Immediate Management of Life-Threatening Problems
See Table 38–1. Patients with active vaginal bleeding are at risk of exsanguination and require immediate evaluation and treatment.
|
Examine the patient for hypotension or tachycardia due to depletion of intravascular volume.
If blood pressure and pulse are normal in the supine position, measure them in the sitting position. If they are still normal, measure them in the standing position to detect more subtle volume depletion. Supine or postural hypotension can indicate life-threatening hemorrhage.
Tachycardia while the patient is resting or when she assumes the upright posture also may indicate vascular depletion.
Cool, mottled skin and delayed capillary refill may indicate significant volume loss.
(See Chapter 11) Briefly, the procedure is as follows:
Insert at least 2 large-bore (≥16-gauge) intravenous catheters. A central venous catheter may be preferable if peripheral venous access is not readily obtainable. Intraosseus access is an acceptable alternative (Chapter 8).
Determine the amount of blood loss and draw blood for (a) typing and crossmatching (reserve four units of fresh-frozen plasma and two to four units of packed red cells), (b) platelet count, prothrombin time, and partial thromboplastin time to uncover any bleeding abnormality, (c) complete blood count (CBC), (d) renal function tests and measurement of serum electrolytes, and (e) blood gas measurements and pH (useful in assessing adequacy of ventilation and perfusion).
Insert a Foley catheter.
If the patient is of child-bearing age, obtain a serum or urinary pregnancy test.
Begin rapid infusion of crystalloid solution (Ringer’s solution or normal saline), the rate depending on vital signs (eg, 200–1000 mL/h), to restore intravascular volume and maintain blood pressure until compatible blood becomes available for transfusion.
Infuse crossmatched blood as soon as possible. If the patient is unstable and crossmatched blood is unavailable, transfuse O-negative blood. Give two or more units depending on vital signs.
In the evaluation of a pregnant patient with vaginal bleeding, ultrasound can be used to rapidly identify fluid in the pelvis or abdomen (presumed to be blood in the setting of shock), which is highly suggestive of ruptured ectopic pregnancy. In the setting of symptomatic vaginal hemorrhage in the first trimester of pregnancy, ultrasound may show retained intrauterine products of conception, indicative of an incomplete spontaneous abortion. For the nonpregnant patient, an ultrasound showing significant pelvic or intraabdominal fluid may be representative of a hemorrhagic ruptured ovarian cyst, which occasionally requires surgical intervention.
The measures described here should not be used in third-trimester pregnancy.
Insert one hand in the vagina, elevate the uterus, and compress it against the abdominal wall and the opposite hand. Alternately, tamponade may be attempted by inserting a foley catheter into the uterine cavity and inflating the balloon until bleeding subsides.
Conjugated Estrogen therapy 25 mg q 4 hrs IV may be used alone, or in combination with direct compression until bleeding is controlled.
If trauma has occurred, determine the extent of injury, and apply pressure to the bleeding site.
Obtain urgent gynecologic or surgical consultation for possible emergency dilation and curettage, laparoscopy, or laparotomy in any hemodynamically unstable patient
Patients with vaginal bleeding resulting in abnormal hemodynamics or significant anemia should be hospitalized.
See Table 38–2.
