Ophthalmologic
4-1 Corneal Abrasion
Anthony S. Mazzeo
Clinical Presentation
Patients with corneal abrasion (CA) present with eye pain, tearing, foreign body sensation, photophobia, blurry vision, and, occasionally, headache.
Pathophysiology
Any mechanism that disrupts the corneal epithelium may leave a residual defect. Common mechanisms include scratches from fingernails, sports-related eye trauma, dust or debris from a blast, and other accidental instillations of foreign bodies. Contact lens wearers are at risk because of the frequency of ocular instrumentation.
Diagnosis
A complete eye examination with adequate ocular anesthesia is imperative to confirm the diagnosis and evaluate for more serious injury. Visual acuity should be tested and documented. The globe should be inspected with eyelid eversion to evaluate for an existing foreign body. Fluorescein staining of the eye and subsequent cobalt-blue light and slit-lamp inspection will reveal the CA. The dimensions and location of the abrasion should be documented so that follow-up examinations can accurately monitor healing.
Clinical Complications
Complications include superinfection, corneal ulcer (CU) formation, scarring, and recurrence.
Management
Prophylactic topical antibiotics are usually prescribed, with expected healing in 1 to 3 days. Patients at risk for Pseudomonas infection (contact lens wearers) should be given aminoglycoside or quinolone drops and told not to use a contact lens in the affected eye until seen by an ophthalmologist. Oral narcotic analgesia may be necessary. Of note, topical ophthalmic nonsteroidal antiinflammatory drugs (NSAIDs) such as ketorolac 0.5%, diclofenac 0.1%, or indomethacin 0.1% can be used as an alternative or in conjunction with oral medication.1 Patching of the affected eye was done in the past, but the medical literature has documented no clear benefit to patching.2 Similarly, although instillation of cycloplegic/mydriatic agents is routinely practiced for pain relief (especially for larger abrasions), there is no convincing evidence to support the use of this therapy.3 CAs can predispose to tetanus, so a tetanus booster should be considered. All patients with CA should be seen for follow-up within 24 hours to evaluate proper healing and for early detection of complications.
REFERENCES
1. Weaver CS, Terrell KM. Evidence based emergency medicine. Update: do ophthalmic NSAIDs reduce the pain associated with simple corneal abrasion without delaying healing? Ann Emerg Med 2003;41:134-140.
2. Le Sage N, Verreault R, Rochette L. Efficacy of eye patching for traumatic corneal abrasions: a controlled clinical trial. Ann Emerg Med 2001;38:129-134.
3. Carley F, Carley S. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Mydriatics in Corneal Abrasion. Emerg Med J 2001;18273.
4-2 Corneal Laceration
Rachel Haroz
Clinical Presentation
Patients with corneal laceration present with pain, decreased vision, and often other injuries due to the trauma event that caused the corneal injury. The presentation varies based on the severity of the laceration.
Pathophysiology
Corneal lacerations occur more commonly in men younger than 40 years of age. Blunt trauma accounts for about one third of these injuries; in younger patients, 12% are caused by motor vehicle accidents.1 Superficial corneal lacerations include partial-thickness injuries and full-thickness lacerations that are self-healing. Severe lacerations are those with scleral involvement, posterior scleral rupture, intraocular foreign body, or intraocular damage and those lacerations that are extensive or large.2
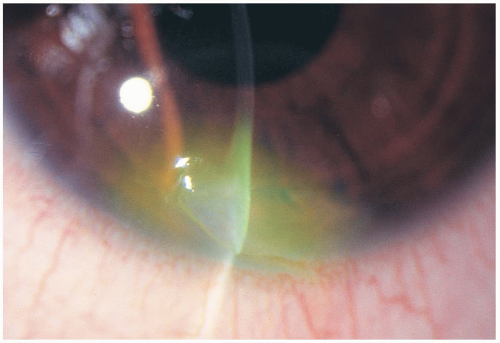
Diagnosis
Superficial lacerations can have minimal to no symptoms and no obvious abnormalities on examination. In severe lacerations, blood in the anterior chamber and decreased anterior chamber depth may be observed. A teardrop-shaped pupil may be present secondary to prolapse of the iris. An abnormally shaped pupil and anterior chamber abnormalities should alert the examiner to a possible corneal laceration or globe rupture. To determine the presence of a laceration, the placement of a fluorescein strip in the corneal region (Seidel test) may be helpful. Aqueous humor leakage turns fluorescent greenblue and can easily be visualized. Other ophthalmologic testing modalities include retroillumination, sclerotic scatter, and indirect illumination. Ocular tonometry is contraindicated in the emergency department for cases of suspected corneal laceration, because of the possible presence of an occult globe rupture.1
Clinical Complications
Complications include visual disability due to astigmatism, infection, and retained foreign bodies.
