CHAPTER 19
Occipital Nerve Blocks
INTRODUCTION
Beruto and Ramus first described occipital neuralgia in 1821.1 In the beginning of the 1900’s, Luff2 as well as Osler and McRae3 emphasized occipital neuralgia as a cause of occipital pain and headaches. Most patients with primary headache syndromes who have frequent attacks of pain have tenderness in the suboccipital region.4 Neural blockade of the greater, lesser, and third occipital nerves are interventions employed in the diagnosis and treatment of upper neck pain and headache believed to be caused by pathology in the superior cervical spine. In the clinical setting, neck pain and headache are common complaints, so, when evaluating such patients, the clinician will be well served by eliciting as precise a history as possible and seeking any past cervical spine or head trauma.
INDICATIONS
The medical terms occipital neuralgia and cervicogenic headache describe a syndrome of neck and head pain primarily referred to the occiput, as well as in the temporal area, forehead and retrobulbar areas, that may arise some distance away, in the upper cervical spine. This occurs because the first three cervical spinal nerve segments (C1-C3) that make up the occipital nerves share a relay-station in the brainstem that continues into the upper cervical spinal cord with the trigeminal cell bodies (the cervico-trigeminal nucleus), and the pain of occipital neuralgia and cervicogenic headaches is referred to structures innervated by the branches of the trigeminal nerve, namely, the forehead, temples, and eyes (Figure 19-1). Neuralgia of C2 (occipital neuralgia) is typically described as a deep or dull pain that usually radiates from the occipital to parietal, temporal, frontal, and periorbital regions. A paroxysmal sharp or shock-like pain is often superimposed over the constant pain. Ipsilateral eye lacrimation and conjunctival injection are common associated signs.5
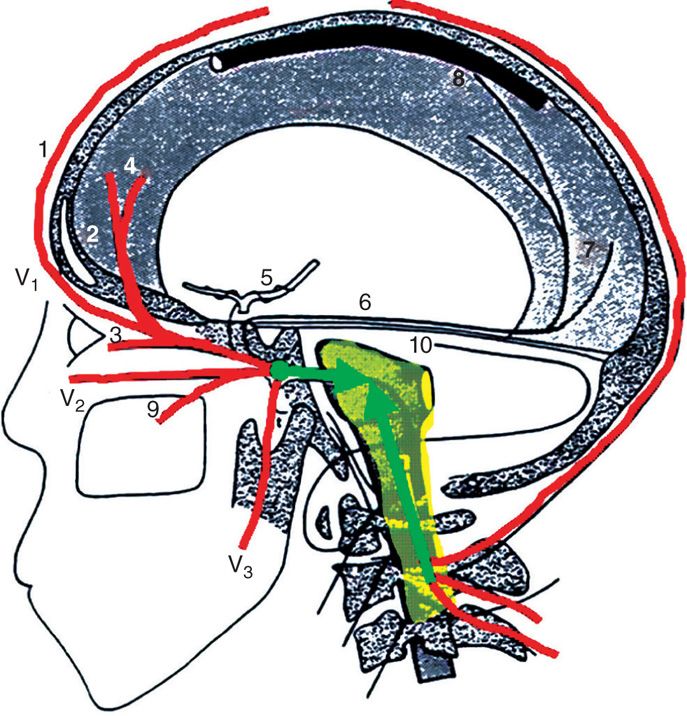
Figure 19-1. Cervico-trigeminal nucleus. (Used with permission from Dr. David Schultz.)
Indications for occipital nerve blocks therefore include:
• Neck pain felt in the upper back of the neck, potentially referring to the occiput, temporal, forehead and retrobulbar regions of the head.
• A history of whiplash injury or similar trauma.
• The presence of a migraine-like headache syndrome not responding to pharmacologic treatment alone.
CONTRAINDICATIONS
• Infection of the scalp.
• Coagulopathy.
• Cervical instability or acute fracture.
• Arnold-Chiari syndrome.
• Inability to lie in the prone or sitting position.
• Inability to provide informed consent.
RELEVANT ANATOMY
The suboccipital nerve (the dorsal ramus of C1) innervates the atlanto-occipital (AO) joint (C0-1), and thus can refer pain to the back of the head, mistakenly attributed to the occipital nerve. The C2 dorsal root ganglion and nerve root innervate the capsule of the atlanto-axial (AA) joint (C1-2) as well as the C2-3 facet, so that trauma to these joints will also refer to the occiput.
• The greater occipital nerve (GON) receives fibers from the dorsal primary rami of the second and third cervical nerve roots.
• The lesser occipital nerve (LON), however, receives fibers from the posterior rami of the second and third cervical nerves.
• The third occipital nerve (the superficial medial branch of the dorsal ramus of C3) crosses the lateral and posterior aspects of the C2-3 facet, and innervates the C2-3 zygapophyseal joint.
• The C23 joint and thus the third occipital nerve appear vulnerable to trauma from acceleration-deceleration injuries of the neck6 (Figure 19-2).
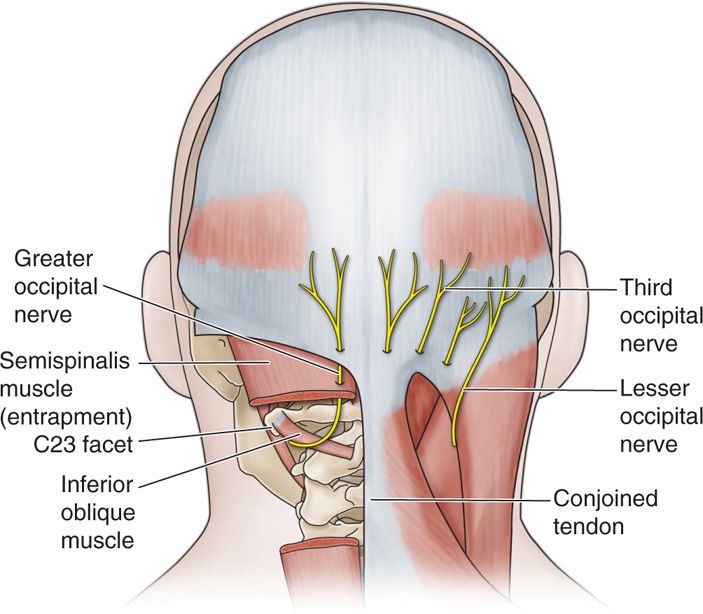
Figure 19-2. Occipital nerves.
