CHAPTER 63
Obturator Nerve Block
INDICATIONS
The obturator nerve innervates a portion of the hip joint, most of the adductor muscles, a variable portion of the medial aspect of the femur, and has variable skin distribution on the medial aspect of the thigh.
The indications for blockade include:
• For acute and subacute pain
![]() Supplementation of femoral and sciatic nerve blocks for lower extremity surgery, especially knee surgery
Supplementation of femoral and sciatic nerve blocks for lower extremity surgery, especially knee surgery
![]() For refractory adductor spasms that interferes with acute rehabilitation
For refractory adductor spasms that interferes with acute rehabilitation
• For chronic pain
![]() As a diagnostic block for hip joint pain or for suspected neuropathy
As a diagnostic block for hip joint pain or for suspected neuropathy
![]() For chronic hip pain with a local anesthetic block, with or without steroids, or using radiofrequency lesioning
For chronic hip pain with a local anesthetic block, with or without steroids, or using radiofrequency lesioning
![]() For adductor spasticity as a neurolytic block. Kwon suggests that a selective blockade of the anterior branch may be sufficient to permit abduction more than 45 degrees.
For adductor spasticity as a neurolytic block. Kwon suggests that a selective blockade of the anterior branch may be sufficient to permit abduction more than 45 degrees.
• Another indication is to prevent the obturator reflex during transurethral resection of the bladder (TURB). The reflex is due to the stimulation through the bladder of the obturator nerve, resulting in sudden thigh adduction that can cause bladder perforation. Bilateral blocks have to be performed to be effective.
RELEVANT ANATOMY
• The obturator nerve is a mixed sensory and motor branch of the lumbar plexus and derives from the anterior divisions of the ventral rami of L2, L3, and L4 (Figure 63-1).
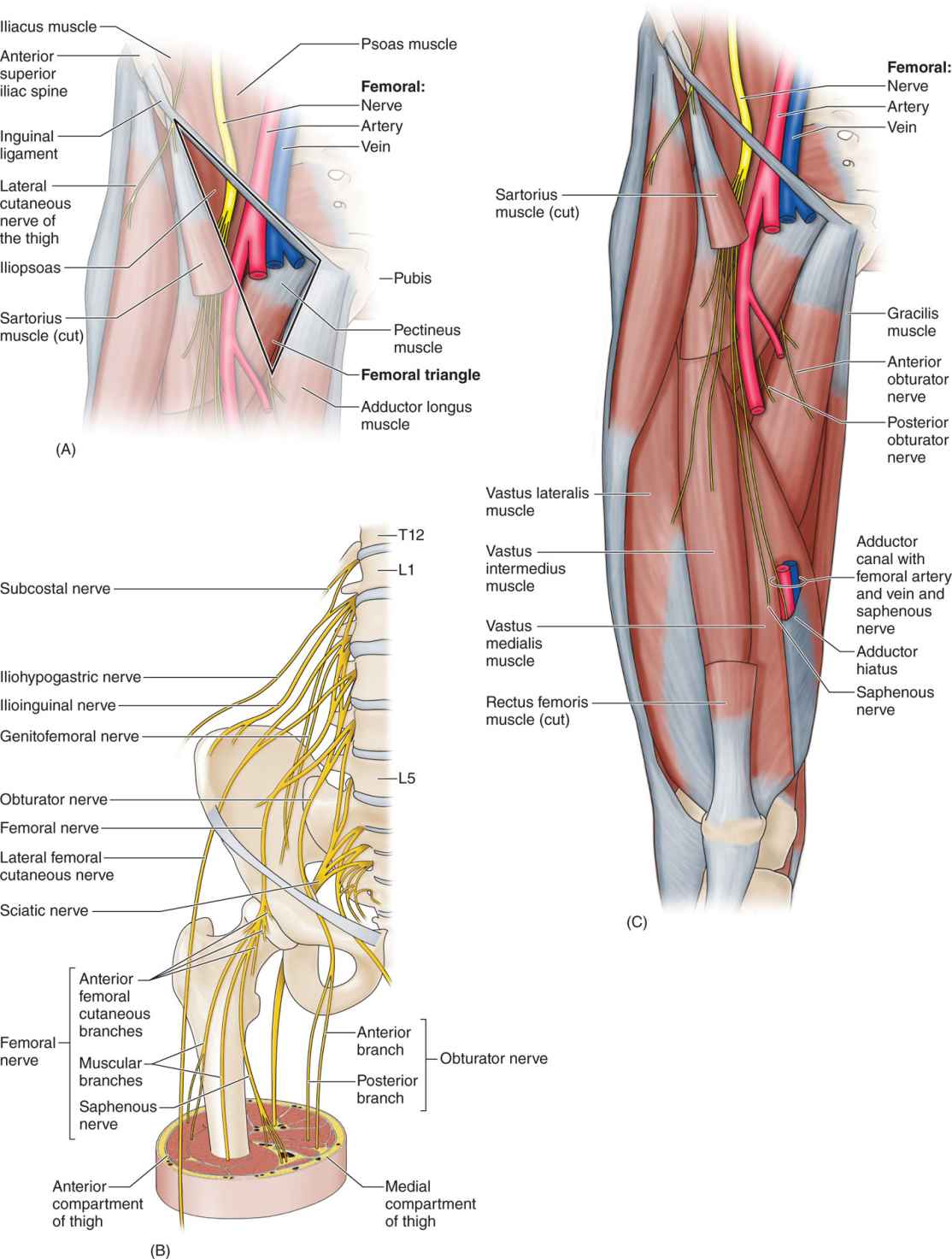
Figure 63-1. Anatomy of the obturator nerve.
• It typically emerges from the medial border of the psoas muscle at the level of the pelvic brim, and divides in the obturator canal into anterior and posterior branches (Figure 63-2), although variations are common with a multiple branching pattern.
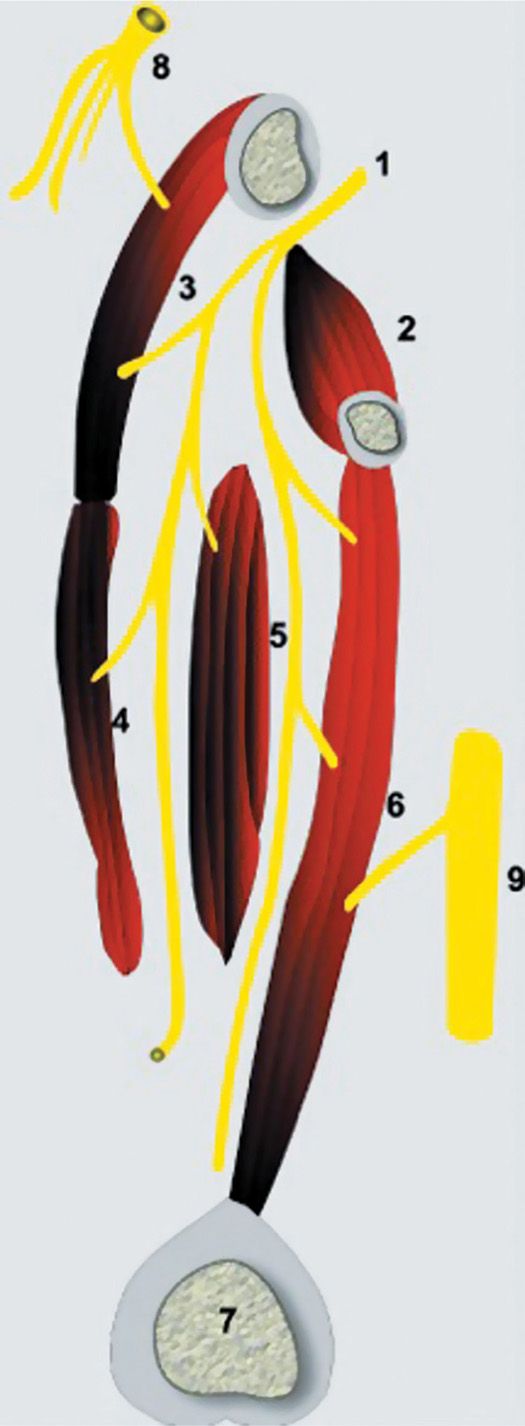
Figure 63-2. Sagittal section demonstrating the relationship of the obturator nerve to the adductor muscles. 1, obturator nerve passing through the obturator canal; 2, obturator externus; 3, pectineus; 4, adductor longus, 5, adductor brevis; 6, adductor magnus; 7, medial femoral condyle; 8, femoral nerve; 9, sciatic nerve.