Management
An ophthalmologist should be consulted for all cases of corneal laceration. Nonsevere (small or partial-thickness) lacerations may be managed with the use of cyanoacrylate tissue adhesive and bandage soft contact lenses.1 Pressure patching may be used. Severe lacerations require surgical intervention. In such cases, a protective rigid eye cover should be secured in place until the surgery is performed. Tetanus immunization should be updated in all cases, and intravenous antibiotics may be necessary for severe lacerations.2 Topical antibiotics and cycloplegics may be sufficient for nonsevere lacerations.2
REFERENCES
1. Hamill MB. Corneal and scleral trauma. Ophthalmol Clin North Am 2002;15:185-194.
2. Hamill MB, Thompson WS. The evaluation and management of corneal lacerations. Retina 1990;10[Suppl 1]:S1-S7.
4-3 Traumatic Iritis
Roger D. Tillotson
Clinical Presentation
Pathophysiology
Blunt trauma to the eye may give rise to structural damage to the iris secondary to a sudden and transient elevation in anterior chamber pressure, which incites a localized inflammatory response.2 This injury may also tear the iris and cause local vascular damage, further increasing inflammation. The iris sphincter constricts in response to the presence of prostaglandins, leading to a miotic pupil.2
Diagnosis
History of trauma to the eye, accompanied by classic clinical findings, implies the diagnosis of traumatic iritis. Fluorescein staining should be used to assess concomitant corneal injury.3 Measurement of intraocular pressure (IOP) enables the physician to exclude the presence of glaucoma and should be performed in all patients with ocular trauma.3 Physical findings may include decreased visual acuity, circumcorneal injection (ciliary flush), and a miotic, sluggish pupil.1,2,3 Slit-lamp examination usually reveals “cells and flare” in the anterior chamber, which may settle into a hypopyon.2
Clinical Complications
Complications include posttraumatic glaucoma and posterior synechiae (fibrous adhesions of the iris to the lens). Severe cases may, on occasion, progress to involve the posterior uvea and retina, with the potential for permanent visual impairment.2
Management
Mild cases may resolve within 1 to 2 weeks with no treatment.2 Cycloplegic eye drops may help to reduce ciliary muscle spasm, reduce synechiae formation, and improve patient comfort. In cases with moderate to severe inflammation, a short course of topical corticosteroids may be considered after consultation with an ophthalmologist.1 In all cases, follow-up with an ophthalmologist should be provided within 24 hours.
REFERENCES
1. Patel H, Goldstein D. Pediatric uveitis. Pediatr Clin North Am 2003;50:125-136.
2. Dalma-Weiszhausz J, Dalma A. The uvea in ocular trauma. Ophthalmol Clin North Am 2002;15:205-213.
3. Liebowitz HM. The red eye. N Engl J Med 2000;343:345-351.
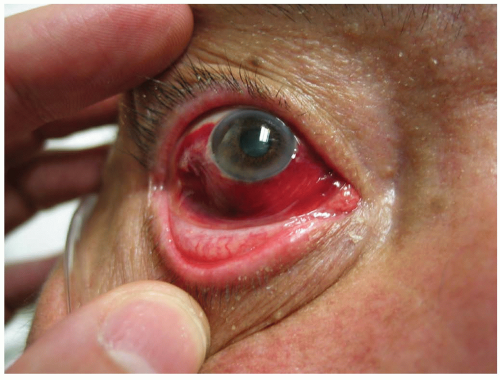
4-4 Ruptured Globe
Michael Horowitz
Clinical Presentation
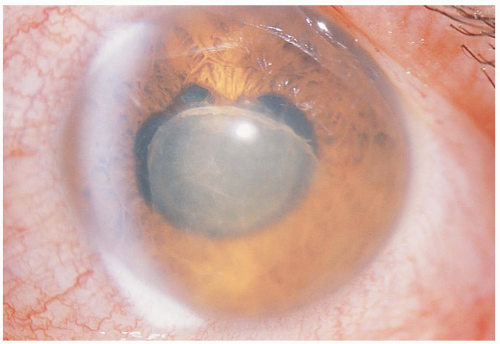
Ruptured globe describes any eye in which the full thickness of either the sclera or the cornea has been disrupted.
Patients present with complaints of eye pain and decreased vision. The rupture is typically secondary to a blunt trauma or a penetrating injury. The affected eye may show chemosis, subconjunctival hemorrhage (SH), visible intraocular contents, decreased anterior chamber depth, decreased intraocular pressure (IOP), and hyphema.
Pathophysiology
In blunt trauma, the scleral rupture is secondary to a sudden increase in IOP; this usually causes rupture in the thinnest portions of the sclera, where the intraocular muscles attach or at the limbus. In patients with prior surgery, the rupture usually occurs at an old surgical site. The full thickness of the cornea or sclera can also be penetrated by a foreign object.1,2
Diagnosis
Ruptured globe should be suspected in any patient with a lid or orbit injury. There may be obvious signs of rupture, such as extrusion of intraocular contents, or the signs may be very subtle, such as a decreased anterior chamber depth or a tented pupil. A modified Seidel test (instillation of fluorescein and observation for streaming) can be used to look for fluid leaks. Decreased IOP is a good indication of ruptured globe, but measurement of IOP should be avoided, because it can worsen the condition. Imaging studies such as computed tomography (CT) for metal objects, magnetic resonance imaging (MRI) for wood or glass, and ultrasonography can be very useful in making the diagnosis.1,2
Clinical Complications
The risk of infectious endophthalmitis is increased if a foreign body is present. Other complications include permanent changes in vision, traumatic cataracts, and various other conditions associated with severe trauma to the eye.