There are usually two greater occipital nerves, two lesser occipital nerves, and two third occipital nerves in each patient, though this may be variable. For instance, in one report, bilateral triplication of the lesser occipital nerve was described.7
THE GREATER OCCIPITAL NERVE (GON)
• It exits the C2 foramen laterally, crosses over the atlanto-axial joint on top of the inferior oblique, and then ascends in the posterior neck medially, pierces the semispinalis muscle and then pierces the lateral edge of the conjoined tendon (Figure 19-3A and B).
• It then becomes superficial immediately inferior to the superior nuchal ridge, where it is joined more cephalad by the occipital artery.
• This nerve could therefore be considered to have 3 parts (part 1, part 2, and part 3) as well as two bends (bend 1 and bend 2)8 (Figure 19-4).
• The GON supplies the main sensory innervation to the posterior scalp and climbs in a cephalad fashion laterally to the vertex and temporal areas,9 where it borders with the area innervated by the supraorbital and auriculotemporal nerve.
• The actual location of the occipital nerve can be very variable; in 10 embalmed cadavers, the GON was located anywhere from 5 to 28 mm from the midline.10 In a dissection of 20 cadavers with no known headache history, the trapezius muscle was penetrated by the GON in 45% of cases, the semispinal muscle was penetrated in 90% of cases, and the inferior oblique was penetrated in 7.5% of cases.11
• When the occipital artery is palpable, the nerve will be medial to the artery.

Figure 19-3. (A, B) Occipital nerve and artery.
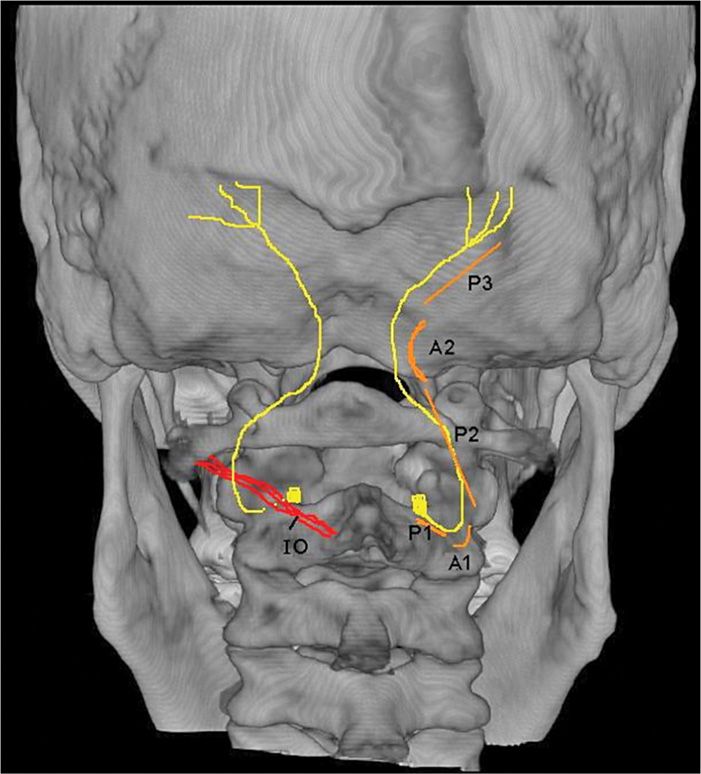
Figure 19-4. Occipital pathway. IO, internal oblique; P1, part 1; P2, part 2; P3, part 3; B1, bend 1; B2, bend 2.8
THE LESSER OCCIPITAL NERVE
• It usually arises from the posterior ramus of C23, and travels along the posterior border of the sternocleidomastoid muscle as part of the superficial cervical plexus, becoming most superficial and accessible at about the level of the mastoid process, 32 to 90 mm from the midline10 (Figure 19-5).
• Accordingly, the lesser occipital nerves supply sensory innervation to the lateral portion of the posterior scalp as well as the posterosuperior surface of the pinna of the ear12 (Figure 19-6).
• The LON has been reported to arise anomalously from the trunk of the suprascapular nerve.7
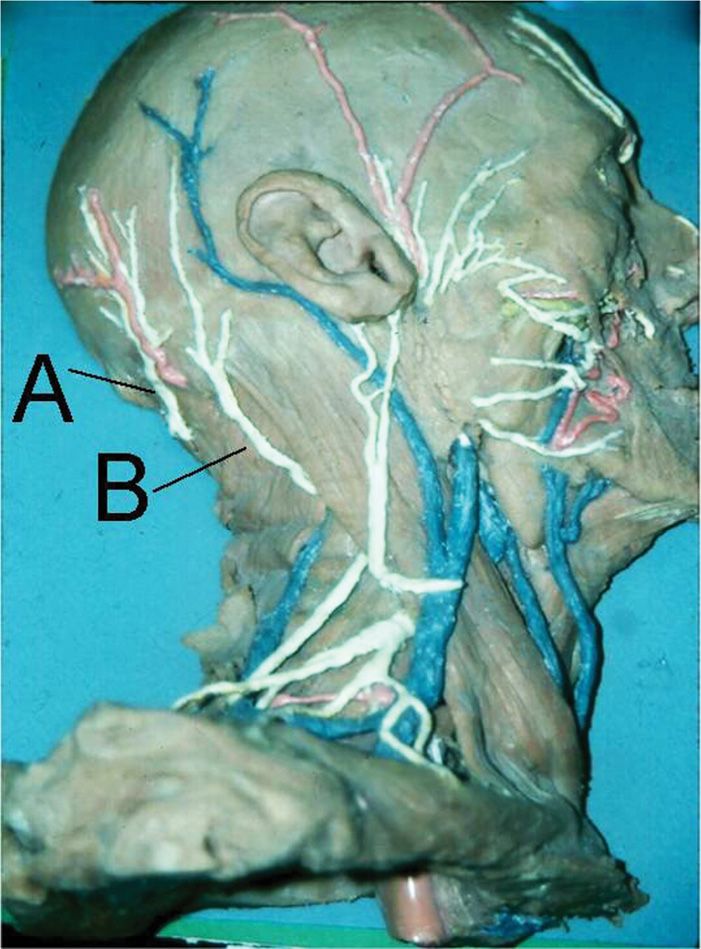
Figure 19-5. Occipital nerve dissection: A, greater occipital; B, lesser occipital.
