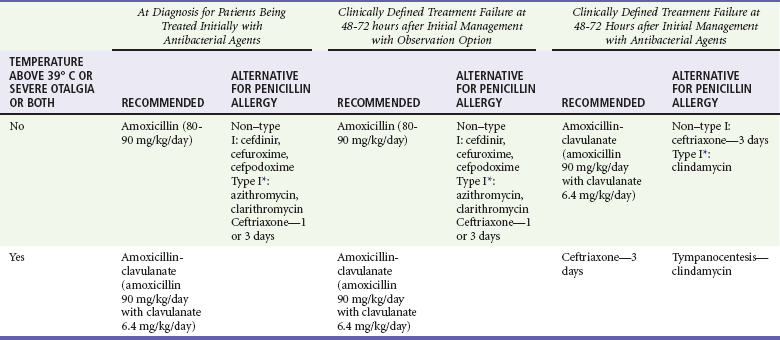
Chapter 72 Otitis media (OM) is the most common diagnosis made by U.S. physicians for children younger than 15 years. In 2002, 16.7 million visits were made to physician offices across the country for OM, with an estimated 2.65 million visits made to emergency departments (EDs), making it the sixth most common ED discharge diagnosis.1 More than 80% of children will have at least one episode of acute otitis media (AOM) during their lifetime, and by age 3, up to 40% will have had at least three episodes. The financial repercussions are enormous; one estimate is that $5 billion per year is spent on the evaluation, treatment, and socioeconomic effects of OM.2 The most frequent outpatient use of antimicrobials in the United States is for OM, with the number of prescriptions having increased from 12 million in 1980 to more than 23.6 million in 1992. The most common causes of bacterial infection in children are Streptococcus pneumoniae, Haemophilus influenzae (primarily nontypeable), and Moraxella (Branhamella) catarrhalis. Streptococcus pyogenes, Staphylococcus aureus, and gram-negative bacteria are much less common.3 The widespread use of the pneumococcal 7-valent conjugate vaccine (Prevnar) has changed the frequency of these common organisms, with H. influenzae increasing in frequency,4 particularly in persistent AOM and treatment failures.5 As the advent of reverse transcriptase polymerase chain reaction technology and other techniques for viral identification has improved, the number of viral agents identified in the middle ear has increased. In a study of 79 patients with tympanostomy tubes with OM, bacteria were found in 92% of the patients, viruses in 70%, and both viruses and bacteria in 66%.6 Respiratory syncytial virus is the most common virus, but parainfluenza virus, influenza virus, rhinovirus, and adenovirus have also been found in the middle ear aspirates of children. Some authors believe that viral infection is the cause of the inflammatory reaction in most cases and antibiotics are not necessary.7 Viruses have contributed to poor treatment outcome by increasing middle ear inflammation, decreasing neutrophil function, and decreasing antibiotic penetration into the middle ear.8 The clinical implications of this are that antibiotic treatment may not be predictable, and a failed course of antibiotic treatment may not be promptly blamed on antibiotic-resistant bacteria, leading to continuous changes in antibiotic regimens.8 In young children, it was formerly believed that gram-negative organisms and S. aureus were the causative organisms. Although these bacteria may be the causes in intubated patients or patients in the neonatal intensive care unit, healthy newborns tend to be infected by the same pathogens as healthy older children. Bullous myringitis produces bullae on the tympanic membrane (TM) and may be present in up to 5% of cases of OM in children younger than 2 years.9 Although bullous myringitis was previously thought to be caused by Mycoplasma pneumoniae, culture of middle ear aspirates in this condition generally grows the usual organisms that cause AOM, and M. pneumoniae is uncommon.10 More than 70% of children with purulent conjunctivitis may have OM, a symptom complex described as the otitis-conjunctivitis syndrome, which is predominantly caused by H. influenza.11 Other, less likely organisms that can cause AOM include Mycobacterium tuberculosis (primarily in children) and Chlamydia trachomatis (most commonly seen in children younger than 6 months with pneumonia). Up to 10% of the general pediatric population may be at risk for developing four or more episodes of OM in the first year of life; these children are generally said to be otitis-prone.12 They may have subtle immunologic abnormalities or a greater baseline colonization of virus and bacteria than the general population. OM may manifest with a multitude of symptoms, such as cough, upper respiratory tract symptoms, poor appetite, diarrhea, vomiting, fever, and pulling at ears and ear pain, all of which are nonspecific. Of all these symptoms, pain seems to be the most useful for making the diagnosis of AOM. In one systematic review, ear pain had a positive likelihood ratio (3-7.3) but was present in only 50 to 60% of children with AOM.13 Fever may be present, but