| History and Symptoms | Signs | Laboratory Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Relationship to Menstrual Period | Quality of Pain | Prior Salpingitis | Type of Vaginal Discharge | Fever | Cervix | Uterus | Adnexal Mass | Adnexal Tenderness | Urine Immunologic Pregnancy Test | Leukocytosis | |
| Salpingitis | Accompanying or just after period | Constant and severe | + | Scant to purulent | + | Tender with motion | Tender | None | Usually bilateral | Indicated | ++ |
| Salpingitis plus tubo-ovarian abscess | + | Also, elevated erythrocyte sedimentation rate | |||||||||
| Incomplete abortion | Period of amenorrhea with recent spotting or frank blood | Cramping and suprapubic | ± | Heavy blood clots | − | Dilated | Enlarged, tender | None | None | ± | ± |
| Septic abortion | Thick and bloody; foulsmelling | + | Dilated, tender | Enlarged, tender | ± | Bilateral | ± | ++ | |||
| Ectopic pregnancy | Amenorrhea with recent spotting | Intermittent; variable severity | ± | Scant but rarely none | ± | Slightly tender | Normal to slightly enlarged | + | Unilateral | ± | ± |
| Ruptured ovarian cyst | Precedes period | Sudden and severe | − | None | ± | Normal | Normal | ± | Unilateral | Indicated | ± |
| Mittelschmerz | Midcycle | Sudden | − | Spotting | − | Normal | Normal | None | Unilateral | − | − |
| Torsion of ovarian tumor | None | Intermittent; radiates to thigh | − | None | ± | Slightly tender | Slightly tender | None | Unilateral | ± | − |
| Endometritis with or without IUD | Variable | Cramping | ± | Scant or none | + | Variable | Slightly tender | +if tubal abscess | Variable | ± | ± |
| Dysmenorrhea | Accompanies period | Cramping | ± | Normal menses | − | Normal | Variable tenderness | Negative | Seldom | − | − |
| Appendicitis | None | Periumbillical; cramping; progressing to constant right lower quadrant | − | None | ± | Normal | Normal | None | Unilateral | ± | ± |
Obtain information about the following points:
- Possible pregnancy (recent amenorrhea or abnormal period, intercourse without contraception, morning sickness, or tenderness of breasts of recent onset)
- History of trauma, including rape or nontherapeutic abortion
- History of salpingitis
- History of ectopic pregnancy
- Duration of symptoms and relation to menses
- Type of pain (cramping or constant)
- Type and amount of vaginal bleeding or discharge
- Use of intrauterine device (IUD)
Fever is often the first sign of infection, and pelvic warmth (from local inflammation) may be noted on bimanual examination. Pelvic organs are tender and engorged.
The white cell count, differential, and erythrocyte sedimentation rate may reflect inflammation or infection but are nonspecific tests.
A pregnancy test is important if pain or bleeding is present (Table 38–3). Qualitative tests of blood or urine are sensitive and may provide positive test results within 7 days of conception. They are also relatively inexpensive, easy to do, and can be performed in 5–10 minutes. Quantitative blood tests are more sensitive and may assist in the evaluation of gestational age.
Obtain cervical swab cultures for gonococci and Chlamydia trachomatis if infection is a possible diagnosis.
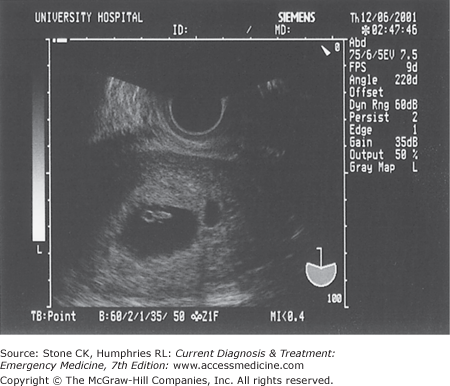
Ultrasound may show an ectopic pregnancy, intrauterine pregnancy, inflamed fallopian tubes, ovarian cysts, or pelvic abscesses (Figures 38–1 and 38–2).
Laparoscopy may be helpful when the diagnosis is uncertain.
| Clinical Findings | Possible Causes |
|---|---|
| Bleeding | Trauma Postpartum hemorrhage Dysfunctional uterine bleeding Carcinoma |
| Pain | Salpingitis and tubo-ovarian abscess Ruptured ovarian cyst Torsion of tube and ovary Mittelschmerz Abdominal disorders (appendicitis, etc.) |
| Pain and bleeding | Dysmenorrhea Endometriosis Endometritis |
| Pregnancy and bleeding | Placenta previa Ectopic pregnancy Spontaneous abortion Abruptio placentae |
| Pregnancy and pain | Ectopic pregnancy Degenerating fibroid (leiomyoma) Normal labor |
| Pregnancy with pain and bleeding | Labor with placenta previa Abruptio placentae Septic abortion Puerperal sepsis Ectopic pregnancy |
If the diagnosis is uncertain but either ectopic pregnancy or septic abortion is a possibility, consultation with a gynecologist for hospitalization or daily follow-up on an outpatient basis is mandatory.
Emergency Management of Gynecologic Disorders
- Unilateral pelvic pain in early pregnancym
- Vaginal bleeding present or absent
- Risk factor assessment
- Unilateral adnexal tenderness or mass
- Uterine size less than dates
- Quantitative human chorionic gonadotropin (hCG) and pelvic ultrasound
Ectopic pregnancy is the leading cause of pregnancy-related death in the first trimester. Patients with ectopic pregnancy are often encountered in the emergency department, and the disorder may be difficult to identify given the varied presentations that occur. Because ectopic pregnancy can be life threatening, it should be suspected in any patient presenting with amenorrhea, vaginal bleeding, and lower abdominal pain. For some women, the initial presenting symptom of an ectopic pregnancy is syncope. The most common presenting complaint is vaginal bleeding, often scant at first, with cramping lower abdominal pain.