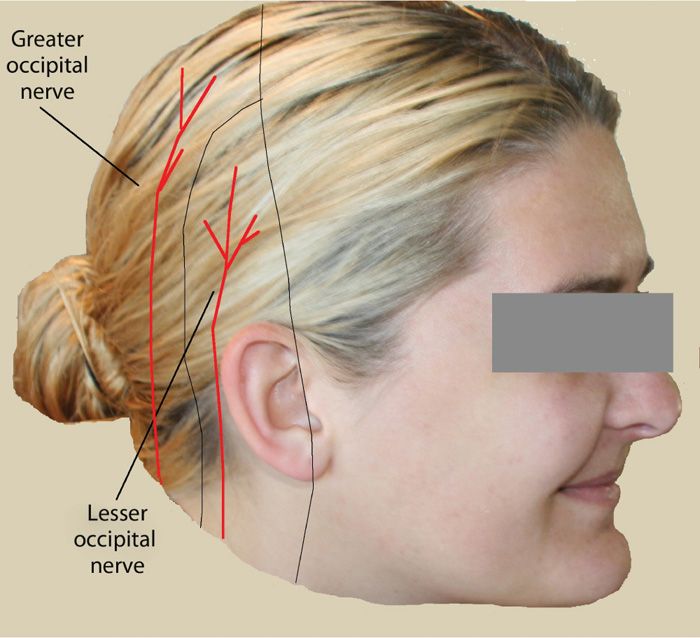
Figure 19-6. Greater occipital versus lesser occipital pattern. (Used with permission from Nicole Gear.)
The Third Occipital Nerve
• It arises from the medial sensory branch of the posterior division of C3, passes through the trapezius and splenius muscles slightly medial to the greater occipital nerve.
• It is sensory to the skin of the midline occipital region.
• It also supplies the proprioceptive fibers to the semispinalis muscles.
• The C2-3 joint and the third occipital nerve appear vulnerable to trauma from acceleration-deceleration injuries of the neck.6
Cadaver studies have shown a great variability in nerve anatomy, both interindividually and intraindividually. For example, in one study,10 the greater occipital nerve was found between 5 and 28 mm from the midline along the intermastoid line, while the lesser occipital nerve was found between 32 and 90 mm from the midline along the same landmark. In most cases, both the greater occipital nerve and the lesser occipital nerve pierced the occipital aponeurosis after branching. There can also be connections between the two (Figure 19-7).
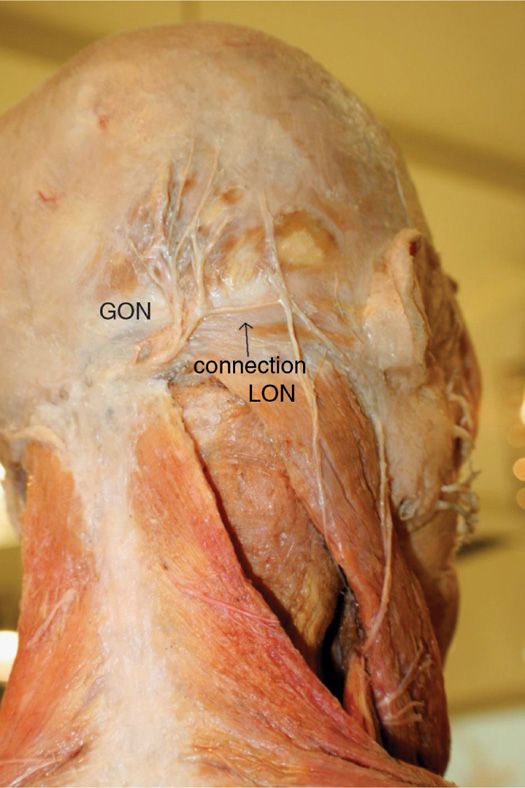
Figure 19-7. Connection between greater and lesser occipital nerves.
PREOPERATIVE CONSIDERATIONS
Although originally associated only tension-type headaches and occipital pain, entrapment of the occipital nerve has recently been recognized as one of the causes of unilateral, throbbing headaches, associated with photophobia, phonophobia, and nausea, which meet the International Headache Society criteria for migraine. Anatomic recognition of multiple occipital nerves (the greater occipital, the lesser occipital, and the third occipital nerve), each with different patterns of pain, neurologic origin, and treatment modalities, has been facilitated by the use of precision diagnostic injections and the search for more aggressive treatment of intractable headaches and upper cervical neck pain. Decisions need to be made preoperatively as to blind versus fluoroscopic versus ultrasound guidance, as well as distal versus proximal injections. In general, the more distal the injection, the lesser the need for image guidance, but the more likely one is to miss the entrapment.
According to a prospective study by Afridi et al,4 there was no significant association between presence of anesthesia in the distribution of the GON after an injection and the response to occipital nerve blocks, but there was a significant relationship between tenderness in the occipital region, and response. Unfortunately, there is no standardized approach to occipital nerve injections, with volumes of injectate ranging from 0.5 to 10 cc,13 local anesthetic with or without steroids13 or botulinum toxin,14,15 with or without epinephrine, single injections or up to 10 injections,13 followed for 1 week16 up to 6 months, which has made comparing efficacy difficult.
DOCUMENTATION FOR OFF-LABEL INDICATIONS
Because of the plethora of techniques available and the large volumes usually used, as well as the lack of a “gold standard,” there has been a great deal of confusion and a lack of convincing evidence regarding the efficacy and effectiveness of occipital nerve block. As a result, many insurance companies have deemed this procedure “experimental.” In addition, the AMA CPT code 64405 is specific for greater occipital nerve blocks, and there is not currently a specific code for lesser or third occipital nerves. Nor is there a specific code for fluoroscopic or ultrasound guidance, or for the occipital decompression technique (see below). Patients need to be made aware of these “off label” uses.
