Opioids
Albert Dahan
Marieke Niesters
Erik Olofsen
Terry Smith
Frank Overdyk
Key Points
Related Matter
Dose-Effect Curves
Drug Concentration and Effect
Vomiting Pharmacology
Introduction
Short History
Opium is among the oldest drugs in the world. Fossilized opium poppies have been found in Neanderthal excavation sites dating back to 30,000 BC. Many old civilizations, including the Sumerians, Egyptians, Greeks, Romans, and Chinese, used opium for nutritional, medicinal, euphoric, spiritual, and religious purposes. The first written reference to the medicinal use of the opium poppy is described in a Sumerian text dated near 4,000 BCE. Just over 200 years ago, the German pharmacist and chemist Friedrich Sertürner isolated a stable alkaloid crystal from the opium sap and named it morphine after the Greek god of dreams, Morpheus.4,5 Morphine was 10-fold more potent than opium and soon replaced it not only for the treatment of severe pain, but also for a myriad of other purposes such as cough and diarrhea. After the invention of the hypodermic syringe in the 1850s, the Englishman Alexander Wood was the first to inject morphine in a controlled fashion into a patient producing more than a day’s sleep (1853).6 The first reported casualty from morphine occurred shortly thereafter when Wood injected his wife with morphine resulting in a fatal overdose from respiratory depression.6 Morphine revolutionized the treatment of the wounded in battlefield medicine, but euphoric and addictive properties led to the addiction of thousands of soldiers to morphine during the American Civil War.
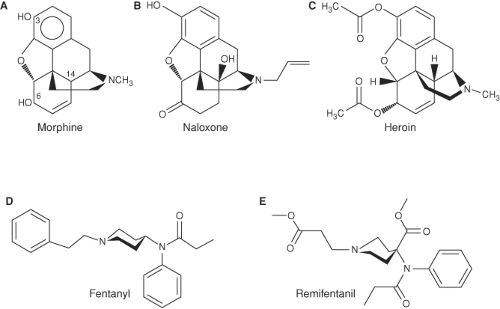
The synthesis of heroin in 1874 was based on the empirical finding that boiling morphine with specific acids caused the replacement of the two morphine –OH groups by –OCOH3 producing diamorphine or heroin (Fig. 19-1).
After the structure of morphine was determined in the 1920s, the synthesis of new morphine-like opioid compounds was based
on chemical principles rather than empirical discoveries. In 1937, meperidine (or pethidine) became the first synthetic opioid synthesized on the basis of the central structure of morphine. Since then many synthetic and semisynthetic opioids have been produced, including the clinically important opioid antagonists naloxone and naltrexone, by replacing the N-methyl substituent in morphine with allyl and cyclopropylmethyl groups, respectively (Fig. 19-1).7
on chemical principles rather than empirical discoveries. In 1937, meperidine (or pethidine) became the first synthetic opioid synthesized on the basis of the central structure of morphine. Since then many synthetic and semisynthetic opioids have been produced, including the clinically important opioid antagonists naloxone and naltrexone, by replacing the N-methyl substituent in morphine with allyl and cyclopropylmethyl groups, respectively (Fig. 19-1).7
For clinical use during anesthesia the most important opioids are the piperidines fentanyl, sufentanil, alfentanil, and remifentanil. These opioids produce potent analgesia and suppression of cardiovascular responses to noxious stimulation from surgery with predictable PK and PD. The latest potent opioid to be registered is tapentadol.8,9 This molecule acts via activation of the opioid receptors at spinal and supraspinal sites and by inhibition of the reuptake of norepinephrine, activating α2-adrenergic receptors in the spinal cord dorsal horn. This produces a synergistic analgesic effect with a more desirable gastrointestinal (GI) side effect profile. The continued development of opioids with complex simultaneous actions at opioid and non-opioid target sites is facilitated by new information gained about mechanisms involved in endogenous pain and analgesia as well as advances in pain-related pharmacology. Development of new opioids is also driven by concerns that the side effect profile of potent opioids, which presents a serious risk to patients, needs to be minimized.