in one large series, a temperature of 38.3° C or greater was present in only 26% of the episodes, with only 4% of cases involving a fever of 40° C or greater. The auricle and external canal should be inspected for signs of erythema, discharge, or tenderness. If the canal is occluded with cerumen, curettage may be successful; if not, the placement of 3% hydrogen peroxide or emulsifying drops, followed by gentle irrigation, may cleanse the canal. A bulging TM increases the likelihood of AOM, whereas a retracted TM is seen in chronic OME. The color may be red, pink, yellow, or a normal pearly gray or translucent. The presence of erythema in itself does not indicate infection because crying or fever may cause hyperemia; however, a TM that is distinctly red (defined as hemorrhagic, strongly or moderately red) suggests AOM.13 Intratemporal.: TM perforation occurs most commonly at the pars tensa and usually resolves spontaneously. It may persist for a longer period, resulting in a chronic perforation, chronic OM, or both. Chronic otitis media refers to inflammation of the middle ear that persists for 6 weeks or longer accompanied by discharge through perforation of an intact membrane.14 Cholesteatoma is an accumulation of keratin-producing squamous epithelium in the middle ear and may result in erosion of bone within the middle ear cavity. It is seen most often in OME, in which retraction of the TM is a common problem, and its presence may alter the courses of some treatment therapies. Intracranial.: Meningitis is the most common intracranial complication of AOM, resulting from hematogenous spread and direct invasion. Brain abscesses are most commonly caused by chronic otitis and are the second most common intracranial complication.15 Extradural abscesses, subdural empyema, and lateral venous sinus thrombosis have all been identified as complications of OM. Physicians in the Netherlands in the early 1990s suggested that OM was a self-limited disease and recommended observation as an initial treatment option, followed by the use of antibiotics if the patient’s condition did not improve within 72 hours. With these practice recommendations, the concern for rising rates of antibacterial resistance, and the growing costs of antibacterial preparations in the United States, the American Academy of Pediatrics (AAP) and the American Academy of Family Physicians developed guidelines for the diagnosis and management of AOM to assist physicians in clinical decision-making. The guidelines recommend an age-stratified approach that incorporates age with a combination of diagnostic certainty and illness severity.16 The introduction of the guidelines was not without controversy, with some authorities voicing concerns that the clinical trials used in decision-making lacked stringent diagnostic criteria, did not include very young children, or used antimicrobial drugs that had limited efficacy or were given in suboptimal doses. The components of these guideline include diagnosis, the management of pain, observation, and antibiotic recommendations. Making the diagnosis of AOM can be challenging but critical. One study suggested that physicians were uncertain of their diagnosis of AOM as much as 40% of the time.17 This lack of confidence may contribute to the unnecessary use of antibiotics. Making a diagnosis of AOM requires three findings: (1) history of acute onset, (2) signs of middle ear effusion (including TM immobility), and (3) signs or symptoms of middle ear inflammation. AOM can cause substantial pain, which should be appropriately addressed. Acetaminophen and ibuprofen are safe over-the-counter medicines that are first-line analgesics. The use of narcotic analgesia has not been well studied. Benzocaine-antipyrine, a local anesthetic, may be helpful in some patients with an intact TM and has been shown to be more effective than placebo.18 There is evidence that children younger than 2 years, those with bilateral OM, or those with otorrhea gain the greatest benefit from antibiotic treatment,19 but because more than 80% of cases of AOM resolve spontaneously, the use of observation versus antibiotics has been advocated. This approach of “watchful waiting” for 48 hours has resulted in lower rates of antibiotic-resistant bacteria.20 The observation option has been restricted to children older