FLUOROSCOPIC VIEWS
Although often performed as a blind technique (see below), fluoroscopy is utilized for the more proximal injections at the C2 and C3 facet level (Figure 19-8) and the occipital decompression approach (see below).
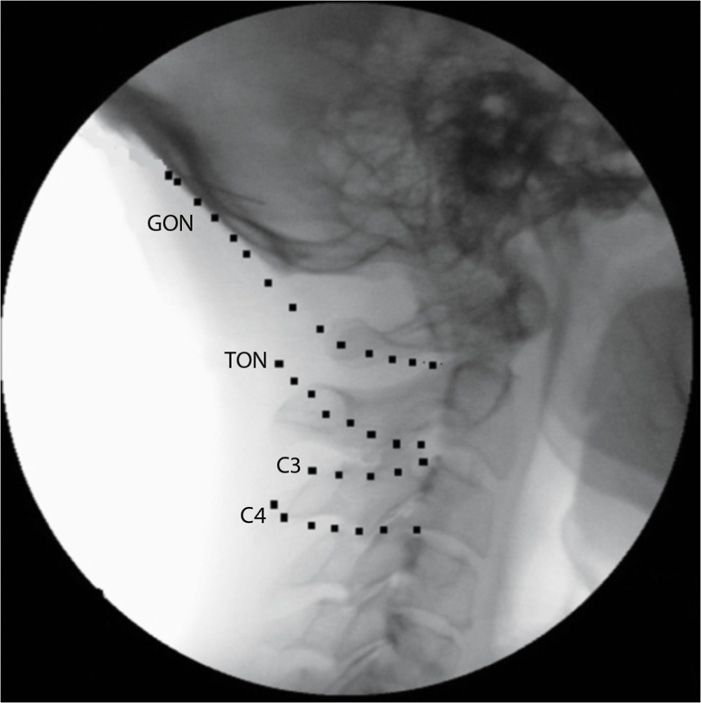
Figure 19-8. Fluoroscopic location of occipital nerves.
POSITIONING OF PATIENT
For the blind procedure, the patient is positioned seated, neck flexed, with their head supported on their hands. This position may also be desirable for ultrasound imaging as well. For fluoroscopic imaging, the patient is usually positioned prone.
SELECTION OF NEEDLES, MEDICATIONS, AND EQUIPMENT
• Equipment for a blind diagnostic or therapeutic occipital nerve block includes:
![]() A 3-cc syringe for each site
A 3-cc syringe for each site
![]() An 18-gauge needle to draw up the desired local anesthetic and corticosteroid solution
An 18-gauge needle to draw up the desired local anesthetic and corticosteroid solution
![]() A 27-gauge needle for injection
A 27-gauge needle for injection
![]() A pair of sterile procedure gloves
A pair of sterile procedure gloves
![]() Alcohol swabs
Alcohol swabs
![]() Local anesthetic, either 1% to 2% lidocaine or 0.5% bupivacaine
Local anesthetic, either 1% to 2% lidocaine or 0.5% bupivacaine
![]() Corticosteroid
Corticosteroid
![]() Although a deposteroid is most desired for longer-term effect, there is concern that the proximity of the vertebral occipital arteries could lead to an unexpected vascular injection. Dr Gabor Racz (personal communication), therefore, recommends that a particulate-free steroid be used.
Although a deposteroid is most desired for longer-term effect, there is concern that the proximity of the vertebral occipital arteries could lead to an unexpected vascular injection. Dr Gabor Racz (personal communication), therefore, recommends that a particulate-free steroid be used.
• Additional equipment for a fluoroscopic diagnostic or therapeutic occipital nerve block includes:
![]() Fluoroscopic imaging equipment and table
Fluoroscopic imaging equipment and table
![]() Because of potential vascular injections, consider equipment with digital subtraction angiography (DSA) capability
Because of potential vascular injections, consider equipment with digital subtraction angiography (DSA) capability
![]() A 30-gauge needle for skin infiltration
A 30-gauge needle for skin infiltration
![]() A 22-gauge 3.5-in Quincke-type needle vs a 20-gauge blunt tip needle with introducer
A 22-gauge 3.5-in Quincke-type needle vs a 20-gauge blunt tip needle with introducer
![]() Nonionic contrast
Nonionic contrast
• Additional equipment for an ultrasound diagnostic or therapeutic occipital nerve block includes:
![]() Ultrasound imaging equipment
Ultrasound imaging equipment
![]() Consider ultrasound-enhanced needles
Consider ultrasound-enhanced needles
• Additional equipment for an occipital adhesiolysis includes:
![]() Fluoroscopic imaging equipment and table
Fluoroscopic imaging equipment and table
![]() A Stealth needle (Epimed®, Johnstown, NY)
A Stealth needle (Epimed®, Johnstown, NY)
![]() A 18-gauge needle to break the skin
A 18-gauge needle to break the skin
![]() Nonionic contrast
Nonionic contrast
![]() Preservative-free saline
Preservative-free saline
INTRAOPERATIVE TECHNICAL STEPS
• Blind technique
![]() The greater, lesser, and third occipital nerves may be blocked with the patient either sitting with the head flexed forward and the head resting on the hands or lying prone on an examination table. If prone, a pillow placed underneath the chest permits easier flexion of head and neck. The clinician stands behind the patient if sitting and on the left side of the patient (if right handed) when the patient is prone. Routine monitors such as a blood pressure cuff and pulse oximeter may be used, but an IV and sedation are generally not required.
The greater, lesser, and third occipital nerves may be blocked with the patient either sitting with the head flexed forward and the head resting on the hands or lying prone on an examination table. If prone, a pillow placed underneath the chest permits easier flexion of head and neck. The clinician stands behind the patient if sitting and on the left side of the patient (if right handed) when the patient is prone. Routine monitors such as a blood pressure cuff and pulse oximeter may be used, but an IV and sedation are generally not required.
![]() The classic approach involves identifying the nuchal ridge, feeling for the occipital artery, and injecting a large volume (up to 10 cc) medial to the artery or as a strip (Figure 19-9). This was initially described as a technique for surgical anesthesia, attempting to anesthetize all three nerves at the same time.