Management
A rigid shield should be kept over the eye at all times. Activities that can increase the IOP (e.g., control emesis, coughing) must be avoided. If the patient needs to be intubated, a nondepolarizing agent should be used first, to avoid the increase in IOP seen with succinylcholine. Systemic antibiotics should be used as prophylaxis for infectious endophthalmitis. Tetanus prophylaxis should be brought up to date, and topical medications should be avoided. The emergency physician should not remove any foreign bodies but should seek early consultation with an ophthalmologist.1,2
REFERENCES
1. Navon SE. Management of the ruptured globe. Int Ophthalmol Clin 1995;35:71-91.
2. Harlan JB Jr, Pieramici DJ. Evaluation of patients with ocular trauma. Ophthalmol Clin North Am 2002;15:153-161.
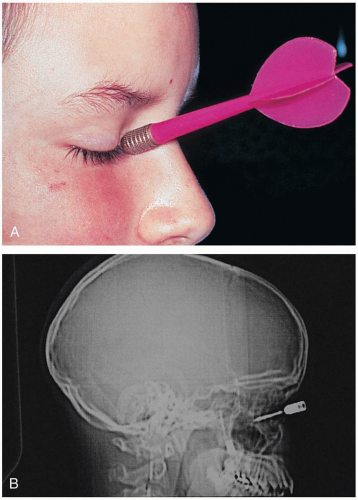
4-5 Penetrating Foreign Body of the Globe
Michael Greenberg
Clinical Presentation
Pathophysiology
PFBG is involved in up to 40% of open globe injuries, with 90% to 100% of cases occurring in men. Most cases of PFBG result from work-related injury; hammering (usually metal on metal) is the source for up to 80% of all cases. Multiple foreign bodies are always a possibility and should be assumed in cases of explosion, ballistic injury, or motor vehicle accident. Most penetrating foreign bodies come to rest in the posterior segment, and more than half lodge in the retina and choroid.3 Injuries involving early signs of endophthalmitis; penetration by objects made of vegetable matter or with copper content; and penetration with possible soil contamination are associated with extraordinarily high risks of permanent visual loss and loss of the globe.3
Diagnosis
PFBG should be assumed in all cases of laceration of the globe. Diagnostic clues include scleral hemorrhage, localized corneal edema, and an obvious rent in the iris. Ultrasonography may be a useful diagnostic adjunct but can give falsely negative results. Plain radiographs are not reliable for the detection of small or nonmetallic foreign bodies. Computed tomography (CT) has a sensitivity of approximately 65%, but many plastic and other foreign bodies may be missed. Magnetic resonance imaging (MRI) is extremely sensitive, but the associated magnetic fields can cause movement of metallic foreign bodies, resulting in secondary damage. Metal detector devices are of virtually no use in diagnosis of PFBG.
Clinical Complications
Management
Emergency on-site ophthalmology consultation is mandatory, because a rapid decision regarding surgical intervention is necessary. It is appropriate to transfer stable patients in order to obtain such consultation in a timely fashion. The benefit of intravenous antibiotics remains unproven, but they should be considered in the discussion with the consulting ophthalmologist. Care must be taken to protect the injured globe from further damage; the use of protective eye shields that do not put pressure on the globe is appropriate.
REFERENCES
1. Harlan JB Jr, Pieramici DJ. Evaluation of patients with ocular trauma. Ophthalmol Clin North Am 2002;15:153-161.
2. Hamill MB. Corneal and scleral trauma. Ophthalmol Clin North Am 2002;15:185-194.
3. Mester V, Kuhn F. Intraocular foreign bodies. Ophthalmol Clin North Am 2002;15:235-242.
4-6 Hordeolum
Michael Greenberg
Clinical Presentation
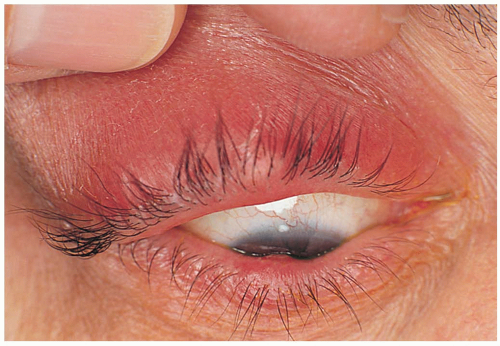
Hordeola, sometimes called “styes,” manifest as acute and focal eyelid abscesses.
Pathophysiology
So-called internal hordeola form by infection of a meibomian gland in the eyelid. External hordeola form by infection of a Zeis gland (hair follicle) in the lid. Most cases are caused by infection with Staphylococcus aureus.1
Diagnosis
The diagnosis is based on clinical recognition.
Clinical Complications
Complications are rare but may include infectious spread to contiguous tissue with the establishment of cellulitis. It is possible for systemic bacteremia to begin from a hordeolum.