• The anterior branch gives an articular branch to the hip joint (Figure 63-3), provides motor innervation of the adductor brevis, adductor longus, gracilis, and occasionally the pectineus, and innervates a variable area of skin; most references show an area in the medial aspect of the thigh, while others suggest a more distal location at the level of the knee.
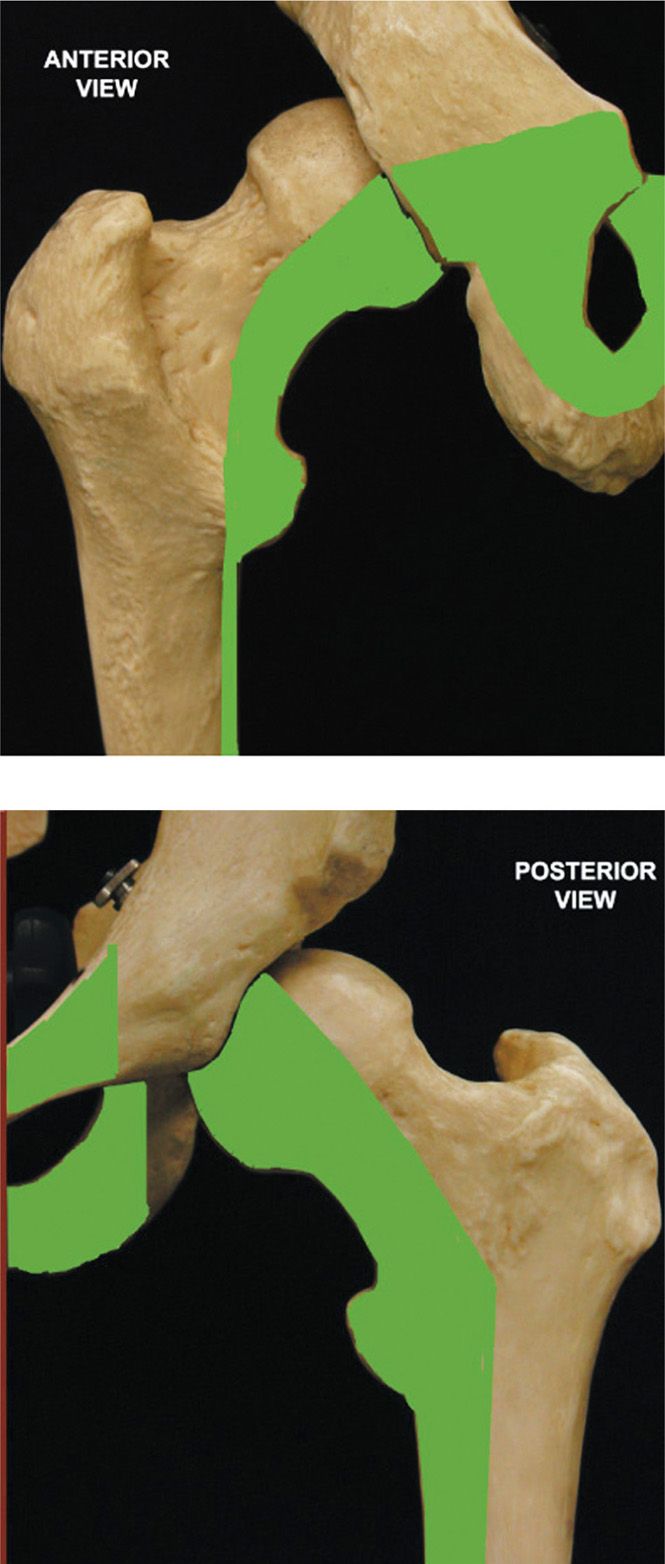
Figure 63-3. Contribution of the obturator nerve to the sensory innervation of the hip.
• The posterior branch provides motor innervation to the adductor magnus, obturator externus, and occasionally the adductor brevis (in that case, this muscle is not innervated by the anterior branch), and ends with an articular branch to the knee joint.
