CHAPTER 73
Occupational Lung Disease
Michele McDermott, DNP, RN, FNP-BC
Primary care providers are in a key position to prevent, identify, and treat occupational illness. First, providers can identify persons at risk of occupational illness because of exposure to a known occupational hazard. Second, primary care providers who care for a multitude of undifferentiated illnesses are also in a position to link an illness and occupational exposure.
The types of occupational pulmonary disorders are listed in Table 73.1. Two of these diseases, occupational asthma and asbestosis, can be adequately diagnosed and treated only if the primary care provider suspects occupational pulmonary disease and elicits a history of a significant workplace exposure.
Occupational asthma is a relatively common medical condition, but the diagnosis could easily be missed if a link is not established between symptoms and the workplace. Asbestosis, an interstitial disease related to asbestos exposure, becomes symptomatic only after a long latency period. An exposure history and knowledge of the early signs and symptoms are essential to diagnose this disease.
The true incidence and prevalence of occupational illness and injury are not known; however, it is estimated that 11 million workers in a variety of industries and occupations are exposed to at least one of the numerous agents known to be associated with occupational asthma (Occupational Safety & Health Administration, 2013). In the United States in 2009, asthma accounted for $56 billion in total societal costs (Chang & Rivera, 2013). The annual cost of fatal injuries for wholesale and retail trade (WRT) is estimated to exceed $8.6 billion (Anderson, Schulte, Sestito, Linn, & Nguyen, 2010). WRT are services that are given with the purchase and sale of merchandise. The merchandise can be in a variety of disciplines such as agriculture, mining, manufacturing, and certain information industries, such as publishing (Anderson et al., 2010). To identify occupationally related disease, primary care providers must maintain a high degree of suspicion and have the following:
 Familiarity with the basic principles of occupational and environmental medicine
Familiarity with the basic principles of occupational and environmental medicine
 Ability to take an occupational and environmental history
Ability to take an occupational and environmental history
 Understanding of the worker’s compensation system
Understanding of the worker’s compensation system
 Awareness of the ethical, legal, and social implications of occupation- and environment-related conditions
Awareness of the ethical, legal, and social implications of occupation- and environment-related conditions
 Knowledge of when and how to report hazards to public health and regulatory authorities
Knowledge of when and how to report hazards to public health and regulatory authorities
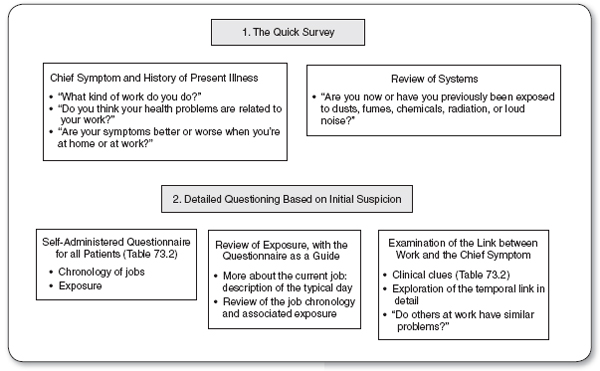
Figure 73.1 outlines an initial clinical approach to the recognition of illness caused by occupational exposure. Table 73.2 lists the essential elements of an occupational history.
Workers in small- and medium-sized companies may be at higher risk for exposure to occupational hazards because their employers are less likely to know the characteristics of hazardous substances in use (Sattler, 1992). Persons who are employed in low-wage, nonprofessional work are at higher risk for a work-related illness and injury because it generally involves more manual labor and more exposure to physical and chemical hazards (Stanbury & Rosenman, 2013).
 OCCUPATIONAL ASTHMA
OCCUPATIONAL ASTHMA
Anatomy, Physiology, and Pathology
Occupational asthma can be defined as a variable airflow limitation and/or hyperresponsiveness associated with inflammation due to causes and conditions attributable to a particular occupational environment and not to stimuli encountered outside the workplace (Baur et al., 2012). The cause of asthma can be either allergic or nonallergic. Allergic occupational asthma develops after a period of allergic sensitization to a substance found at work over a period of months to years and is characterized by intermittent airflow limitation. Although the respiratory symptoms are variable, they always occur at work.