Management
Warm, wet compresses applied to the area every 2 to 3 hours help the infection localize.1 Topical antibiotics (e.g., erythromycin) may be added if there is coexistent blepharitis. Systemic antibiotics are rarely needed. Plucking of the eyelashes at the site of a pointing abscess facilitates drainage. Patients should be cautioned against squeezing or puncturing hordeola, because doing so may facilitate the spread of infection. Persistent cases may require incision and drainage.1
REFERENCES
1. Lederman C, Miller M. Hordeola and chalazia. Pediatr Rev 1999;20:283-284.
4-7 Optic Nerve Avulsion
Michael Greenberg
Clinical Presentation
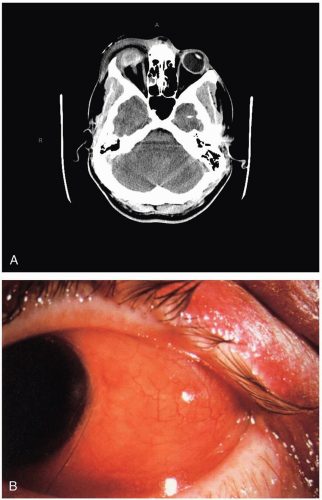
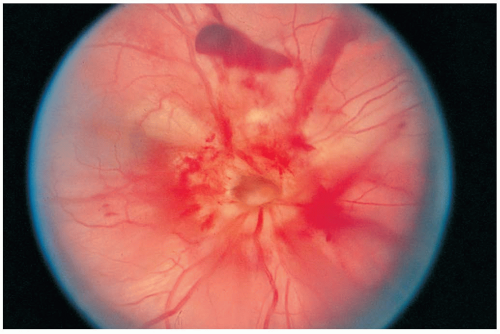
Patients with optic nerve avulsion (ONA) present with acute and complete visual loss coincident with trauma to the orbit.
Pathophysiology
ONA usually occurs after major trauma to the orbit but result from seemingly minor injuries to the globe. Common events associated with ONA include high-speed facial trauma, martial arts injuries, and autoenucleations in psychiatric patients.1 ONA may result from shearing forces that develop when forces applied to the globe cause its rotation; these rotational forces can cause a tearing of the nerve and partial or complete avulsion. In other cases, the globe is forced posteriorly, with a sudden rebound to the anterior position, which can tear the nerve. In most cases, some combination of rotational and retropulsive forces is the most likely mechanism for ONA. In addition, sudden extreme increases in intraocular pressure (IOP) may play a role. ONAs typically occur at one of three anatomic locations: the optic disc, the orbital apex, and the optic chiasm.1 Most ONAs occur at the orbital apex.1
Diagnosis
The clinical ocular examination is often diagnostic for ONA. Indirect ophthalmoscopy may reveal absence of the optic disc. In addition, retinal bleeding is often evident. The diagnosis can be confirmed with advanced imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI), which typically demonstrate avulsion of the nerve. In these cases, the optic nerve sheath usually remains intact. Ocular ultrasonography may be helpful in determining the diagnosis of ONA.
Clinical Complications
Complications include permanent blindness, endocrine abnormalities due to pituitary injury, leaks of cerebrospinal fluid (CSF), meningitis, subarachnoid bleeding, and development of carotid-cavernous fistulae.1
Management
In cases involving the sudden and severe accumulation of orbital blood, emergency decompression by lateral canthotomy may be necessary. Surgical decompression may be helpful in some cases in which optic nerve sheath hematoma is a problem. High-dose corticosteroids may be helpful. There is no effective treatment for ONA at the chiasm, and, in fact, most treatments have not met with good results for ONA at any anatomic location.1,2
REFERENCES
1. Arkin MS, Rubin PA, Bilyk JR, Buchbinder B. Anterior chiasmal optic nerve avulsion. AJNR Am J Neuroradiol 1996;17:1777-1781.
2. Thakar A, Mahapatra AK, Tandon DA. Delayed optic nerve decompression for indirect optic nerve injury. Laryngoscope 2003;113:112-119.
4-8 Corneal/Conjunctival Foreign Body
Michael Greenberg
Clinical Presentation
Patients with corneal/conjunctival foreign body (CCFB) present with eye discomfort and a sensation of foreign material in the eye, excessive tearing, sensitivity to light, and redness. Some patients are able to indicate what the specific foreign material might be.1
Pathophysiology
CCFBs can result from minor or serious trauma. In most cases, foreign material is inadvertently introduced into the eye by rubbing with unclean hands. Some CCFBs are introduced as a result of movement of foreign particles by high-speed equipment. Other CCFBs are simply suspended in the air as particulates and come into contact with the eye randomly.1
Diagnosis
Although the diagnosis is suspected based on the history, confirmation requires a careful physical examination, including triple eversion of the upper lid and eversion of the lower lid. In addition, all patients with suspected CCFBs must be examined with the use of a slit-lamp microscope to identify, locate, and remove the CCFBs.1
Clinical Complications
Complications include corneal abrasions, conjunctivitis, deep ocular infection, retained intraocular foreign body, and permanent corneal damage.
Management
All CCFBs must be removed. Removal technique depends on the location of the CCFB. The slit-lamp microscope vastly facilitates removal by providing adequate magnification and visualization. If the emergency physician is unable to perform this procedure, an ophthalmologist should be consulted for timely CCFB removal. After removal, underlying corneal or conjunctival damage or injury should be evaluated. Cycloplegia and the instillation of topical ophthalmic antibiotics is reasonable in most cases. Patching usually is not needed. All patients should be reevaluated 24 hours after CCFB removal.1
REFERENCES
1. Leibowitz HM. The red eye. N Engl J Med 2000;343:345-351.
4-9 Tarsal Plate Foreign Body
Michael Greenberg
Clinical Presentation
Patients with tarsal plate foreign body (TPFB) invariably present complaining of the sensation of a foreign body in the eye, or of a painful eye with tearing and photophobia, or both. Some complain of a scratching sensation or a feeling that the eye is being abraded every time the upper lid closes over the eye.