than 6 months. In children older than 6 months to 2 years, treatment recommendations are based on the certainty of the diagnosis and severity of illness, with observation as an option if the diagnosis is uncertain. In children older than 2 years, treatment is necessary only in patients with severe illness, defined as severe otalgia or temperature higher than 39° C. Unless severe illness is present, children older than 2 years should be clinically observed. Table 72-1 summarizes the AAP recommendations. Table 72-1 Clinical Practice Guidelines: Diagnosis and Management of Acute Otitis Media AOM, acute otitis media; TM, tympanic membrane. Type I sensitivity—urticaria or anaphylaxis. From American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media: Diagnosis and management of acute otitis media. Pediatrics 113:1451, 2004. Observation recommendations are also based on the reliability of the caregivers and ability for close follow-up. If there is concern about the ability to get follow-up, parents can be given a prescription to be filled if the patient’s condition does not improve within 48 hours, a so-called “safety net prescription.”21 Several studies in the ED have shown success with use of this approach.22,23 An analysis from the National Ambulatory Medical Care Survey revealed that management without antibiotics has not increased since the guidelines were published, although children who did not receive antibiotics were more likely to have mild infections.24 The decision to treat is balanced against the medication’s adverse effects, which may include allergic reactions, gastric upset, accelerated bacterial resistance, and unfavorable changes in the bacterial flora. Several large systematic reviews revealed that antibiotics are modestly more effective than no treatment but that 4 to 10% of children experienced adverse effects from the treatment itself.25,26 Two recent randomized controlled trials comparing amoxicillin-clavulanate versus placebo in a total of 610 patients reported modestly improved time to resolution of symptoms and otoscopic findings but with more side effects, diarrhea being the most common.27,28 Although some authorities believe that these studies settled the treatment controversy, the studies were far from conclusive, and observation as recommended by the previously published guidelines remains an acceptable treatment. Amoxicillin’s cost, efficacy, safety profile, and palatability continue to make it a good first-line agent, and the guidelines recommend it as the first-line agent in the non–penicillin-allergic patient.16 It can be given twice a day at a dose of 45 mg/kg. This higher concentration is preferred because it is effective against susceptible and intermediately resistant strains of S. pneumoniae and because 15 to 20% of children have poor gastrointestinal absorption of amoxicillin.29 In patients who are allergic to penicillin, the guidelines distinguish between those with type I sensitivity (urticaria or anaphylaxis) and those with non–type I sensitivity, but second- and third-generation cephalosporins have little cross-reactivity. Options for treatment of patients with non–type I reactions include cefdinir (14 mg/kg/day in one or two doses), cefpodoxime (10 mg/kg once a day), cefuroxime (30 mg/kg/day in two divided doses), and intramuscular ceftriaxone (50 mg/kg/day) as a single injection.16,29 Treatment of patients with type I reactions can include macrolides such as azithromycin (10 mg/kg for one day, then 5 mg/kg for an additional 5 days), clarithromycin (7.5 mg/kg twice a day for 10 days), and clindamycin (7.5 mg four times a day). Patients with severe otalgia or a temperature greater than 39° C should be given amoxicillin-clavulanate (80-90 mg of the amoxicillin component per kilogram per day) or intramuscular ceftriaxone for 1 to 3 days. Patients should be reevaluated in 3 days if the treatment fails. Treatment failure is defined by lack of clinical improvement in signs and symptoms such as ear pain, fever, and TM findings of redness, bulging, or otorrhea. In these cases, treatment includes agents effective against the β-lactamase–producing organisms H. influenzae and M. catarrhalis. Recommended agents include amoxicillin-clavulanate (80-90 mg of the amoxicillin component per kilogram per day) and intramuscular ceftriaxone and clindamycin