Ophthalmic, Ear, Nose, and Throat Surgery
Thoha Pham
1. The most accurate statement regarding absorption of topically administered ophthalmic drugs is that they are absorbed
A. Slower than subcutaneous absorption
B. Faster that intravenous absorption
C. Similar to oral absorption
D. Slower than intravenous absorption
2. Drainage of aqueous humor occurs at all of these sites, except
A. Canal of Schlemm
B. Trabecular network
C. Episcleral venous system
D. Tear ducts
3. The normal intraocular pressure (IOP) is _______ (mm Hg):
A. 5
B. 10
C. 25
D. 30
4. Correct consequence of respiratory variables on intraocular pressure (IOP) is
A. Decrease in PaO2 will decrease IOP
B. Increase in PaO2 will decrease IOP
C. Decrease in PaCO2 will increase IOP
D. Increase in PaCO2 will increase IOP
5. All of the following will serve to decrease intraocular pressure (IOP), except
A. Nitrous oxide
B. Acidosis
C. Morphine
D. Vecuronium
6. Increases in intraocular pressure (IOP) following succinylcholine administration for tracheal intubation can be minimized by all of the following, except
A. β-Adrenergic blocker
B. Nondepolarizing relaxant
C. Detachment of extraocular muscles from the globe
D. Lidocaine
7. The ocular effects of ketamine includes
A. Pupillary constriction
B. Blepharospasm
C. Decrease in intraocular pressure
D. Myoclonus
8. An 82-year-old female patient who resides in a nursing home facility presents for breast biopsy. She states that she uses eye drops to treat glaucoma, but does not know exact names. Patient denies other medical issues, however states that she frequently has acid reflux. Potential anesthetic considerations as a result of eye drops include all of the following, except
A. Hyperchloremic metabolic acidosis
B. Hypokalemic metabolic acidosis
C. Prolonged neuromuscular block with succinylcholine
D. Atropine-resistant bradycardia
9. An air bubble is injected into the posterior chamber at the conclusion of retinal surgery (pneumatic retinopexy) to facilitate anatomically correct healing. The most appropriate anesthetic management, before the air bubble is injected, is
A. Increase depth of anesthesia
B. Discontinue nitrous oxide (N2O)
C. Ensure adequate muscle relaxation
D. Hyperventilate the patient
10. Compared with air, sulfur hexafluoride (SF6) bubble injected following vitreous surgery
A. Has a longer duration of action
B. Is more soluble in blood than nitrogen
C. Is inert and will not expand
D. Is contraindicated in outpatient surgery
Questions 11 to 14
A 22-month-old 14.5-kg “preemie” is undergoing strabismus repair under general endotracheal anesthetic (GETA). Following an uneventful inhaled induction with sevoflurane, peripheral IV was obtained, and by oversight, patient was given 20 mg of succinylcholine prior to intubation. Masseter spasm was noted moments later.
11. What parameter is considered the earliest sign and symptom of an ensuing hypermetabolic state following succinylcholine administration?
A. Hyperthermia
B. Hypotension
C. EtCO2 increase
D. Low oxygen saturation
12. Midway through the surgery, when surgical traction in the operative field is applied, patient’s heart rate plummets from 110 bpm down to 55 bpm. The pairing that accurately reflects the afferent and efferent limbs, respectively, of this reflex is
A. Trigeminal nerve vagus nerve
B. Optic nerve vagus nerve
C. Vagus nerve trigeminal nerve
D. Trochlear Nerve optic nerve
13. The most appropriate first step in the management of this hemodynamic instability is
A. Epinephrine
B. Atropine
C. Remove traction
D. Phenylephrine
14. At the conclusion of the surgery, postoperative nausea and vomiting should be anticipated and can be minimized by all of the following, except
A. Serotonin (5-HT3) antagonist
B. Propofol infusion
C. Limiting opioids
D. Deep extubation
15. The true statement regarding an oculocardiac reflex is
A. It does not occur in enucleated patients
B. Incidence is increased in the setting of hypercarbia
C. Intensity increases with repeated stimulation
D. Suppressed by general anesthesia
16. All of the following anatomic structures may participate in triggering an acute and abrupt bradycardia during ophthalmic surgery, except
A. Trigeminal nerve
B. Vagus nerve
C. Globe
D. Optic nerve
17. Appropriate anesthetic management for ophthalmic surgery requires tight control of intraocular pressure (IOP) before, during, and after the procedure. The accurate effect of an anesthetic drug or maneuver on IOP is
A. Decreased by glycopyrrolate
B. Increased by hyperventilation
C. Decreased by nitrous oxide
D. Increased by nondepolarizing muscle relaxants
18. All these nerves can be disrupted by injection of local anesthetics into the retrobulbar space, except
A. Optic nerve
B. Oculomotor nerve
C. Trochlear nerve
D. Abducens nerve
19. The eye movement that is preserved, or unaffected, following a retrobulbar block with 0.5% bupivacaine is
A. Abduction
B. Rotation
C. Adduction
D. Elevation
20. Possible complications of a retrobulbar block include all the following, except
A. Central retinal artery occlusion
B. Oculocardiac reflex
C. Puncture of the globe
D. Horner syndrome
A patient is given propofol 20 mg intravenously just before placement of a retrobulbar block (0.5% bupivacaine—3 mL) to provide ocular akinesia for ocular surgery.