• The obturator nerve can be blocked with the other nerves of the lumbar plexus using the psoas compartment approach. Despite initial claims, a perivascular inguinal block (Winnie’s “3-in-1 block”) only rarely reaches the obturator nerve, as demonstrated by Macalou et al.
• The block can be performed using external anatomic landmarks and neurostimulation, or using imaging guidance (fluoroscopy or ultrasound, rarely CT scan). Blockade can be performed proximally, in the obturator foramen, before nerve division, or more distally, in the proximal thigh, between the adductor muscles.
• The anterior and posterior branches can be blocked separately at that level, as the anterior branch lies between adductor longus and adductor brevis, while the posterior branch lies between adductor brevis and adductor magnus.
BASIC CONCERNS AND CONTRAINDICATIONS
Absolute
• Patient refusal
• Inguinal lymphadenopathy (although a posterior approach would still be possible)
• Infection in the injection area or in the perineum
• Hematoma at the needle insertion site
• Systemic infection
Relative
• Preexisting obturator neuropathy (except if the block is used to diagnose such a neuropathy)
• Significant coagulopathy or anticoagulation (an ultrasound-guided block could be considered by a trained operator)
• Contrast allergy if a fluoroscopic technique is used and contrast will be administered, although premedication is feasible
• Patient unable to lie supine and achieve the desired position to be able to perform the block
PREOPERATIVE CONSIDERATIONS
• Informed consent should be obtained after thorough discussion of risks and benefits.
• Anticoagulation or coagulopathy: evaluate the risk/benefit ratio.
• Examination of the area for infection or hematoma.
• The patient should be able to lie supine.
• IV access can be considered for sedation and treatment of a possible vasovagal reaction. Vital sign monitoring can include ECG, NIBP, heart rate, and pulse oximetry.
• Resuscitation equipment and 20% intralipid can be available to treat local anesthetic toxicity.
• Position the patient supine, with the lower extremity slightly abducted, and in slight external rotation. Optimal positioning might be difficult to achieve in a spastic patient.
• Protect the genitalia and the perineum from the antiseptic solution.
Equipment
• 25-gauge 35-mm needle for skin anesthesia
• 3 or 5 mL syringe for skin anesthesia
• 10 or 20 mL syringe for medication
• 21- or 22-gauge, 50- to 80-mm nerve block needle, used with a peripheral nerve stimulator or ultrasound machine
• 22-gauge 100-mm spinal needle and fluoroscopy equipment, according to the technique used
Medications
• 1% lidocaine for skin anesthesia
• 0.0625% to 0.25% bupivacaine or 1% to 2% lidocaine or another suitable local anesthetic for nerve blockade; phenol for neurolytic block (3% phenol if only a sensory block is desired, 6% phenol to obtain a motor block as well).
Technique Using Neurostimulation
Labat’s original technique is uncomfortable for the patient, as it requires bone contact and multiple redirecting of the needle, and the needle may enter the pelvis if inserted too far. Wassef described an elegant interadductor technique, but the technique described by Choquet is preferred, as it is more distal and thus minimizes the risk of vascular injury and of entering the pelvis. One has to be aware, however, that because the nerve is blocked more distally, the branches to the hip joint might not be blocked.
• The insertion of the tendon of the long adductor muscle on the pubic tubercle is identified, using extreme leg abduction (Figure 63-4).
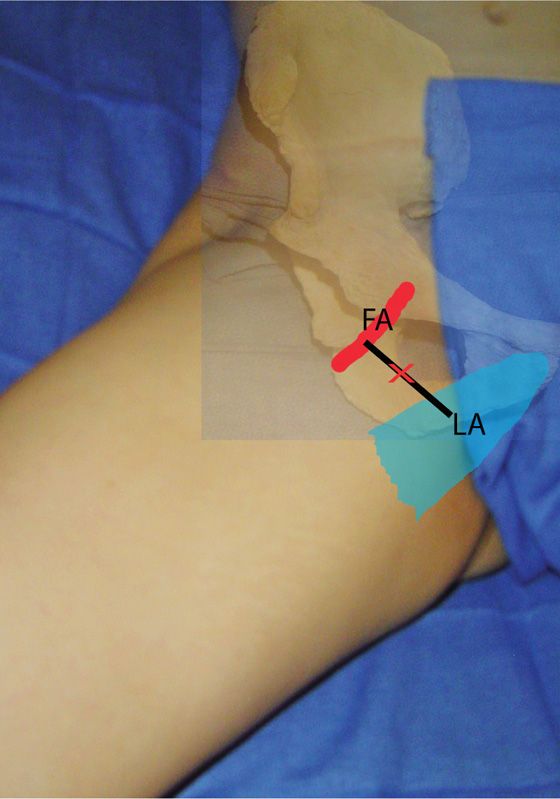
Figure 63-4. Neurostimulation technique as described by Choquet. Tendon of the long adductor muscle (LA). Pulse of the femoral artery (FA). Needle insertion site (X).