The Endogenous Opioid System
A major breakthrough in the understanding of opioid pharmacology came from a series of discoveries of opioid receptors, endogenous opioid peptides, their encoding genes, and endogenous opioid alkaloids. The endogenous opioid system is composed of a family of structurally related endogenous peptides that act at a four-member opioid receptor family consisting of the μ-opioid receptor (MOR), κ-opioid receptor (KOR), δ-opioid receptor (DOR), and orphanin FQ/nociception (NOP) receptor.10,11 This opioid system is involved in a variety of regulatory functions including important roles in nociceptive, stress, emotional, and hedonic responses and modulation of thermoregulation, breathing, neuroendocrine function, GI motility, and immune responses. Various subtypes of opioid receptors have also been identified, with different pharmacologic functions. For example, at least three MOR subtypes have been described: μ1 is predominantly involved in opioid analgesia, μ2 is involved in opioid-induced respiratory depression, and μ3 is involved in opioid-induced immune suppression.12,13 Note, however, that the functional validation of most opioid receptor subtypes awaits the development of antagonists with sufficient selectivity to allow a clear differentiation by effect.
Opioids act not only through central and peripheral neuronal pathways, but also via non-neuronal mechanisms, such as actions on the immune system.16 Morphine and morphine-6-glucuronide (M6G), endogenously formed and stored in adrenal chromaffin cells and leukocytes, play an import role as modulators of non-neuronal responses in the immune system.17 Our considerations of endogenous opioid systems, therefore, have expanded from an opioid peptide system present in the central nervous system (CNS) and peripheral nervous system to include various peptide and non-peptide ligands in neuronal and non-neuronal cells throughout the body.
Opioid receptors are linked to G proteins in the cell membrane and are hence members of the large G-protein–coupled receptor (GPCR) family.18 GPCRs mediate a cascade of downstream signaling pathways leading to (i) the inhibition of adenyl cyclase and decreased cyclic AMP, (ii) activation of Ca2+ and K+ channels, and (iii) activation of MAPK/ERK, PKC, and P13 K/Akt.19 Interactions between opioid ligands and selective receptors have a number of important clinical effects. Morphine-induced analgesia and respiratory depression are both induced through activation of the MOR and subsequent activation of the adenylate cyclase/cyclic AMP pathway.20 Recently, opioid-induced activation of alternate cell signaling pathways through interactions with many (opioid and non-opioid) receptor types have been shown to affect the growth and distribution of cancer cells.19,21
Opioid Receptor Knockout Mice
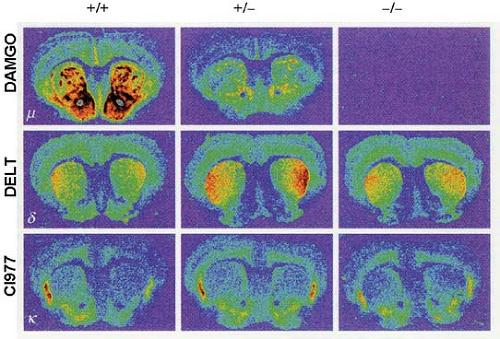
In the last decade a variety of mice lacking the various opioid receptors (“knockout mice”) have been bred to understand the molecular targets of exogenous opioids (Fig. 19-2).10 Inactivation of the μ-, κ-, and δ-opioid receptors, either separately or in combination, is not lethal. This suggests that the opioid receptor system is not crucial for development but is critical when experiencing stress or pain. For example, under conditions of fight or flight, recruitment of the endogenous opioid system will result in development of endogenous analgesia allowing the subject to respond to an acute body insult and consequently increases the chance of survival.
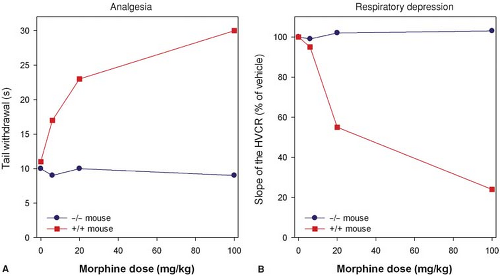
Studies indicate that morphine’s action at the MOR gene produces its clinical effects. Mice lacking the MOR gene do not experience morphine-induced analgesia, respiratory depression, reward and withdrawal, inhibition of GI transit, immunosuppression, or an increase in steroid hormones (Fig. 19-3).22,23,24 Analgesic responses after administration of other opioids, such as morphine’s metabolite M6G, are also absent in MOR knockout mice.25 These observations suggest the MOR is the target for both the desired and undesired effects of opioid analgesics and consequently designing a MOR activating drug that selectively produces desired effects such as analgesia, but not undesired effects such as life-threatening respiratory depression, is not possible.