21. As the surgeon attempts to place a lid speculum, the patient squints, preventing adequate placement. Additional blockade of which muscle can provide additional akinesia?
A. Orbicularis oculi
B. Temporalis
C. Zygomaticus minor
D. Levator anguli oris
22. Moments later, apnea occurs followed by complete loss of consciousness. The most likely etiology to explain this event is
A. Subarachnoid injection of local anesthetic
B. Effects of propofol
C. Oculocardiac reflex
D. Intravenous injection of local anesthetic
Questions 23 to 27
A 57-year-old otherwise-healthy male was leaving a dinner party when he was involved in a rollover car accident during which a foreign object became lodged into his right eye. He is taken to the OR for emergent surgical repair of a penetrating wound to his right globe.
23. The most appropriate anesthetic plan to consider is
A. Retrobulbar block followed by monitored anesthesia care (MAC)
B. IV induction of general anesthesia avoiding muscle relaxants
C. Rapid-sequence induction of anesthesia using large dose rocuronium
D. Secure the airway with an awake fiberoptic intubation
24. Anesthetic strategies that can minimize intraocular pressure (IOP) increase and lessen his risk of ocular extrusion include all of the following, except
A. Ketamine
B. Hyperventilation
C. Inhaled volatile agent, 2.0 MAC
D. Controlled hypotension
25. Fifteen minutes after the start of surgery, while the surgeon is retracting the medial rectus muscle, the patient becomes hypotensive and bradycardic. The first-line therapy to address this cardiovascular derangement is
A. Atropine 1 mg IV
B. Phenylephrine 100 μg IV
C. Ask the surgeon to stop
D. Glycopyrrolate 1 mg IV
26. The patient’s vital signs normalize and anesthesia is maintained with desflurane and nitrous oxide. Later in the case, conjunctival instillation of a phenylephrine (10%) solution results in immediate escalation of blood pressure from 105/70 to 220/115 mm Hg, while his pulse falls from 86 to 35 bpm. The ECG reveals new onset of ectopic ventricular complexes. The most appropriate treatment option at this time is
A. Ask the surgeon to stop
B. Administer nitroprusside
C. Administer atropine
D. Discontinue nitrous oxide
27. At the conclusion of the surgery, patient is extubated and brought to the recovery room (PACU) in a stable condition. Thirty minutes later, when he is more awake, he notes unilateral eye discomfort in the nonsurgical eye. He has associated tearing, conjunctivitis, photophobia, and pain, which is worsened with blinking. These eye symptoms are most likely caused by
A. Retinal hemorrhage
B. Oculogyric crisis
C. Angle-closure glaucoma
D. Corneal abrasion
28. True statement regarding laryngospasm is
A. Associated risk of pulmonary edema
B. The false vocal cords do not spasm
C. Mediated through the recurrent laryngeal nerve
D. Increased risk of aspiration
29. A patient in the intensive care unit (ICU) with pulmonary failure requires tracheal intubation. Compared with nasotracheal intubation, oral tracheal intubation carries a higher incidence of
A. Patient discomfort
B. Maxillary sinusitis
C. Transient bacteremia
D. Otitis media
30. When compared to an adult, the airway anatomy of a 6-week-old infant reveals
A. Tongue is smaller and floppy
B. Airway is narrowest at the glottic opening
C. Position of the larynx is more anterior in the neck
D. Epiglottis is flat and firm
Questions 31 to 32
A 3-year-old patient arrives for rescheduled tonsillectomy and adenoidectomy with another acute upper respiratory tract infection (URI). Her initial surgery was postponed 3 weeks ago as she had a URI at that time as well. Exam reveals a runny nose with greenish-yellow discharge with an intermittant wet cough. She is afebrile with normal vital signs.