Pathophysiology
TPFBs are foreign bodies that have not penetrated the globe and have come to rest beneath the upper eyelid. They may be small particles from virtually any source of airborne particulates or materials inadvertently instilled into the eyes by unclean hands, clothing, or the work or recreational environment. They may be made of metal, wood, glass, plant materials, plastic, or other materials.
Diagnosis
As a result of pain and tearing, patients may be unable to cooperate for an adequate physical examination. On fluorescein staining, multiple superficial vertical corneal abrasions (CAs)provide a clue that a TPFB may be present, and a lid eversion examination should be carried out.
Clinical Complications
Complications include CAs, infection, and foreign body penetration into the cornea, as well as the potential for missed associated ocular injuries (e.g., penetrating foreign bodies). The failure to diagnose an ocular penetrating foreign body has the potential to result in devastating intraocular infection.1
Management
All patients should be treated with a short-acting topical ocular anesthetic to facilitate the examination. Anesthesia is appreciated by the patient and allows the examiner to perform double lid eversion, typically by gently pulling the upper lid out and over a sterile wooden applicator stick, to reveal its underside. Although most TPFBs are visible to the naked eye, it is advisable to perform this examination under slit-lamp microscopy. The TPFB is then easily visualized in almost 100% of cases and can be removed with the moistened cotton tip of another applicator stick. After TPFB removal, fluorescein staining should be performed to check for CAs induced by the TPFB. Superficial CAs may be allowed to heal without treatment, whereas deeper abrasions may benefit from cycloplegia and topical antibiotic drops. Abrasions should be reevaluated in 24 hours to check for adequate healing. At no time should patients be given topical analgesics to go home with, because they may mask the development of serious corneal disease, including destructive infection.
REFERENCES
1. Mester V, Kuhn F. Intraocular foreign bodies. Ophthalmol Clin North Am 2002;15:235-242.
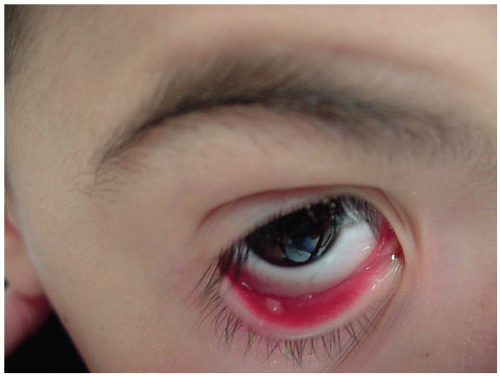
4-10 Subconjunctival Hemorrhage
Michael Greenberg
Clinical Presentation
Patients with subconjunctival hemorrhage (SH) present with painless hemorrhagic areas of varying size in the conjunctiva. Some patients present after ocular trauma and may have pain related to their injury or to other ocular or facial injuries. Often, patients are unaware of the conjunctival bleeding and are alerted to its existence by family members or coworkers.
Pathophysiology
SH is usually spontaneous and in most cases unilateral. SH results when the small vessels bridging the potential space between the conjunctival tissues and episcleral blood vessels tear, as a result of either direct forces applied to the globe or intermittent increased intrathoracic pressure. Other causes include forceful and frequent vomiting (as in bulimia), prolonged extremes of patient positioning (head in dependent position), blunt ocular trauma, forceful and frequent coughing (as may occur in pertussis, influenza, or viral upper respiratory tract infections), heavy exercise, straining at stool, forceful sneezing, Valsalva maneuver, systemic hypertension, ocular amyloidosis, salicylate overuse, idiopathic thrombocytopenic purpura, acute conjunctivitis, and as a complication of gastrointestinal endoscopy.1
Diagnosis
The diagnosis is based on the clinical examination. A complete examination, including a slit-lamp evaluation, should be performed in cases of trauma to the globe, or if penetration of the globe is a possibility.
Clinical Complications
Most SHs resolve spontaneously with no special complications.
Management
Most SHs resolve over a period of 3 to 4 weeks and require no treatment other than reassurance to the patient. However, because SH may represent a manifestation of disease, a complete history and physical examination should be provided, both at the initial presentation and at follow-up. Bilateral involvement should prompt a search for a systemic cause.1
REFERENCES
1. Fukuyama J, Hayasaka S, Yamada K, Setogawa T. Causes of subconjunctival hemorrhage. Ophthalmologica 1990;200:63-67.
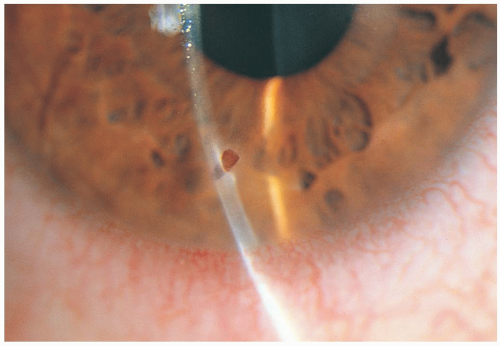
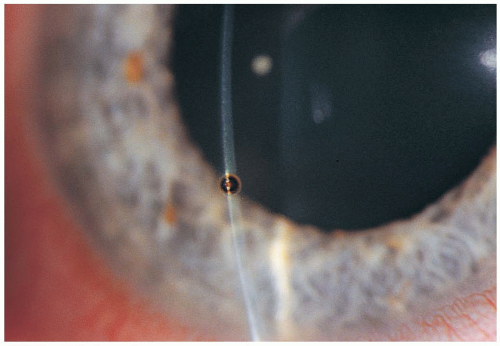
4-11 Corneal Rust Ring
Michael Greenberg
Clinical Presentation
Patients with corneal rust ring (CRR) present with the presence of a metallic foreign body on the surface of the cornea.