The classic approach involves identifying the nuchal ridge, feeling for the occipital artery, and injecting a large volume (up to 10 cc) medial to the artery or as a strip (Figure 19-9). This was initially described as a technique for surgical anesthesia, attempting to anesthetize all three nerves at the same time.
![]() For the Trescot approach,17 3 landmarks are appreciated with the clinician’s left hand: the foramen magnum, the conjoined tendon, and the occipital nerve groove of the skull just lateral to the tendon (Figure 19-10A, B, and C).
For the Trescot approach,17 3 landmarks are appreciated with the clinician’s left hand: the foramen magnum, the conjoined tendon, and the occipital nerve groove of the skull just lateral to the tendon (Figure 19-10A, B, and C).
![]() The scalp can be cleaned over the planned injection sites with an alcohol pad.
The scalp can be cleaned over the planned injection sites with an alcohol pad.
![]() Complete sterilization of the scalp is not necessary and the hair should not be shaved.
Complete sterilization of the scalp is not necessary and the hair should not be shaved.
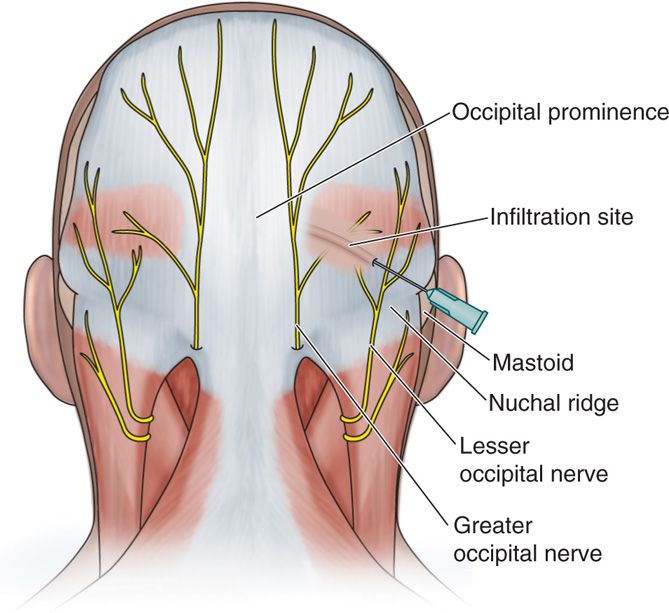
Figure 19-9. Occipital nerve injection sites and landmarks: A, traditional anesthesia injection technique; B, Trescot occipital injection site; C, lesser occipital entrapment site; D, conjoined tendon.
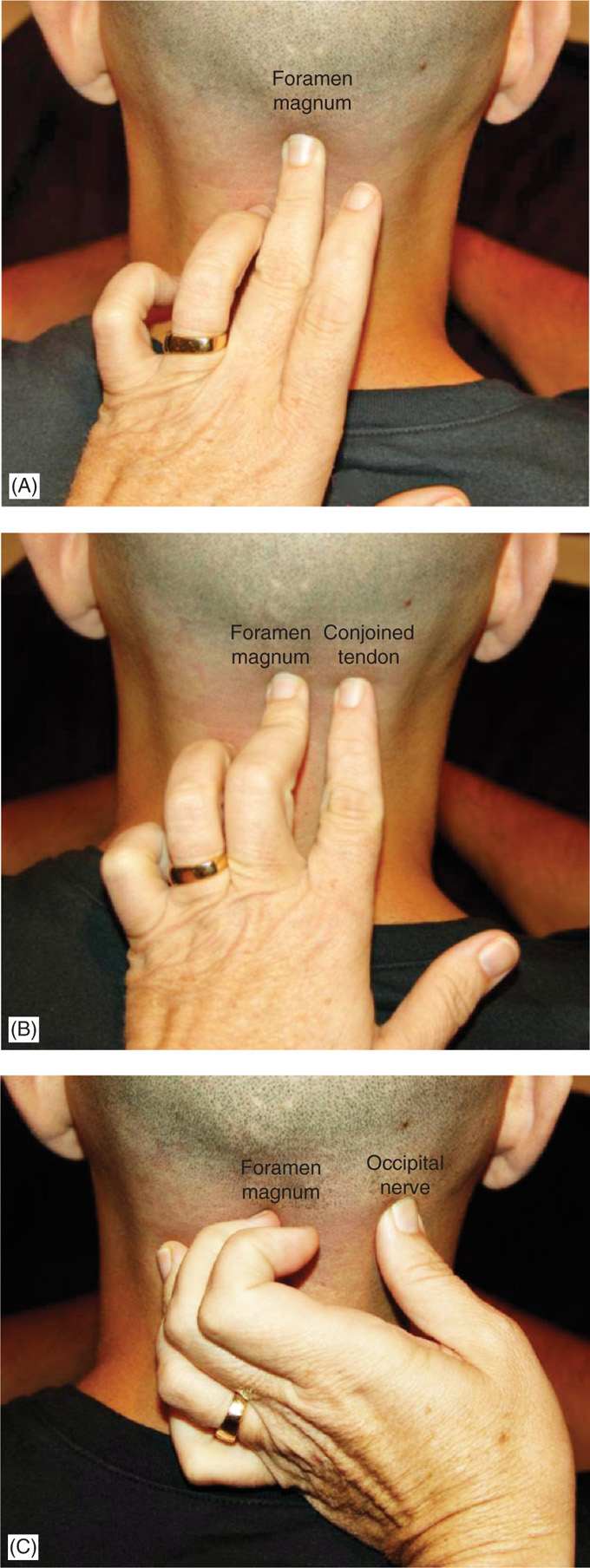
Figure 19-10. (A) Examiner’s middle finger in the foramen magnum. (B) Examiner’s index finger on the conjoined tendon. (C) Examiner’s thumb on the occipital nerve.
![]() The small-gauged needle (27 gauge 1.5 inch) is aimed superiorly and medially and advanced until contact is made with the bony skull (Figure 19-11). After aspiration, injection may then be made of no more than 2 cc of the therapeutic solution (local anesthetic and steroid). Note that this injection site is inferior to the nuchal line, the site of traditional injections.