Classification of Exogenous Opioids
Opioids may be classified on the basis of their synthesis, chemical structure, potency, receptor binding, and effect at the opioid receptors. According to their synthesis opioids are subdivided into natural (morphine), semisynthetic, and synthetic opioids. Natural opioid alkaloids are known as opiates, while the term opioids is used for all opioids (endogenous opioid peptides, natural opioid alkaloids, semisynthetic opioids, and synthetic opioids).
Semisynthetic opioids are derived from the morphine molecule and include buprenorphine, codeine, etorphine, heroin, hydromorphone, oxycodone, and oxymorphone. The synthetic opioids comprise the piperidines (e.g., loperamide, meperidine, alfentanil, fentanyl, sufentanil, remifentanil) and the methadones (e.g., methadone, dextro-propoxyphene).
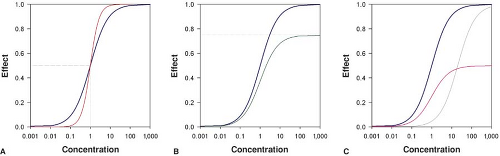
Opioids may be full agonists which cause the maximum possible effect when activating their receptors. Opioid full agonists at the MOR include morphine, piperidines, and methadone. Opioid partial agonists activate their receptor but cause only a partial or reduced effect (Fig. 19-4). Buprenorphine acts as a partial agonist at the MOR while it is a full agonist at the NOP and DOR.26 In clinical practice buprenorphine behaves as a full agonist with respect to pain relief yet its respiratory depressant effects are limited and display a “ceiling effect”.27 At the KOR buprenorphine acts as a competitive antagonist, which classifies this opioid also as a mixed agonist–antagonist. Naloxone and naltrexone are opioid antagonists.
A more practical classification of opioids is their subdivision into agents with a rapid onset and offset of action (e.g., remifentanil and alfentanil) and agents with a slow onset/offset of action (e.g., morphine and buprenorphine). The concept of onset/offset of action will be discussed below.
Opioids Acting at Opioid and Non-opioid Receptors
Most opioid analgesics act at multiple receptor systems with different affinities. For example, morphine acts with high affinity at the MOR and with lower affinities at the KOR and DOR. Various opioids including methadone, dextro-propoxyphene and ketobemidone are opioid analgesics and also antagonists at the N-methyl-D-aspartate (NMDA) receptor.28,29 Of all opioids, methadone is the most potent NMDA receptor antagonist, being 6 to 18 times more potent than morphine in producing this effect. Antagonism of the NMDA receptor is clinically useful in reducing opioid tolerance and opioid-induced hyperalgesia (OIH) and in chronic pain states leading to pain hypersensitivity.30
Tramadol has both opioidergic and monoaminergic activity at dorsal horn spinal synapses of the nociceptive pathways.31 The analgesic effect of tramadol is due to enhancement of spinal inhibition of 5-hydroxytryptamine (5HT) and norepinephrine reuptake, causing the accumulation of 5HT and norepinephrine in the dorsal spinal horn.
The latest “novel” opioid recently registered worldwide is tapentadol, a potent analgesic with reduced GI and CNS side effects.8,9 Tapentadol has a dual mechanism of action. It is active at the MOR at spinal and supraspinal sites and as a norepinephrine reuptake inhibitor (NRI) in the spinal cord. The combination of these two mechanisms has been designated as the MOR–NRI concept. The affinity of tapentadol for the MOR is 50-fold lower than that of morphine. However, due to synergy between the two mechanisms of action, tapentadol produces potent analgesia and is useful in the treatment of moderate to severe acute and chronic pain. Tapentadol differs from tramadol due to its lack of serotonergic effects resulting in a lower incidence of nausea and vomiting. Tapentadol’s low affinity for the MOR may limit its undesirable side effects although its respiratory side effects have not yet been fully studied.