31. Postponement of surgery will reduce the risk of
A. Laryngospasm
B. Hemorrhage
C. Difficult intubation
D. Gastroesophageal reflux
32. Surgery proceeded without incident; however, 2 hours later in the recovery room (PACU), she vomits a large blood clot followed by ongoing bleeding. She appears pale and anxious. Vitals reveal heart rate = 130 bpm, respiratory rate = 25 bpm, and blood pressure = 77/35 mm Hg. Her capillary refill time is 4 seconds. The most appropriate next step in management at this time is
A. Insertion of orogastric tube to empty the stomach of blood
B. Emergent return to the operating room
C. Administer anxiolysis medication
D. Provide liberal fluid resuscitation
A 65-year-old male requires transoral laser microsurgery to address his laryngeal webs. His medical history reveals remote tobacco smoking and recreational drug use in college.
33. Minimizing airway fire hazards associated with laser surgery can be accomplished by use of all of the following, except
A. Intermittent mode laser emissions
B. An air/oxygen anesthetic technique
C. A polyvinylchloride (PVC) endotracheal tube
D. Saline-soaked sponges over exposed tissues
34. Ten minutes later, the surgeon yells “FIRE!” The most appropriate next step is to
A. Ventilate with air
B. Increase Fio2 to 1.0
C. Instill saline down the endotracheal tube lumen
D. Remove the endotracheal tube
35. One hour later while recovering in the PACU, the patient is noted to have stridor and difficulty breathing. At this time, the most appropriate next step in his airway management includes
A. Administration of aerosolized epinephrine
B. Endotracheal intubation
C. Administration of helium and oxygen
D. Intravenous injection of dexamethasone
36. A 10-year-old girl with hoarseness presents for laser microsurgery to address laryngeal papillomas. She is otherwise healthy. The surgeon is requesting a general endotracheal anesthetic (GETA). The gas mixture least likely to support combustion is
A. Oxygen 35%, air 65%
B. Oxygen 30%, helium 70%
C. Oxygen 20%, nitrous oxide (N2O) 80%
D. Oxygen 30%, nitrogen (N2) 70%
37. A 55-year-old woman with a 35 pack-year history of tobacco smoking is undergoing laryngobronchoscopy utilizing the Sanders jet ventilation technique. The principle behind apneic oxygenation is
A. Contrasting density of inhaled gases
B. Maintenance of spontaneous ventilation
C. Air entrainment
D. Use of helium–oxygen mixtures
38. During apneic oxygenation via a rigid bronchoscope, anesthetic considerations include all of the following, except
A. Duration of the procedure is limited by the increase in carbon dioxide
B. Denitrogenation should be performed prior to apnea
C. PaCO2 remains unchanged for the first 15 minutes
D. Functional residual capacity and body weight influence the rate of desaturation
Questions 39 to 43
A 35-year-old male with a toxic multinodular goiter presents for thyroidectomy with radical neck dissection. He denies any other significant medical history. Review of systems reveals orthopnea and dysphagia with a recent change in the caliber of his voice.
