitute for insufficient critical care beds, poor ward facilities or inadequate staffing.
BACKGROUND
Many patients who require critical care are on a ward for part of their hospital admission. Comparison of outcomes of patients admitted to a critical care unit from the emergency department, operating theatre/recovery area and wards shows that the highest number of deaths is found in patients admitted from wards.3 The longer patients are in hospital before admission to critical care, the higher their mortality.4 Reports from many countries show that hospital patients frequently suffer adverse events and that these events can cause major morbidity or death.5 Suboptimal treatment is common before admission to critical care and is associated with worse outcomes.6 Crucially, the baseline characteristics of patients who receive suboptimal care are not significantly different from those who are well managed. Differences in mortality are attributable to differences in the quality of care rather than differences between patients themselves. Many factors are implicated, including lack of knowledge and failure to appreciate clinical urgency and to seek advice, compounded by poor organisation, breakdown in communication and inadequate supervision.
About one-quarter of all ‘critical care deaths’ occur after patients have been discharged back to wards from critical care. Patients discharged inappropriately early have an increased mortality.7,8 There are also deaths among surgical patients who have returned to the ward following surgery without ever being admitted to critical care.
OUTREACH SYSTEMS
Medical emergency teams (METs) were first introduced in Australia in 1990. METs expanded the role of the hospital cardiac arrest team to include the pre-arrest period, with call-out criteria generally based upon markedly deranged physiological values.9 In the UK, critical care outreach (CCO) services became relatively widespread following negative publicity about shortages of critical care facilities and the national review of critical care services in 2000.10 This led to some additional funding for critical care beds and outreach services. Other countries have also recognised the needs of critically ill patients outside designated critical care areas and have introduced their own systems to address these problems.
There are now many models and a variety of terms for outreach services.11,12 Some organisations have enthusiastically embraced the concept whereas others have reservations. METs are usually physician-led, while CCO teams and rapid response teams (RRTs) are typically nurse-led but may include physiotherapists and other allied health professionals as well as doctors. Most teams respond to defined triggers, although some, particularly CCO services, also work proactively with known at-risk patients such as intensive care unit (ICU) discharges.
These systems have the following features in common:
The aim is to prevent unnecessary critical care admissions, to ensure timely transfer to critical care when needed, to facilitate safe discharge from critical care back to the ward, to share critical care skills and to improve standards of care throughout the hospital. There may also be a role in outpatient support for patients and their families after hospital discharge (Table 2.1).
Table 2.1 Functions of critical care outreach
• Education for ward staff in recognition of fundamental signs of deterioration, and in understanding how to obtain appropriate help promptly • Development of systems of coordinated, collaborative, continuous care of critically ill and recovering patients across the hospital and also in the community |
| Together, these elements comprise a system to deliver safe, quality care by proactive management of risk and timely treatment of critical illness |
RECOGNISING CRITICAL ILLNESS
Critically ill patients are identified by review of the history, by examination and investigations. Higher risks are associated with extremes of age, with significant comorbidities or with serious presenting conditions. Outcome is often related to and can be predicted by abnormal physiology. Many studies show patients have abnormal physiology for hours and sometimes days before critical events such as cardiopulmonary arrest.13–18 However, measuring and recording of vital signs on general wards are often inadequate.19
A physiologically based system for identifying critical illness should have certain attributes (Table 2.2).
Table 2.2 Ideal attributes of an early-warning (track and trigger) scoring system
| Timely | Measurable |
| Reliable | Reproducible |
| Inexpensive | Non-invasive |
| Repeatable | Safe |
| Accurate | Independent of disease state |
For early recognition of hospital patients to be effective:
ABNORMAL PHYSIOLOGY AND ADVERSE OUTCOME
There is an association between abnormal physiology and adverse outcome. Critical care severity scoring systems such as Acute Physiology, Age and Chronic Health Evaluation II (APACHE II)20 are based on this relationship. Patients who suffer cardiopulmonary arrest or who die in hospital generally have abnormal physiological values recorded in the preceding period, as do patients requiring transfer to the critical care unit.
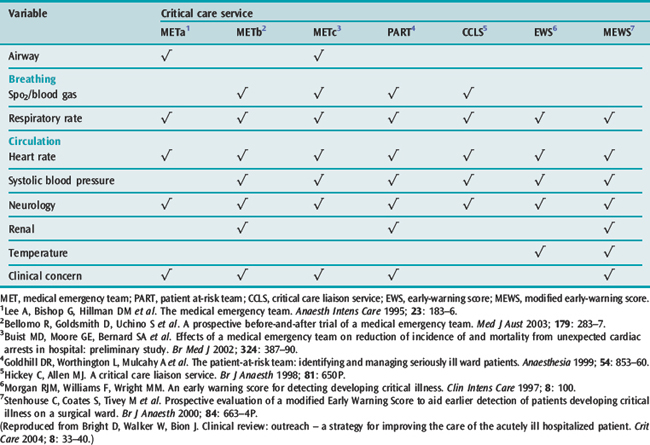
It therefore follows that vital signs can predict many adverse events. These principles have been incorporated into a number of early-warning scoring (EWS) systems. The systems incorporate different combinations of physiological parameters, a range of approaches to scoring and various trigger thresholds. Examples of the variables included in a few of the scoring systems are given in Table 2.3.
Table 2.3 Variables used by different scoring systems to trigger referrals to a critical care service

Full access? Get Clinical Tree