Finally, non-opioids may also act at opioid receptors. An important example is ketamine, which is an NMDA receptor antagonist with affinity for multiple receptor systems including the opioid receptors.32 Its anesthetic properties are related to its effect at the NMDA receptors while its analgesic effects are predominantly due to MOR activation.
Opioid Mechanisms
Mechanisms of Opioid Analgesia
Whereas nociception is the reception of signals in the CNS that have been triggered by noxious stimulation, pain is the subjective perception of that noxious stimulation. Opioids modify both nociception and the perception of a noxious stimulus (emotional coloring of pain).
Different types of peripheral sensory nociceptors, often free nerve endings, are stimulated by tissue damage and the resulting pain information is transmitted to the spinal cord by two types of small diameter peripheral afferent fibers: Slow conducting, unmyelinated C-fibers (which cause a dull burning pain) and faster, thinly myelinated Aδ fibers (which cause sharp, pricking pain). Both types of primary afferent fibers enter the dorsal horn of the spinal cord and terminate in its superficial layers (lamina I–II). Projection neurons from these laminae give rise to the ascending pathways of the spinothalamic tract. Thalamic nuclei receive the nociceptive inputs and pass the information to key brain pain reception sites such as the periaqueductal gray (PAG), amygdala, and somatosensory cortex. Activation of the MORs extensively located in these higher brain centers stimulates analgesia by activating descending inhibitory pathways from the PAG and rostroventral medulla (RVM) that inhibit nociceptive dorsal horn neuron firing in the spinal cord.33,34 Opioids also exert actions in the cortex and limbic systems affecting cholinergic systems that lead to changes in arousal and pain perception.35
μ-opioid-induced analgesia and descending inhibitory pathways may be activated not only by exogenous opioids, but also by activation of endogenous opioid systems. Direct electrical stimulation of the PAG and RVM induces analgesia that may be reversed by opioid antagonists.36 The electrically stimulated sites overlap with the opioid receptor sites and with opioid-containing interneurons, linking together the actions of exogenously applied analgesic stimuli and endogenous opioid systems. Three major examples of analgesia driven by the endogenous opioid system are (1) stress-induced analgesia37; (2) placebo-induced analgesia38; and (3) conditioning pain modulation (CPM).39
Stress-induced analgesia. The endogenous opioid system is activated under stressful conditions, as demonstrated by the delayed onset of pain by soldiers wounded in battle.40 The same higher brain centers bearing MORs are involved in the implementation of stress-induced analgesia.
 Placebo-induced analgesia. The endogenous opioid system also mediates placebo-induced analgesia, a reduction of pain resulting from an expectation of pain relief. Studies using fMRI and PET show activation of the endogenous opioid systems and MORs in the brains of subjects receiving placebo described as an analgesic.41,42,43 Placebo-induced analgesia may be used to enhance opioid-derived analgesia.
Placebo-induced analgesia. The endogenous opioid system also mediates placebo-induced analgesia, a reduction of pain resulting from an expectation of pain relief. Studies using fMRI and PET show activation of the endogenous opioid systems and MORs in the brains of subjects receiving placebo described as an analgesic.41,42,43 Placebo-induced analgesia may be used to enhance opioid-derived analgesia.
Opioids may also act at spinal sites to induce analgesia. In the superficial laminae of the dorsal horn, local neuronal circuits process both ascending and descending pain pathways and are regulated by local endogenous opioid circuits.