Pathophysiology
Iron-containing foreign bodies may oxidize if they remain in contact with the moist microenvironment of the cornea. The portion of the foreign body that is in contact with the cornea rusts and leaves a circular ring of rust embedded in the corneal tissue. The longer the object has been in contact with the cornea, the larger and deeper the rust ring.1
Diagnosis
CRRs are diagnosed by physical examination, usually immediately after the removal of a corneal/conjunctival foreign body (CCFB). At times, a CRR is easily visible to the naked eye. However, a slit-lamp examination is in order for patients who may have residual CRRs after foreign body removal.
Clinical Complications
Untreated CRR may predispose to deep ocular infection, as well as conjunctivitis and ocular irritation. CRRs that remain in the cornea may retard healing of the corneal defect left by the removal of the associated foreign body.1
Management
CRRs should be removed as soon as they are diagnosed. Frequently, they can be removed by the emergency physician with the use of a slit-lamp microscope and a bur or small-gauge needle with appropriate topical anesthesia. It is essential to remove the majority of the rust ring, but it is not necessary to remove 100% of it. Difficult cases and those in which the majority of the CRR cannot easily be removed should be referred to an ophthalmologist as soon as possible. After removal of the CRR, some authorities recommend application of topical antibiotics and daily reevaluation until the corneal defect has healed.1
REFERENCES
1. Newell SW. Management of corneal foreign bodies. Am Fam Physician 1985;31:149-156.
4-12 Chalazion
Michael Greenberg
Clinical Presentation
Chalazia present as a swollen, minimally tender mass at the eyelid margin or within the body of the lid itself.1
Pathophysiology
Chalazia are lipid-containing granulomatous masses that represent foreign body reactions surrounding a meibomian gland. These are essentially reactions to lipid produced by the gland. The inflammatory exudates contain histiocytes, multinucleated giant cells, plasma cells, eosinophils, lymphocytes, and polymorphonuclear leukocytes.1
Diagnosis
Chalazia are diagnosed based on clinical recognition.
Clinical Complications
Complications include the potential for superinfection if the chalazion is manipulated by the patient or other nonmedical personnel. The most common complication of chalazia is recurrence.
Management
Some chalazia resolve without treatment. Most authors recommend frequent application of warm, moist compresses, which serve to facilitate drainage of the chalazion.1 If blepharitis coexists, topical antibiotics may be helpful. If the problem does not resolve after 1 month of conservative therapy, the patient should be referred to an ophthalmologist for incision and curettage. Some ophthalmologists advocate the administration of intralesional steroids by injection. Recurrent chalazia may require the use of oral antibiotics.1
REFERENCES
1. Lederman C, Miller M. Hordeola and chalazia. Pediatr Rev 1999;20:283-284.
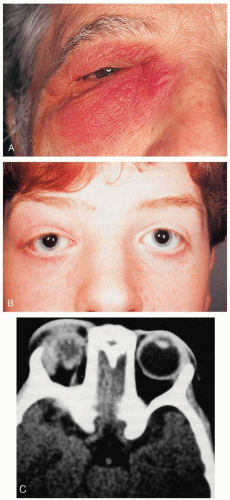
4-13 Dacryoadenitis/Dacryocystitis
Michael Greenberg
Clinical Presentation
Pathophysiology
Dacryocystitis can be acute or chronic. In cases of acute dacryocystitis, there is acute blockage of the nasolacrimal duct as a result of inflammation, swelling, and debris accumulation in that duct.1,2 Secondary infection results in acute dacryocystitis as a preseptal infection that may be of viral, bacterial, or fungal origin. Most cases of bacterial origin involve staphylococcal organisms.1,2 Prior dacryocystitis is a substantial risk factor for the development of orbital extension.2
Diagnosis
The diagnosis is based on clinical examination and history. Orbital computed tomography (CT) may confirm the diagnosis and rule in or out various clinical complications, including abscess formation and malignancy.
Clinical Complications
Management
Patients who appear to be systemically ill or are febrile, diabetic, immunocompromised, suffering a reoccurrence of dacryocystitis, homeless, or noncompliant should be admitted to the hospital for local care and administration of intravenous antibiotics.1,2 Other patients may be treated as outpatients with hourly warm compresses, oral antibiotics, and follow-up with an ophthalmologist within 24 hours. Despite therapy, most patients require surgical intervention for drainage procedures.
REFERENCES
1. Ataullah S, Sloan B. Acute dacryocystitis presenting as an orbital abscess. Clin Exp Ophthalmol 2002;30:44-46.
2. Kikkawa DO, Heinz GW, Martin RT, Nunery WN, Eiseman AS. Orbital cellulitis and abscess secondary to dacryocystitis. Arch Ophthalmol 2002;120:1096-1099.