Nonallergic occupational as thma is usually the result of high-level exposures to an irritant gas, fume, aerosol, or vapor. It develops without a latency period and is distinguished by persistent nonspecific airway hyperresponsiveness. Although this nonallergic bronchospasm is referred to as reactive airway dysfunction syndrome, it is not true asthma, even though clinically it presents in a similar fashion (Chan-Yeung, 1990).
Estimates of the prevalence of occupational a sthma have ranged between 9% and 15% of all asthmatic adults (Bardana, 2008). The prevalence within industries varies widely and is determined by the agents used in the workplace. The prevalence within a particular industry depends on the type, source, and concentration of the agent, as well as conditions at the workplace.
Occupational Pulmonary Disorders |
Occupational asthma
Asthma due to allergic sensitization
Other forms of occupational asthma
Pneumoconiosis
Silicosis
Asbestosis
Talcosis
Coal workers’ pneumoconiosis, mixed dust fibrosis, berylliosis hard metal disease
Nonspecific airway disease
Hypersensitivity pneumonitis (extrinsic allergic alveolitis)
Inhaled toxic gases
Respiratory tract cancer
Occupationally linked pulmonary infections
Diagnostic Criteria
The task of the primary care provider is twofold. The first is to diagnose asthma, which may be present with varied, atypical symptoms such as cough, chest tightness, wheeze, shortness of breath, and spirometry that shows significantly reversible airflow limitation (Hoy, Abramson, & Sim, 2010). The second task is to connect symptomatic episodes to the workplace.
Serial measurements of peak expiratory flow (PEF) on workdays and rest days are recommended as the first objective method for confirming occupational a sthma (Moore et al., 2009). A sound connection to the workplace can be made with serial peak flow measurements at home and work. Another strategy is to perform the “stop-resume” work test, in which the patient measures and records peak flow rates every 2 hours while awake both at home and work. Measurements are made on days at work and days away from work. The record should be kept for a total of 4 consecutive weeks (Moore et al., 2009). If it is not possible to monitor peak flow rates in this detailed way, the patient should be removed from work for 1 to 2 weeks and then carefully monitored for symptoms on return.
FIGURE 73.1
The initial clinical approach to the recognition of illness caused by occupational exposure.
Source: Newman (1995).
Materials in the workplace that are linked to asthma are listed in Table 73.3. Many agents can cause occupational asthma, and new agents are identified every year. An individual can be referred to a specialist when the diagnosis is uncertain, and this may be necessary for individuals who are suspected to have occupational asthma (Hoy et al., 2010). An occupational medicine specialist may perform skin testing, immunologic studies, and bronchial inhalation challenges.
Essential Elements of the Occupational History and Questionnaire |
CURRENT OR MOST RECENT WORK AND EXPOSURE HISTORY | |
Job title; type of industry; name of employer Year work started and year work finished (if not currently employed) Description of job (what is a typical workday), especially the parts of the job the patient believes may be potentially hazardous Current work hours and any shift changes Current exposure to dust, fumes, radiation, chemicals, biological hazards, or physical hazards Protective equipment used (clothes, safety glasses, hearing protection, respirator, or gloves) Other employees at the workplace who have similar health problems | |
EARLIER EMPLOYMENT HISTORY | |
Job chronology, working backward from the current or most recent job The same information as above for each job previously held | |
MAJOR TYPES OF EXPOSURE ASSOCIATED WITH CLINICAL ILLNESS | |
Gases Corrosive substances (acids, alkalis) Dyes and stains Dusts and powders Asbestos, other fibers Infectious agents Insecticides and pesticides Metals and metal fumes Organic dusts (cotton, wood, biological matter) | Plastics Solvents Petrochemicals (coal, tar, asphalt, petroleum distillates) Physical factors (noise, lifting, thermal stress, vibration, repetitive motion) Emotional factors (stress) Radiation (electromagnetic fields, x-ray radiation, ultraviolet radiation) |
Source: Newman (1995).