Peripheral Opioid Analgesia
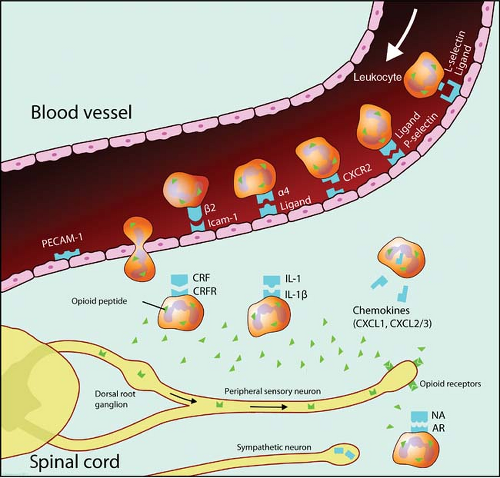
Opioids are also involved in peripheral analgesia by acting directly on sensory neurons (Aδ and C-fibers) to inhibit pain signal transmission. This is especially important in inflammatory pain. However, the immune system is also widely involved in peripheral analgesia.46 Opioid receptors are located not only on neurons, but on immune cells, such as human leukocytes.47 An insult to a peripheral tissue triggers the local release of many proinflammatory mediators that generate an inflammatory cascade, induce spontaneous nociceptor activity, and sensitize sensory neurons to induce spontaneous pain, allodynia (a non-painful stimulus is perceived as painful), and hyperalgesia (increased pain sensitivity). Early in the inflammatory process there is an influx of leukocytes into the inflamed area and these cells are a major source of opioid peptides to inflamed sites. Opioid peptides released locally interact with the opioid neuronal receptors to induce analgesia (Fig. 19-5).48 The inflammatory process also stimulates further opioid receptor upregulation and thereby increases the antinociceptive action of opioid peptides released by immune cells. In aggregate, the inflammatory process not only promotes inflammation and its painful sequelae, but also initiates and sustains a counteracting analgesia driven by endogenous opioids.49
Opioid-induced Hyperalgesia (OIH) and Tolerance
Postoperative patients who have received remifentanil infusions intraoperatively can have a higher incidence of OIH and need greater doses of morphine for control of postoperative pain than patients receiving non-remifentanil–based anesthesia.51 Although animal and human data indicate that all μ-opioids may cause OIH there seems to be a gradual difference in prevalence, with most observation of OIH following remifentanil treatment. This high incidence of OIH following remifentanil infusions may be related to its rapid offset of analgesia. In order to prevent severe pain responses following remifentanil-based anesthesia, administration of morphine (0.1 to 0.25 mg/kg) 45 to 60 minutes before the end of surgery is advisable, and adding a low-dose ketamine infusion may prevent the development of OIH (dose range: 10 to 30 mg/hr) due to ketamine’s NMDA antagonistic properties.52
OIH is not the same phenomenon as opioid tolerance.50 Acute opioid tolerance due to tachyphylaxis requires increasing doses of the opioid to reach a specific analgesic end point during the initial hours of opioid treatment. Chronic tolerance, often seen in opioid abusers, occurs over days and manifests as a decreasing analgesic effect, resulting in dose escalation and increasing the likelihood of OIH. In contrast to OIH, opioid receptor–related and post-activation intracellular processes play an important role in the development of tolerance (including β-arrestin–dependent receptor desensitization and internalization, and G-receptor uncoupling).56,57 Finally, pseudo-tolerance is a phenomenon seen in chronic pain patients due to progression of disease with an increase in the level of nociception often due to destruction of nerves in the tumor region, resulting in neuropathic pain, which is poorly responsive to opioid dose escalation.
Routes of Administration
The most important and predictable route of administration of opioids perioperatively is the intravenous route, since the amount of drug entering the systemic circulation is precisely known. Non-intravenous administration routes (e.g., oral, subcutaneous, transdermal, inhalational, sublingual, oral transmucosal, intranasal, or rectal routes) are often more convenient for the patient although they come at the cost of more variable (and often slower) rates of absorption and bioavailability. Opioids given orally have bioavailabilities of 20% to 40% due to a rapid first-pass effect as a result of opioid metabolism in the liver.
Opioids given via epidural (e.g., patient-controlled epidural analgesia) and intrathecal routes need to diffuse into the surrounding nerve tissue and spinal cord to activate MORs. More lipophilic opioids (fentanyl, sufentanil) will penetrate faster and achieve higher concentrations into the spinal cord than hydrophilic opioids such as morphine and meperidine, yet they are also cleared from the spinal fluid more rapidly.58 Thus the lipophilic opioids may cause an early-onset respiratory depression whereas morphine tends to cause late ventilatory depression due to its slow clearance from the spinal fluid. After the epidural administration of opioids, lipophilic drugs are rapidly absorbed into the systemic circulation resulting in plasma concentrations similar to those observed after low-dose intravenous injections.58 The clinical effects of lipophilic opioids given epidurally are due to systemic, spinal, and supraspinal sites of action. It is important to note that epidurally administered opioids may exacerbate the risk of serious respiratory depression when coadministered with other parenteral opioids.