• A line is drawn, following the inguinal crease, from the pulse of the femoral artery to the tendon of the long adductor muscle.
• The needle is inserted at the midpoint of this line and directed cephalad at a 30-degree angle.
• After 3 to 5 cm in an average size patient, contractions of the long adductor and gracilis muscles can be detected on the posterior and medial aspect of the thigh.
• After the current is decreased to less than 0.4 mA and the response is preserved, 5 to 7 mL of local anesthetic are injected after aspiration.
• The needle is then redirected slightly laterally and inserted 0.5 to 1.5 cm deeper until a response from the adductor magnus muscle is obtained on the posteromedial aspect of the thigh.
• Again, the current is decreased to less than 0.4 mA and 5 to 7 mL of local anesthetic can be injected. Occasionally, the obturator nerve divides more distally, and both motor responses may be observed with a single stimulation.
• Both branches can then be blocked with a single injection.
Technique Using Ultrasound Guidance
Soong et al described the ultrasonographic imaging of the obturator nerve.
• With the patient supine and the lower extremity slightly abducted, a low-frequency ultrasound probe is placed just lateral to the tendon of the adductor longus muscle, perpendicular to the axis of the thigh.
• The muscles are identified by scanning between proximal and distal positions. The anterior and posterior branches of the obturator nerve have typically a flat and hyperechoic (ie, white) appearance (Figure 63-5).
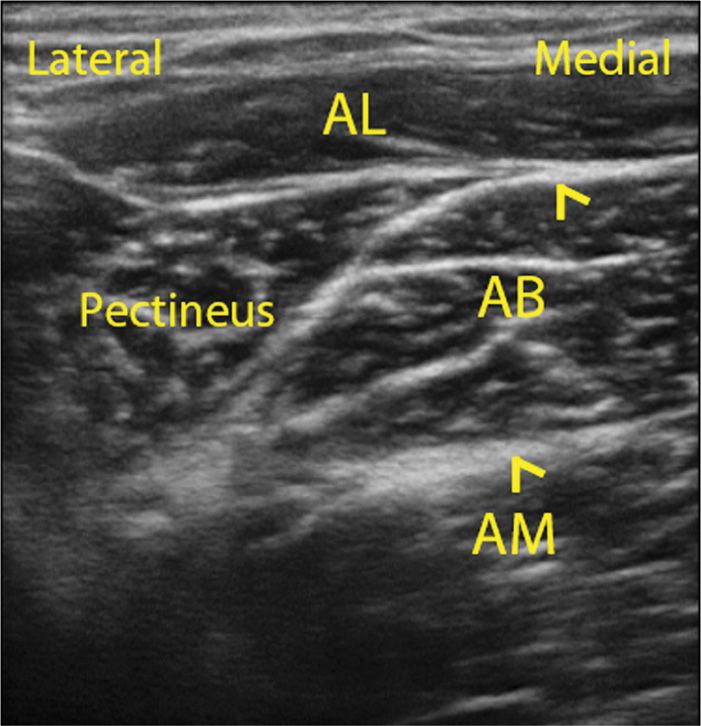
Figure 63-5. Ultrasonographic appearance of the branches of the obturator nerve. The anterior branch (A) is seen lying between, the adductor longus (AL) and the adductor brevis (AB). The posterior branch is found between the adductor brevis (AB) and the obturator externus muscle (OE).
• The anterior branch can be found between, superficially, the adductor longus or the pectineus, and the adductor brevis. The posterior branch is found between the adductor brevis and the obturator externus muscle, or, if the probe is positioned more distally, the adductor magnus muscle.