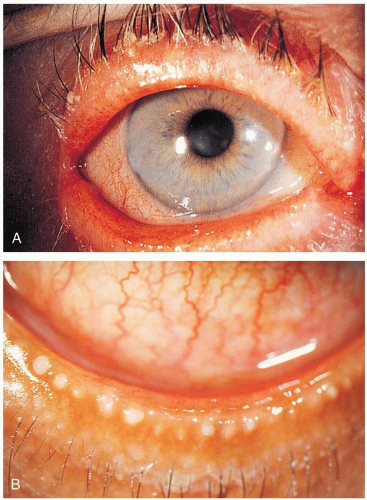
4-14 Blepharitis
Michael Greenberg
Clinical Presentation
Patients with blepharitis present with acute or chronic inflammatory changes of the eyelids, often accompanied by ocular foreign body sensation, light sensitivity, redness and swelling of the eyelids, loss of eyelashes, and conjunctival redness.1
Pathophysiology
Blepharitis usually arises from local staphylococcal infection; however, seborrhea, acne rosacea, and Demodex folliculorum infection may also be causative. Seborrheic blepharitis is similar but less severe than staphylococcal blepharitis. Seborrheic blepharitis involves dysfunction of the glands of Zeis; it occurs in patients who already have seborrheic dermatitis. Dysfunction of the meibomian glands is characterized by excess lipid secretion. Staphylococcal infection occurs at the base of the lashes and results in chronic irritation, itching, soreness, photophobia, and tearing. Dry, scaly concretions called collarettes build up at the base of the lashes. Hypersensitivity to staphylococcal exotoxins may cause inflammation of the conjunctiva. Seborrhea can be oily or dry, and it is thought that the excessive amounts of neutral lipids produced in this condition are broken down into irritating fatty acids by Corynebacterium acnes. In some cases, it is possible to see globules of oil on the posterior lid margin.
Diagnosis
The diagnosis is based on physical examination. Slit-lamp examination is essential to identify inverted lashes, corneal inflammation, and associated foreign material. Blepharitis symptoms tend to be worse in the morning.
Management
Frequent lid cleansing is essential and is directed at removal of debris and secretions from the lid margins. This can be accomplished with the use of a clean cloth and a dilute solution of baby shampoo. Lid cleansing should be done twice daily until the symptoms are under control, and the patient should be cautioned that this may take months. If staphylococcal infection is suspected, topical antibiotic ointment should be applied to the eyelids and lid margins. In severe cases, topical steroids may be helpful, but they should be used in consultation with an ophthalmologist, because prolonged ocular exposure to steroids increases the risk of iatrogenic glaucoma and cataract induction. Artificial tears may be helpful in alleviating ocular irritation from inflamed lid margins. All cases not responding to basic therapy should be referred to the care of an ophthalmologist.1,2
REFERENCES
1. Leibowitz HM. The red eye. N Engl J Med 2000;343:345-351.
2. McCulley JP, Shine WE. Changing concepts in the diagnosis and management of blepharitis. Cornea 2000;19:650-658.
4-15 Gonococcal Conjunctivitis
Benjamin Roemer
Clinical Presentation
Patients with this hyperacute conjunctivitis present with purulent discharge, erythema, and irritation of the eye. Additional complaints may include foreign body sensation, eyelids “stuck together,” and genital symptoms.1
Pathophysiology
Gonococcal conjunctivitis is caused by Neisseria gonorrhoeae via direct inoculation of the organism into the eye. This conjunctivitis is seen in two patient populations: sexually active adults and neonates. Hand-eye inoculation occurs most commonly in the adult. Neonatal inoculation occurs via direct contact during passage through an infected birth canal. Neonatal infection usually manifests within the first 48 hours of life.
The conjunctiva is a thin, translucent layer composed of nonkeratinizing squamous epithelium and the substantia propria. Much of the inflammatory reaction to gonococcus occurs due to the activity of lymphocytes, plasma cells, macrophages, and mast cells in the substantia propria. The incidence of gonococcal ophthalmia neonatorum is 3 per 1,000 live births in the United States, and it is higher in countries without routine silver nitrate prophylaxis.2 The exact incidence in adults is not known. Gonococcal conjunctivitis appears to be more prevalent among the urban poor.
Diagnosis
Diagnosis is made by clinical examination, Gram staining for intracellular gram-negative diplococci, and culture of conjunctival discharge.2 The clinical presentation includes severe purulent discharge, punctate keratitis, chemosis, and conjunctival papillae. Membrane formation, subconjunctival hemorrhage (SH), and preauricular lymph nodes usually are present. Corneal infiltrates and ulceration occur in severe cases.3
Clinical Complications
Complications include permanent partial or total blindness and disseminated disease.
Management
Treatment consists of administration of topical chloramphenicol eye drops and intramuscular benzylpenicillin or a cephalosporin. Prophylactic treatment is required for neonates born to mothers with known gonorrhea within the first hour of life.
REFERENCES
1. Greenberg MF, Pollard ZF. The red eye in childhood. Pediatr Clin North Am 2003;50:105-124.
2. Rapoza PA, Quinn TC, Kiessling LA, Taylor HR. Epidemiology of neonatal conjunctivitis. Ophthalmology 1986;93:456-461.
3. Wan WL, Farkas GC, May WN, Robin JB. The clinical characteristics and course of adult gonococcal conjunctivitis. Am j Ophthalmol 1986;102:575-583.