39. True statements about this patient include all of the following, except
A. A flow–volume loop on spirometry can evaluate tracheal compression
B. The airway may obstruct with sedation
C. The trachea may collapse postoperatively
D. An abnormally low forced expiratory volume in 1 second (FEV1) would be diagnostic of an upper airway obstruction
40. To attenuate risk of a “cannot ventilate, cannot intubate” scenario, an awake airway intubation is discussed. The neural structure that does not need to be blocked in order to provide adequate airway analgesia for a nasal intubation is
A. Hypoglossal nerve
B. Sphenopalatine ganglion
C. Superior laryngeal nerve
D. Recurrent laryngeal nerve
41. At the conclusion of a complicated 4-hour resection, the patient is extubated and brought to the recovery room. One hour after extubation, the patient complains of dyspnea with stridorous respiration. Initial steps include all of the following, except
A. Intravenous administration of calcium
B. Nebulized racemic epinephrine
C. Inspection of the surgical site
D. Direct laryngoscopy
42. If bilateral recurrent laryngeal nerves were unintentionally severed, the likely finding on direct laryngoscopy would be
A. Paralysis of the cricothyroid muscles
B. Intermediate position of the cords
C. Midline, closed position of the cords
D. Pure adductor vocal cord paralysis
43. Instead, postoperative direct laryngoscopy reveals normal position of the cords at rest, widely open glottic opening at maximal inspiration, and symmetrically moving cords during quiet breathing but with weak phonation and inability to speak loudly or shout. The most likely etiology is
A. Recurrent laryngeal nerve paralysis
B. Superior laryngeal nerve (SLN) paralysis
C. External airway compression
D. Vagus nerve paralysis
Questions 44 to 45
A 27-year-old male arrives to the operating room with laryngotracheal injuries stemming from a motorcycle collision. He presents with hoarseness and dyspnea while sitting, but is unable to lie flat due to worsening dyspnea. He is unable to swallow, and is drooling/spitting moderately blood-stained sputum. His anterior neck is diffusely swollen and exquisitely tender with notable subcutaneous emphysema. Oxygen saturation is 100% with supplemental oxygen via face mask. Review of imaging reveals a thyroid cartilage fracture horizontally and crossing the midline.
44. The most appropriate approach to his airway management is
A. Tracheostomy
B. Laryngeal mask airway
C. Nasotracheal intubation
D. Cricothyroidotomy
45. His injury would be consistent with trauma to this zone of his neck:
A. Zone I
B. Zone II
C. Zone III
D. Zone IV
Questions 46 to 47
During thyroidectomy for carcinoma, a 22-year-old patient develops tachycardia to 115 bpm while blood pressure intensifies to 145/100 mm Hg. The inhaled anesthetic is deepened and minute ventilation is increased. Thirty minutes later, tachycardia and hypertension persists despite all efforts (Table 16-1).
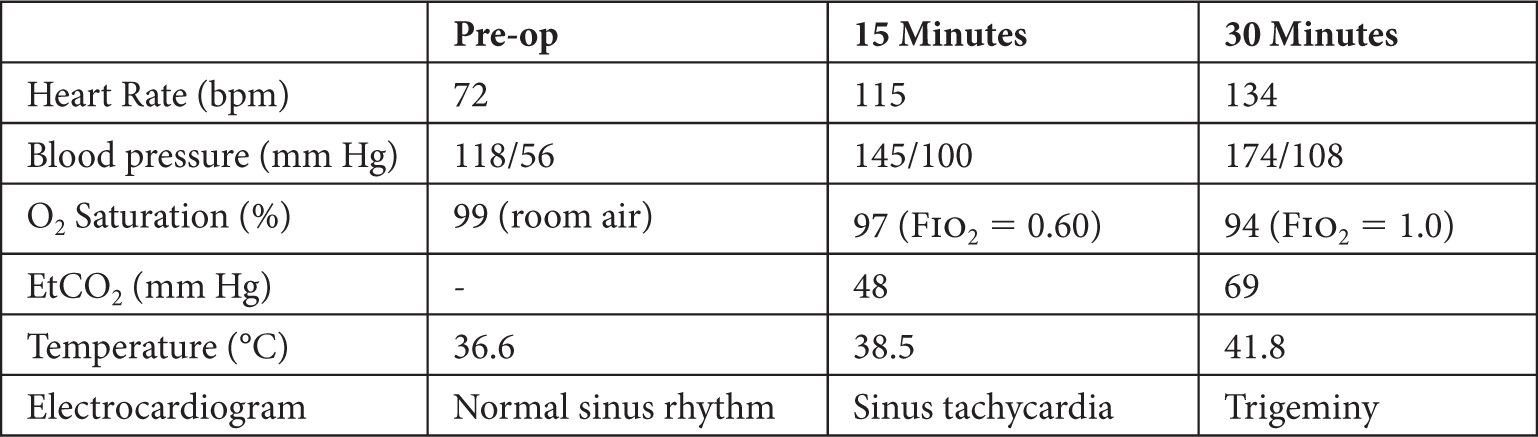
46. The appropriate treatment to consider at this time is
A. Propranolol
B. Acetaminophen
C. Iodine
D. Dantrolene
47. Diagnosis of malignant hyperthermia is most commonly confirmed by
A. Caffeine halothane contracture test (CHCT)
B. Urinalysis
C. Arterial blood gas
D. Core temperature >42°C

Full access? Get Clinical Tree