• It is useful to track the nerves up and down to confirm that they are indeed continuous structures. Color Doppler can be used to locate the obturator artery or its branches.
• The block is often performed using an out-of-plane technique, as the area is small and a needle introduced in-plane would have to go through the adductor longus tendon medially, or might threaten the femoral vessel immediately lateral to the ultrasound probe, but careful technique makes the in-plane approach possible, especially if a probe with a small footprint (“hockey-stick”) is used.
• Following negative aspiration for blood, 5 to 7 mL of local anesthetic are deposited near both nerves, although some authors recommend injecting 7 to 10 mL near one branch to block both branches by diffusion.
Akkaya described a more proximal approach, comparable to Labat’s approach but without the need for bone contact. The ultrasound probe is positioned parasagittally medial to the area where the femoral vein is visualized, at the level of the inguinal ligament.
• The superior pubic ramus is identified, and a triangular hypoechoic area bound by the superior pubic ramus superiorly, the pectineus muscle anteriorly, and the obturator externus muscle posteriorly is defined, containing the obturator nerve (hyperechoic) and the obturator vein (Dopplerable).
• A 22-gauge needle is inserted in-plane from the distal side of the probe.
• Neurostimulation is used to confirm proximity of the needle tip with the obturator nerve (adductor response with a current of >0.5 mA).
• 10 mL of local anesthetic is then slowly injected while monitoring solution spread under real-time ultrasound.
Technique Using Fluoroscopic Guidance
• Labat’s approach is typically used.
• The patient is positioned supine with the leg slightly abducted.
• A 22-gauge 100-mm needle is inserted at a point 1.5 cm caudal and lateral to the pubic tubercle, perpendicular to the skin, after raising a skin wheal with lidocaine.
• The needle is advanced until bone (the inferior pubic ramus) is contacted.
• It is then slightly withdrawn, redirected cranially and laterally, and advanced 2 to 3 cm in order to enter the obturator canal.
• Fluoroscopy is used to confirm the needle position (Figure 63-6), and 3 mL of contrast is injected for further confirmation.

Figure 63-6. Position of the needle in the obturator canal confirmed by fluoroscopy. (Reproduced with permission from Viel EJ, Perennou D, Ripart J, Pélissier J, Eledjam JJ. Neurolytic blockade of the obturator nerve for intractable spasticity of adductor thigh muscles. Eur J Pain. 2002;6(2):97-104.)
• If a stimulating needle is used, neurostimulation can be used to elicit contraction of the adductors, or to reproduce the pain sensation.
• Anterior and posterior CT-guided techniques have also been described.
POSTPROCEDURE FOLLOW-UP
• The patient must be warned of the risk of gait or standing instability and fall, as adductor muscle tone will be significantly decreased.
• Depending on the local anesthetic or phenol concentration injected, the duration of the blockade will vary from a few hours to up to a year.
POTENTIAL COMPLICATIONS AND PITFALLS
As this block is used only infrequently, no complication has, to our knowledge, been reported in the literature. This is not in itself an assurance that complications cannot happen.
• A misdirected needle could pass over the superior pubic ramus and penetrate the pelvic cavity, perforating the bladder, rectum, or spermatic cord.
• The obturator vessels travel with the nerve in the obturator canal; intravascular injection and hematoma formation are possible.
• The corona mortis, a retropubic anastomosis between the external iliac (or deep epigastric) and obturator arteries, is present in 10% to 30% of patients; bleeding secondary to laceration of the corona mortis could be difficult to control.
• As with other peripheral nerve blocks, nerve trauma or local anesthetic toxicity is also possible.
CLINICAL PEARLS
• In 8% to 30% of patients, an accessory obturator nerve arises from L3 and L4, travels with the femoral nerve and gives branches to the hip joint.
• Adductor spasm persisting after an obturator block can be due to this accessory nerve. However, among the adductor muscles, the femoral nerve usually innervates the pectineus, and a portion of the adductor magnus is innervated by the sciatic nerve.
• These might be sufficient to explain a persistent adductor tone following a well-conducted obturator nerve block.
• Adductor motor strength has been shown to be decreased by about 25% following femoral nerve blockade, and 11% following sciatic nerve blockade.

Full access? Get Clinical Tree