for 3 days.16 Table 72-2 is a synopsis of the treatment guidelines. Table 72-2 Treatment Guidelines for Otitis Media *Type I sensitivity—urticaria or anaphylaxis. From American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media: Diagnosis and management of acute otitis media. Pediatrics 113:1451, 2004. Recurrent AOM is encountered in roughly 20% of children before age 1 year; 20 to 30% occur within a month after successful completion of therapy.30 These episodes are usually a result of a new pathogen. Patients with AOM in whom treatment with a conventional β-lactam antibiotic has failed and β-lactam–allergic patients with AOM in whom macrolide therapy has failed may benefit from the use of fluoroquinolones, though the lack of liquid suspension and lack of approval in children may limit this treatment option.31 After a 10-day treatment with antibiotics, 50% of children may exhibit OME, but 90% of cases resolve within 3 months. However, about 30 to 40% of children have recurrent OME, and 5 to 10% of cases last 12 months or longer. The treatment of OME is controversial, but OME may interfere with hearing and subsequent development of speech and language. OME is, by definition, asymptomatic, and the effusion may be sterile or contain infectious agents, but there is little benefit derived by antibiotics, and they should not be used.32,33 Antihistamines, decongestants, steroids, or surgical procedures are not beneficial in patients with OME.33 Myringotomy and tympanostomy tubes may be beneficial in children who have had OME for more than 4 months with persistent hearing loss, those with a hearing loss greater than 40 dB, children with structural damage to the TM or middle ear, and children with persistent OM who are at risk for speech, language, or hearing problems.33 Tonsillectomy is not beneficial, but adenoidectomy may be helpful in older children who have a specific indication such as nasal obstruction or chronic adenoiditis. Tympanostomy tube insertion is one of the most common operative procedures among children the United States, and emergency physicians will frequently encounter patients with these tubes. There is no consensus for the most appropriate treatment in a patient with an acutely draining ear. A meta-analysis concluded that there was little high-quality evidence available to identify the most effective treatment.34 The organisms involved are the same ones that cause AOM acutely, particularly in children younger than 2 years, but Pseudomonas aeruginosa, S. aureus, and Staphylococcus epidermidis are also implicated.35 In the acute setting, topical antibiotic administration with 5 oxfloxin drops to the affected ear twice a day or 4 drops of ciprofloxacin-dexamethasone twice a day is an effective treatment.36 Systemic treatment (usually with amoxicillin-clavulanate 45 mg/kg twice a day) should be reserved for patients showing signs of complicated or invasive infections or signs of systemic disease. External otitis is an inflammation of the external auditory canal. There is a lifetime incidence of 10%, and it accounts for 7.5 million annual ototopical prescriptions in the United States.37 The external auditory canal is lined with squamous epithelial cells and cerumen glands that provide a protective lipid layer. This protective layer may be disrupted by high humidity, increased temperature, maceration of the skin after prolonged exposure to moisture, and local trauma (e.g., cotton swabs or the use of hearing aids), resulting in the introduction of bacteria. Otitis externa (OE) is a bacterial disease most commonly caused by P. aeruginosa and S. aureus but can also be polymicrobial.38 Occurring most often in the summer and in tropical climates, it is also known as swimmer’s ear or tropical ear.
Otolaryngology
Otitis Media
Background
Principles of Disease
Etiology
Clinical Features
Complications
Management
AGE
CERTAIN DIAGNOSIS
UNCERTAIN DIAGNOSIS
<6 mo
Antibacterial therapy
Antibacterial therapy
6 mo-2 yr
Antibacterial therapy
Antibacterial therapy;
Observation option if nonsevere illness
>2 yr
Antibacterial therapy
Observation option if severe illness; observation option if nonsevere illness
Otitis Externa
< div class='tao-gold-member'>

Full access? Get Clinical Tree


Otolaryngology
Only gold members can continue reading. Log In or Register to continue