The small-gauged needle (27 gauge 1.5 inch) is aimed superiorly and medially and advanced until contact is made with the bony skull (Figure 19-11). After aspiration, injection may then be made of no more than 2 cc of the therapeutic solution (local anesthetic and steroid). Note that this injection site is inferior to the nuchal line, the site of traditional injections.
![]() Injection of the lesser occipital nerve is made with a second needle insertion just behind the mastoid process. Often a groove can be palpated. After testing aspiration again, 1 cc of therapeutic solution can be then injected to block the lesser occipital nerve.
Injection of the lesser occipital nerve is made with a second needle insertion just behind the mastoid process. Often a groove can be palpated. After testing aspiration again, 1 cc of therapeutic solution can be then injected to block the lesser occipital nerve.
![]() The distal third occipital nerve can be injected just medial to the attachment of the conjoint tendon on the occipital condyles, taking care to avoid the foramen magnum by angling the needle medial to lateral and contacting bone.
The distal third occipital nerve can be injected just medial to the attachment of the conjoint tendon on the occipital condyles, taking care to avoid the foramen magnum by angling the needle medial to lateral and contacting bone.

Figure 19-11. Occipital injection technique.
• Fluoroscopy guided injections
![]() Third occipital nerve blocks are often performed under fluoroscopic guidance at the level of the C2-C3 facet.6 In patients with neck pain and headache after whiplash, the prevalence of pain stemming from the C2-C3 zygapophysial joint was found to be 27%. Among those patients in whom headache was the dominant feature, the prevalence increased to 53%.18 The third occipital nerve most often crosses the C2-C3 joint opposite the center of the C3 superior articular process, but it may run lower or higher than this plane. Because of anatomic variations, a radiofrequency needle is placed opposite the middle of the joint as well as above and below this point19 (Figure 19-12).
Third occipital nerve blocks are often performed under fluoroscopic guidance at the level of the C2-C3 facet.6 In patients with neck pain and headache after whiplash, the prevalence of pain stemming from the C2-C3 zygapophysial joint was found to be 27%. Among those patients in whom headache was the dominant feature, the prevalence increased to 53%.18 The third occipital nerve most often crosses the C2-C3 joint opposite the center of the C3 superior articular process, but it may run lower or higher than this plane. Because of anatomic variations, a radiofrequency needle is placed opposite the middle of the joint as well as above and below this point19 (Figure 19-12).