Intramuscular injections of opioids for treatment of postoperative pain should be avoided as there are superior alternatives such as the intravenous administration of opioids using patient-controlled analgesia (PCA) devices. Compared to IM injections intravenous PCA is associated with lower pain scores and greater patient satisfaction. PCA also does not require frequent painful injections. Under specific and exceptional circumstances, nurse-administered interval IM analgesia is acceptable, such as when the
patient is unable to use the PCA device (mentally or physically incapacitated patients) or in case of fear of PCA by proxy.59 The latter is the case when family members press the PCA button.
patient is unable to use the PCA device (mentally or physically incapacitated patients) or in case of fear of PCA by proxy.59 The latter is the case when family members press the PCA button.
Pharmacokinetics (PK) and Pharmacodynamics (PD)
When injected intravenously opioids are rapidly transported to the heart and pulmonary vessels from where they are dispersed to the various organs and tissues. After a standard dose of opioid, the inter-patient variability of effect is large and related to various factors including weight-related parameters (lean and fat body mass), organ function (hepatic and renal function), and cardiac output. This variability is manifest in the distribution and elimination constants that describe the PK profile of these drugs, which is also related to their physicochemical properties, such as molecule size, pKa (affects the degree of ionization of the molecule and depends on the plasma pH), protein binding (to albumin and α1-acid glycoprotein), and lipid solubility. These factors affect the passage of the drug into the brain across the blood–brain barrier and hence affect both the opioid’s PK and PD characteristics. For example, a small increase in pH seen with respiratory alkalosis will increase the non-ionized form of morphine, fentanyl, sufentanil, and remifentanil, which subsequently crosses the blood–brain barrier. Different drugs may also affect the blood–brain barrier active transport systems that eliminate opioids from the brain. For example, cyclosporine enhances morphine’s analgesic effect but not that of methadone, suggesting that cyclosporine selectively interferes with morphine’s efflux from the brain via specific transporter proteins.
When an opioid is injected into the venous system, there is an initial rapid peak in plasma concentration. Next, the drug rapidly enters multiple organ systems with high blood flow (such as the brain, liver, kidney) from which the plasma drug concentration rapidly drops followed by a slower drop due to redistribution to organs (such as the muscles and later tissues with high fat content) that are less well perfused. These concentration changes over time can be described by non-compartmental and compartmental PK models. Non-compartmental analysis describes the drug’s PK behavior in terms of volume of distribution (VD = drug dose/steady-state plasma drug concentration), rapid and slow distribution half-lives, and elimination half-life (t½elim). A high VD is observed for lipophilic opioids with low protein-binding affinity such as fentanyl (VD = 300 L) but a low VD is observed for remifentanil and alfentanil, due to a high clearance (remifentanil) and/or high protein binding. When VD is small, clearance is responsible for the drop in plasma concentration and consequently the loss of analgesia, whereas redistribution accounts for loss of analgesic effect in drugs with a high VD.
difficult to predict for individual patients. For some side effects such as opioid-induced respiratory depression, the prediction of onset or offset of effect is even more complicated due to counteracting forces, such as the respiratory stimulant effects of increased arterial CO2 and the presence of pain.62
Metabolism: Which Pathways and Metabolites are Clinically Relevant?
Most opioids are metabolized in the liver through either phase I (oxidative and reductive reactions catalyzed by the cytochrome P450 enzyme system) or phase II reactions (conjugation to a specific substrate). Metabolism may occur at other sites as well, such as in the enterocytes of the gastric tract, the kidney, or the brain. Excretion of the parent drug and/or metabolites occurs via the kidney and/or via the biliary tract into the gut where some opioids (morphine, buprenorphine) may undergo reuptake of the compound into the blood stream.