History and Physical Examination
Any adult presenting with new-onset asthma should be evaluated for occupational asthma. The medical history for these patients is detailed in Table 73.4. The primary care provider should look for aggravating agents in the workplace and should attempt to elicit a relation between symptoms and work. Occupational factors that worsen the symptoms of a patient with stable preexisting asthma should also be sought.
The physical examination should focus on the respiratory tract and skin (see Chapter 69). Rhinitis, nasal polyps, hyperinflation of the lungs, and a prolonged expiratory phase should be noted. Eczema may suggest the presence of atopy.
Diagnostic Studies
All patients with new onset of asthma-like symptoms should receive a symptom questionnaire, blood test to look for antibodies to the substance, allergy skin test, bronchial provocation test, complete blood count, PEF rate, chest radiograph, and pulmonary function tests (A.D.A.M, 2013). Other testing may be done as described in the “Diagnostic Criteria” section.
Some Products That Are Linked to Asthma |
VEGETABLE MATERIAL | ANIMAL MATERIAL |
Grain dust | Danders |
Flour | Insects |
Fig plants | Silkworm larvae |
Wood dust | Shellfish |
Seaweed | Excreta (pigs, chickens) |
Green coffee beans | Fish feed |
Fungal spores | Animal enzymes |
Gum tragacanth | Metals |
Castor bean | Stainless steel |
Tea | Galvanized steel |
Tobacco | Aluminum fluoride |
Flax | Vanadium |
Hemp | Cobalt |
Cotton | Tungsten carbide (cobalt) |
Hops | Platinum salts |
Bacterial enzymes | Nickel |
Colophony | Chromium |
PLASTICS/CHEMICALS | PHARMACEUTICALS |
Acid anhydrides | Penicillins |
Epoxy resins | Cephalosporins |
Diisocyanates (TDI, MDI, HDU) | Piperazine |
Persulfate salts | Psyllium |
Paraphenylene diamine | Methyldopa |
Phthalic anhydride | Spiramycin |
Dimethyl ethananolamine | Tetracycline |
Azobisformamide | Amprolium |
Azodicarbonamide | Cimetidine |
Formaldehyde | Isoniazid |
Ethylenediamine | Phenylglycine |
Acrylates |
|
Henna |
|
HDU, hexamethylene diurethane; MDI, methylene diphenyl diisocyanate; TDI, toluene diisocyanate.
Source: Cullen (1990).
Treatment Options, Expected Outcomes, and Comprehensive Management
Occupational asthma is treated the same way as is asthma that is not related to the workplace. However, in occupational asthma, an additional goal is to eliminate exposure to the causative agent. The patient should be advised to have reduced exposure if complete removal cannot be achieved, although it should be clearly stated that deaths have been reported in subjects who remain exposed (Malo, 2005).
For patients with occupational asthma secondary to sensitization, removal from the work environment is strongly recommended because even minute exposures to the offending agent may cause fatal bronchospasm. Worsening asthma is an indication that immediate removal is necessary. Even after removal from the workplace, a patient may continue to be symptomatic from asthma for an indefinite period of time (Malo, 2005).