![]() Occipital adhesiolysis or suboccipital decompression is a technique developed by Dr Gabor Racz to approach the high cervical entrapment of the occipital nerve. A blunt-tipped, curved, winged needle (Figure 19-13A), called a Stealth ™ needle, is introduced from cephalad to caudad (Figure 19-13B), hugging the inferior occipital bone. This allows fluid to be used to lyse adhesions around the occipital nerve to decompress the nerve (Figure 19-13C).
Occipital adhesiolysis or suboccipital decompression is a technique developed by Dr Gabor Racz to approach the high cervical entrapment of the occipital nerve. A blunt-tipped, curved, winged needle (Figure 19-13A), called a Stealth ™ needle, is introduced from cephalad to caudad (Figure 19-13B), hugging the inferior occipital bone. This allows fluid to be used to lyse adhesions around the occipital nerve to decompress the nerve (Figure 19-13C).
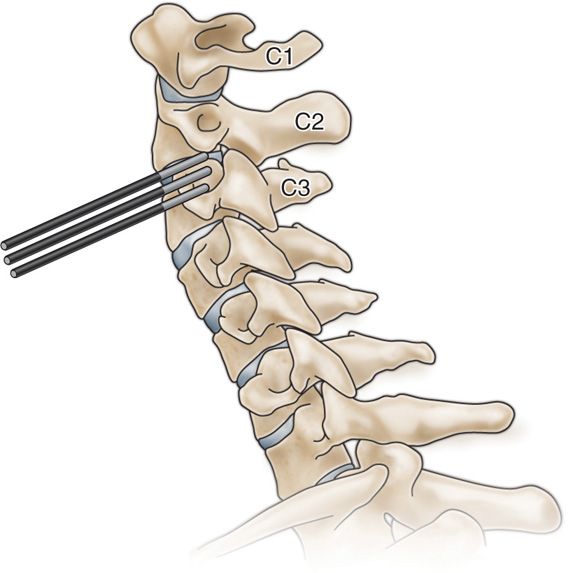
Figure 19-12. Radiofrequency sites for third occipital nerve denervation.18
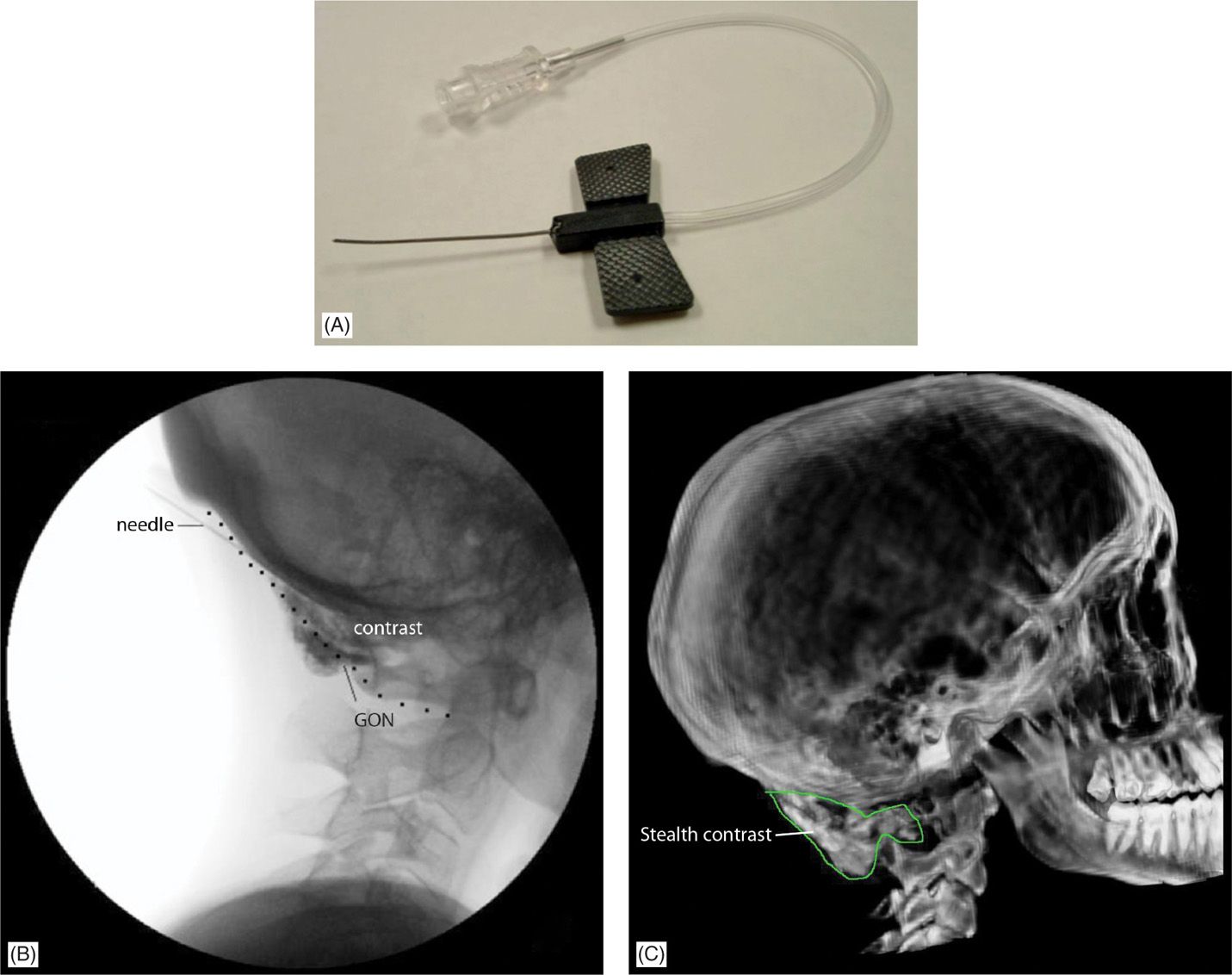
Figure 19-13. (A) Stealth needle (Epimed International). (B) Fluoroscopic view of contrast during suboccipital injection. (C) CT 3D reconstruction after suboccipital injection. (Used with permission from Andrea Trescot, MD.)
• Ultrasound injections
![]() Using ultrasound, the occipital nerve can be identified as it crosses the inferior oblique muscle (Figure 19-14). Greher et al20 described an anatomic study using ultrasound to compare the traditional injection site at the nuchal ridge with a more proximal technique (Figure 19-15). Using 0.1 cc injections of dye, they used ultrasound to identify the GON bilaterally in 10 cadavers (Figure 19-16). They reported successful injection of the GON distally in 16/20 dissections, while 20/20 of the proximal GON was stained with dye.
Using ultrasound, the occipital nerve can be identified as it crosses the inferior oblique muscle (Figure 19-14). Greher et al20 described an anatomic study using ultrasound to compare the traditional injection site at the nuchal ridge with a more proximal technique (Figure 19-15). Using 0.1 cc injections of dye, they used ultrasound to identify the GON bilaterally in 10 cadavers (Figure 19-16). They reported successful injection of the GON distally in 16/20 dissections, while 20/20 of the proximal GON was stained with dye.
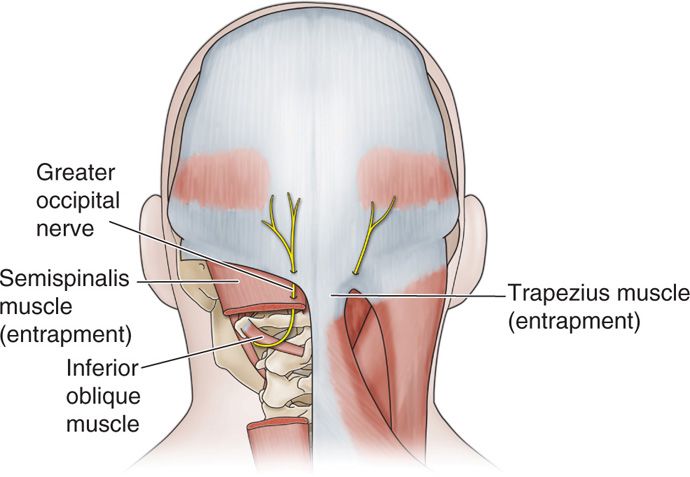
Figure 19-14. Occipital nerve entrapment internal oblique.
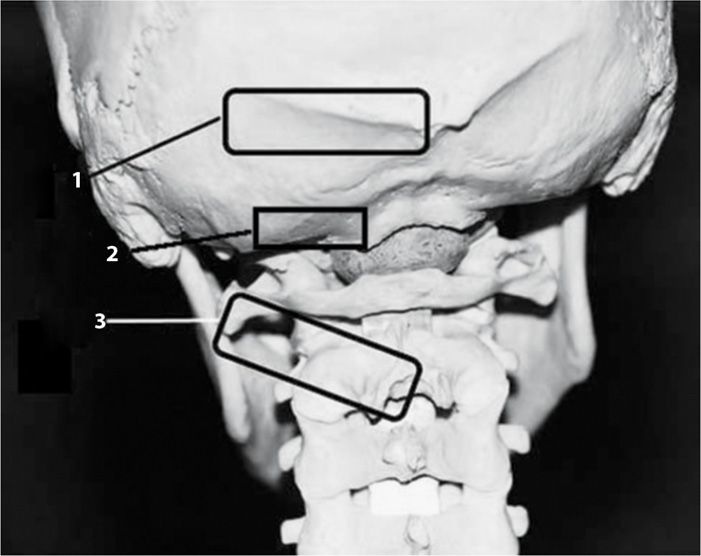
Figure 19-15. Location of ultrasound transducer (1 = standard occipital nerve injection site; 2 = Trescot approach injection site; 3 = Greher et al20 approach).