Three aspects of opioid metabolism have clinical importance:
Medications that inhibit or induce the CYP450 system may increase or decrease the clinical effect of opioids by interfering with their metabolism (Table 19-1).63,64
 Opioid metabolites may either be active or inactive, which applies not only to their analgesic effect but also to their unwanted side effects.65,66
Opioid metabolites may either be active or inactive, which applies not only to their analgesic effect but also to their unwanted side effects.65,66
Genetic variability in the CYP system has clinical implications that are discussed in the section on Pharmacogenetics.
Morphine
Morphine undergoes rapid metabolism (by UGT2B7, a phase II reaction) in the liver and within minutes after its administration the two most important hydrophilic metabolites appear in plasma: Morphine-3-glucuronide (M3G) and M6G.64,65,66 M3G is the major metabolite and about 60% of morphine is converted into M3G, while just 5% to 10% is converted to M6G. In humans M3G is without any analgesic or anti-analgesic action. M6G is a full MOR agonist but at the concentrations observed following morphine administration in a patient with normal renal function its contribution to the overall analgesic effect is minimal.67 Due to its low lipophilicity, passage of M6G across the blood–brain barrier is slow and consequently limited. In the hepatocytes both M3G and M6G are transported back into the bloodstream while a small part is transported into the bile ducts.68 In the gut both glucuronides are deglucuronidated and the resultant morphine molecule is partly absorbed by the enterocytes (Fig. 19-7). Enterocytes are able to metabolize morphine and transport the resultant M3G and M6G to the bloodstream (the enterohepatic cycle).
Table 19-1. Inhibitors and Inducers of CYP3A and inhibitors of CYP2D6 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
Since the morphine-glucuronides are excreted via the kidney, patients with renal failure are at risk for M6G-related side effects.67 Since M6G is a full MOR agonist these side effects are typical of opioids and, most importantly, include sedation and respiratory depression. In patients with compromised renal function morphine treatment causes M6G to accumulate in high concentrations that may cause loss of consciousness and severe respiratory depression.67,69 Attempts to market M6G as a potent opioid analgesic have failed, likely due to its slow onset/offset time (t½ke0 4 to 6 hours) and low potency in humans.
Piperidines
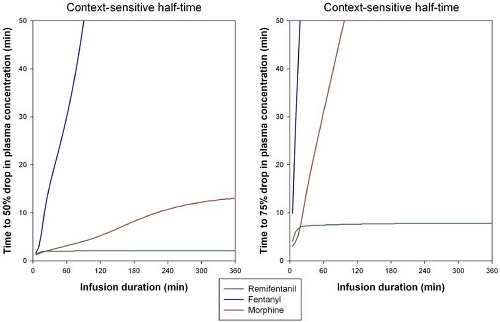
Fentanyl, alfentanil, sufentanil, and remifentanil are lipophilic opioids that rapidly cross the blood–brain barrier. Fentanyl, alfentanil, and sufentanil are metabolized by the liver, catalyzed by the cytochrome P450 enzyme system.64,70,71 Fentanyl has a high hepatic extraction ratio with clearance approaching liver blood flow (1.5 L/min). The major metabolite of fentanyl is the inactive compound norfentanyl. Sufentanil also has a high hepatic extraction ratio with a clearance of 0.9 L/min. Alfentanil is metabolized by CYP3A4 and 3A5 forming the inactive compounds noralfentanil and N-phenylpropionamide. The polymorphic expression of the CYP3A5 gene accounts for the great variability in alfentanil metabolism and clearance.72 Remifentanil contrasts with the other piperidines in that it is not metabolized in the liver.73 Remifentanil contains a methyl ester side chain (Fig. 19-1) that is metabolized by blood (within the erythrocyte) and tissue nonspecific esterases. This causes a rapid clearance of the drug (context sensitive half-life of 2 minutes) making it the most rapidly acting opioid currently available. Clearance of remifentanil is 3 to 5 L/min, which exceeds liver blood flow affirming its extrahepatic clearance. Remifentanil is usually administered as a continuous infusion since its plasma level decreases by 50% in as little as 40 seconds.74,75,76

Full access? Get Clinical Tree