Medical History for Occupational Asthma |
I. | Symptoms | ||
| A. | Cough, wheezing, shortness of breath, chest tightness, and sputum production (generally of modest degree) | |
| B. | Conditions known to be associated with asthma, such as rhinitis, sinusitis, nasal polyposis, or atopic dermatitis | |
II. | Pattern of symptoms | ||
| A. | Perennial, seasonal, or perennial with seasonal exacerbations | |
| B. | Continuous, episodic, or continuous with acute exacerbations | |
| C. | Onset, duration, and frequency of symptoms (days per week or month) | |
| D. | Diurnal variation, with special reference to nocturnal symptoms | |
III. | Precipitating or aggravating factors | ||
| A. | Viral respiratory infections | |
| B. | Exposure to environmental allergens (pollen, mold, house-dust mite, cockroach, animal dander, or secretory product, such as saliva or urine) | |
| C. | Exposure to occupational chemicals or allergens | |
| D. | Environmental change (e.g., moving to a new home, going on a vacation, alterations in workplace, work processes, or materials used) | |
| E. | Exposure to irritants, especially tobacco smoke and strong odors, air pollutants, occupational chemicals, vapors, gases, and aerosols | |
| F. | Emotional expressions: fear, anger, frustration, crying, hard laughing | |
| G. | Drugs (aspirin, beta-blockers, nonsteroidal anti-inflammatory drugs, others) | |
| H. | Food additives (sulfites) and preservatives | |
| I. | Changes in weather, exposure to cold air | |
| J. | Exercise | |
| K. | Endocrine factors (e.g., menses, pregnancy, thyroid diseases) | |
IV. | Development of disease | ||
| A. | Age of onset, age at diagnosis | |
| B. | Progress of disease (better or worse) | |
| C. | Previous evaluation, treatment, and response | |
| D. | Present management and response, including plans for managing acute episodes | |
V. | Profile of typical exacerbation | ||
| A. | Prodromal signs and symptoms (e.g., itching of skin of the anterior neck, nasal allergy symptoms) | |
| B. | Temporal progression | |
| C. | Usual management | |
| D. | Usual outcome | |
VI. | Living situation | ||
| A. | Home age, location, cooling and heating (central with oil, electric, gas, or kerosene space heating), wood-burning fireplace | |
| B. | Carpeting over a concrete slab | |
| C. | Humidifier | |
| D. | Description of patient’s room, with special attention to pillow, bed, floor covering, and dust collectors | |
| E. | Animals in home | |
| F. | Exposure to cigarette smoke, direct or sidestream, in home | |
VII. | Impact of disease | ||
| A. | Impact on patient | |
|
| 1. | Number of emergency department or urgent care visits and hospitalization |
|
| 2. | History of life-threatening acute exacerbation, intubation, or oral steroid therapy |
|
| 3. | Number of school or work days missed |
|
| 4. | Limitation of activity, especially sports |
|
| 5. | History of nocturnal awakening |
|
| 6. | Effect on growth, development, behavior, school or work achievement, and lifestyle |
| B. | Impact on family | |
|
| 1. | Disruption of family dynamics, routines, or restriction of activities |
|
| 2. | Effect on siblings, spouse |
|
| 3. | Economic impact |
VIII. | Assessment of family’s and patient’s perception of illness | ||
| A. | Patient, parental, and spousal knowledge of asthma and belief in the chronicity of asthma and in the efficacy of treatment | |
| B. | Ability of patient and parents or spouse to cope with disease | |
| C. | Level of family support and patient and parents’ or spouse’s capacity to recognize severity of an exacerbation | |
| D. | Economic resources | |
IX. | Family history | ||
| A. | Immunoglobulin E (IgE)-mediated allergy in close relatives | |
| B. | Asthma in close relatives | |
X. | Medical history | ||
| A. | General medical history and history of other allergic disorders (e.g., chronic rhinitis, atopic dermatitis, sinusitis, nasal polyps, gastrointestinal disturbances, adverse reactions to foods, drugs); in children, history of early life injury to the airways (e.g., bronchopulmonary dysplasia, history of pulmonary infiltrates, documented pneumonia, viral bronchiolitis, recurrent croup, symptoms of gastroesophageal reflux, passive exposure to cigarette smoke); in adults, cigarette smoking history | |
| B. | Detailed review of symptoms | |

Full access? Get Clinical Tree