4-16 Bacterial Conjunctivitis
Nick Gorton
Clinical Presentation
Patients with bacterial conjunctivitis (BC) present with a painful, red eye and mucopurulent discharge. Severe discharge and a hyperacute presentation suggest neisserial disease. A subacute presentation with concomitant genital symptoms suggests chlamydial disease. Infections are unilateral initially but spreads to the contralateral eye in up to 80% of cases. Patients may complain of a foreign body sensation. Mild pruritus may be present, but if it is a prominent symptom, allergic conjunctivitis should be suspected.1,2,3
Pathophysiology
Pathogenic bacteria overwhelm conjunctival defenses, resulting in inflammation followed by purulent infection. Hyperacute and hyperpurulent disease is generally N. gonorrhoeae or Neisseria meningitidis, although staphylococcal and streptococcal species may also be present. Chronic infections are frequently secondary to repeated bacterial contamination of the conjunctiva from blepharitis or dacryocystitis. Three fourths of acute childhood conjunctival infections are bacterial, with Haemophilus influenzae comprising the majority. Streptococcus pneumoniae, S. aureus, and Moraxella catarrhalis are also common. Only half of acute adult conjunctival infections are bacterial in nature, with S. aureus being the most common cause, followed by pneumococcus, H. influenzae, and Moraxella species.1
Diagnosis
It is impossible to clinically differentiate between bacterial and viral conjunctivitis. In patients who are debilitated, if severe discharge is present, or if clinical suspicion exists for sexually transmitted diseases, samples should be collected for culture. Physical examination with and without fluorescein staining is recommended. In simple conjunctivitis, the corneal epithelium is intact and no corneal ulcers are revealed with fluorescein stain. Cell and flare in the anterior chamber suggests uveitis.1,2,3
Clinical Complications
Most BC is self-limited even without treatment, and ocular complications are rare. However, complications of concomitant systemic infections can be significant. In addition to the sequelae of untreated genital infections, N. meningitidis conjunctivitis is accompanied by meningitis in 18% of cases, and H. influenzae conjunctivitis is complicated by otitis media in 25% of children.3
Management
Uncomplicated cases are self-limited, but topical antibiotics shorten the average duration of clinical disease.3 Prompt referral to an ophthalmologist is advisable. Adults with suspected gonococcal disease should have a follow-up visit with an ophthalmologist within 24 hours. Children with suspected gonococcal disease must be admitted for intravenous antibiotic therapy. Other patients should be rechecked within 2 days.1
REFERENCES
1. Diamant JI, Hwang DG. Therapy for bacterial conjunctivitis. Ophthalmol Clin North Am 1999;12:15-20.
2. Chung C, Cohen E, Smith J. Bacterial conjunctivitis. Clin Evid 2002;(7):574-579.
3. Sheikh A, Hurwitz B, Cave J. Antibiotics for acute bacterial conjunctivitis. Cochrane Database Syst Rev 2000;(2):CD001211.
4-17 Viral Conjunctivitis
Roger D. Tillotson
Clinical Presentation
Patients with viral conjunctivitis (VC) may present with only ocular symptoms or with a concomitant upper respiratory tract infection.1,2 VC usually begins unilaterally, but contralateral involvement often develops after the patient touches the disease-free eye without washing.1,2 These patients classically complain of conjunctival injection, discharge, and pruritus. Transient blurry vision may occur because of the ocular discharge, but persistent blurry vision should prompt consideration of an alternative diagnosis.2 On physical examination, scleral injection, epiphora, chemosis, subconjunctival hemorrhage (SH), and eyelid erythema and edema may all be present. Preauricular adenopathy is also common, but it is a nonspecific finding.2
Pathophysiology
All age groups are susceptible to viral conjunctivitis.1 Because of the highly contagious nature of this disease, the patient may report recent exposure to another individual with similar symptoms. Adenovirus is the most common cause, but a variety of other viruses, such as herpes simplex virus (HSV), enterovirus, coxsackievirus, poxvirus, and human immunodeficiency virus (HIV) can all cause viral conjunctivitis.1 Viral transmission is through direct contact or via fomites.
Diagnosis
Clinical Complications
Complications include superinfection with bacteria, ulcer formation, and other consequences of bacterial conjunctivitis (BC).
Management
REFERENCES
1. Greenberg MF, Pollard ZF. The red eye in childhood. Pediatr Clin North Am 2003;50:105-124.
2. Liebowitz HM. The red eye. N Engl J Med 2000;343:345-351.
4-18 Herpes Simplex Keratitis
Roger D. Tillotson
Clinical Presentation
Herpes simplex keratitis (HSK) can occur in the context of primary infection by herpes simplex virus (HSV); however, it is observed more frequently in secondary or recurrent disease.1 Patients present with a painful, red eye accompanied by tearing, blurred vision, and photophobia. The patient may reveal a history of prior episodes of HSK, because approximately 25% of patients with prior episodes of HSK experience a recurrence within 1 to 2 years.1
Pathophysiology
HSV is a DNA virus with worldwide distribution.2 HSK is among a spectrum of eye diseases caused by HSV; blepharitis, conjunctivitis, and retinitis are also well documented.1,2 HSK may be classified into four main forms: infectious epithelial keratitis, neurotrophic keratopathy, stromal keratitis, and endotheliitis.3 Infectious epithelial keratitis is the most common form; it results from viral replication in the corneal epithelium with subsequent cell lysis. Stromal keratitis and endotheliitis result from a combination of infectious and immune-mediated effects.3

Full access? Get Clinical Tree