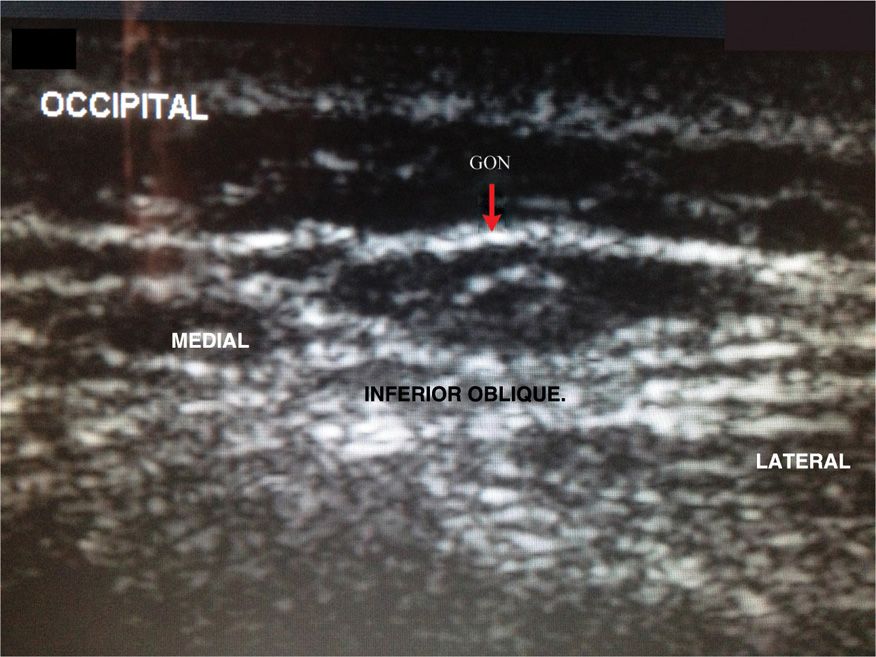
Figure 19-16. Ultrasound image of the occipital nerve on the inferior oblique. (Used with permission from Andrea Trescot, MD.)
POSTPROCEDURE CONSIDERATIONS
• Because the scalp is highly vascular, a hematoma can form; thus, manual pressure should be applied for several minutes to ensure both hemostasis and adequate coverage of the nerve branches.
• Postprocedure, most patients will report that the back of the neck and head now feels “numb,” or “frozen.” Many patients who were in the midst of a severe cervicogenic headache will report immediate improvement of neck pain and headache symptoms.
• The patient should be encouraged to rest in the waiting room for about 10 minutes, if no IV sedation was administered.
• Although counterintuitive, hypoesthesia over the occipital area does not appear to be necessary for headache relief. Alfridi et al4 reported that decreased pin-prick sensation occurred in only 12 of 23 injections that resulted in complete pain relief, and in 20 of 35 with partial relief. Supplemental pharmacotherapy is often indicated, such as anticonvulsants, anti-inflammatories, and muscle relaxants, and is synergistic with well-performed greater and lesser occipital blocks. The reader is referred to standard references for discussions of the pharmacotherapy of headache, since drug therapy for “migraines” is sometimes helpful for occipital neuralgia and cervicogenic headache. Physical therapy is also sometimes added to the above injections and drug therapy, particularly in instances of whiplash or athletic neck injury.
• Postoperatively, mild ataxia and unsteadiness can be anticipated in most subjects, particularly when looking downward, owing to the loss of tonic neck reflexes. The patient can expect the unsteadiness to gradually subside, especially if visual cues including fixing on the horizon are utilized. Patients should not drive a car until their ataxia and unsteadiness has completely resolved.
• Alopecia and skin atrophy can occur after steroid injections.21
• Infection of the injection site can occur, but is uncommon if proper aseptic technique is used.
• Patients with a history of blunt trauma to the occiput or prior posterior fossa surgery may have a defect in the skull, allowing, direct entry into the cranial vault, which may result in a total spinal anesthesia or brain injury.22
• Monitoring of potential complications
![]() Inadvertent intravascular injection is rare, if one aspirates before injecting.
Inadvertent intravascular injection is rare, if one aspirates before injecting.
![]() Inadvertent injection into the foramen magnum is theoretically possible, although even rarer.
Inadvertent injection into the foramen magnum is theoretically possible, although even rarer.
![]() Nevertheless, as with any interventional procedure, cardiorespiratory resuscitation equipment, automatic blood pressure cuff, ECG monitor, IV lines, laryngoscope and endotracheal tubes, plus oxygen and Ambu bag and ACLS-trained personnel must be immediately available.
Nevertheless, as with any interventional procedure, cardiorespiratory resuscitation equipment, automatic blood pressure cuff, ECG monitor, IV lines, laryngoscope and endotracheal tubes, plus oxygen and Ambu bag and ACLS-trained personnel must be immediately available.
![]() Specific identification of the foramen magnum prior to injection (see Trescot technique above) should decrease that risk.
Specific identification of the foramen magnum prior to injection (see Trescot technique above) should decrease that risk.
CLINICAL PEARLS AND PITFALLS
• Occipital nerve blocks are simple office procedures that are underutilized in the treatment of occipital neuralgia and cervicogenic headache.
• Anatomically and physiologically, occipital nerve blocks approximate C2 and C3 nerve root blockade, and a first set of injections can be performed easily—even at the conclusion of the patient’s first office visit.
• Occipital nerve injections have proven useful in the diagnosis and treatment of many forms of cephalgia, including occipital neuralgia, extracranial “migraine,” cervicogenic headache, whiplash and “cluster” headache. Its utility as a diagnostic technique capable of discriminating between these related types of headache has not been well studies, primarily because of the lack of standardized techniques.
• Lasting therapeutic benefit in occipital neuralgia and/or cervicogenic headache usually requires a series of a several injections.
• Combining this minor interventional procedure with appropriate pharmacotherapy and physical therapy yallows many patients a lasting beneficial outcome.
• Persistent pain that responses only temporarily to low volume occipital nerve injections may respond to botulinum toxin (to release the trapezius entrapment), cryoneuroablation of the GON/LON, radiofrequency lesioning of the third occipital nerve, occipital stimulation, or regenerative injection therapy (prolotherapy).

Full access? Get Clinical Tree