The incidence of ectopic pregnancy is increased in women using an IUD and in those with a history of pelvic infection (eg, salpingitis), tubal surgery, infertility treatments, or previous tubal pregnancies. About 98% of ectopic pregnancies are tubal.
The clinical presentation of ectopic pregnancy is variable, ranging from the asymptomatic patient to the patient with hemorrhagic shock. Rupture of the fallopian tube followed by free intraperitoneal bleeding from tubal vessels is the principal cause of illness and death.
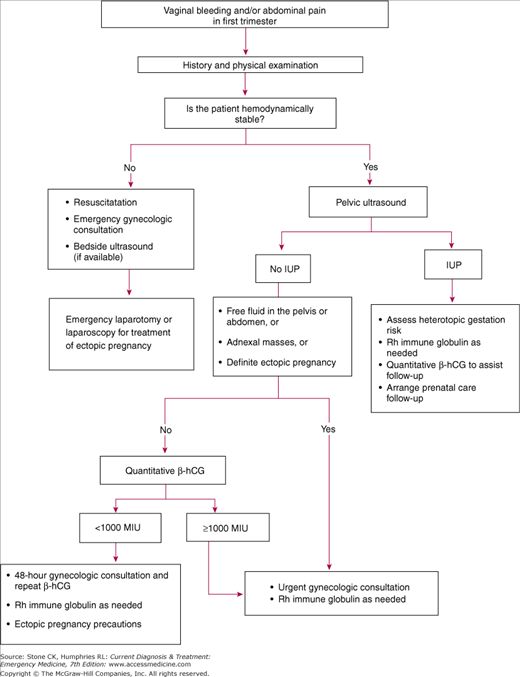
With improved resolution of ultrasound and rapidly available quantitative hCG assays, the diagnosis of ectopic pregnancy can be made more accurately and earlier than in the past (Figure 38–3).
Patients have a history of the following: (1) missed or abnormal menses or vaginal bleeding—however, 30% of patients with ectopic pregnancy have no vaginal bleeding; (2) pelvic pain, which may be unilateral, following amenorrhea; and (3) possible intermittent pain; rupture of the fallopian tube may bring temporary relief of pain.
Symptoms of early pregnancy (eg, breast tenderness and nausea) may be present. Unilateral abdominal or pelvic pain may be present. Referred shoulder pain, syncope, or lightheadedness may also occur. Peritoneal pain may develop after tubal rupture with bleeding into the peritoneum.
In the early stages of ectopic pregnancy, the results of pelvic examination may be normal. Initially, symptoms may be completely nonspecific, because the tubal pregnancy producing them may be in the early stages of development. In advanced cases, a tender adnexal mass, enlarged uterus, or blood in the peritoneal cavity (eg, doughy cul-de-sac) may occur.
Obtain complete vital signs, including supine, sitting, and standing pulse and blood pressure measurements to look for supine or orthostatic hypotension.
The qualitative urine and serum pregnancy test may be positive at levels as low as 10 mIU/mL. Check with the laboratory. The most specific and sensitive test is the serum quantitative hCG. It may detect levels as low as 5 mIU/mL depending on laboratory assay. Quantitative hCG values are invaluable in the interpretation of pelvic ultrasound in this setting. In a normal intrauterine first-trimester pregnancy, the hCG level should double about every 1.5 days.
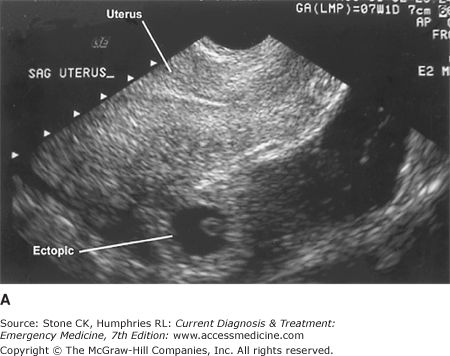
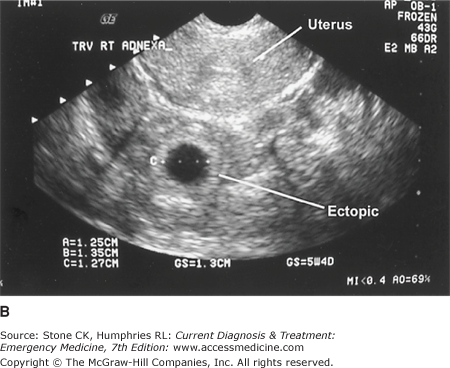
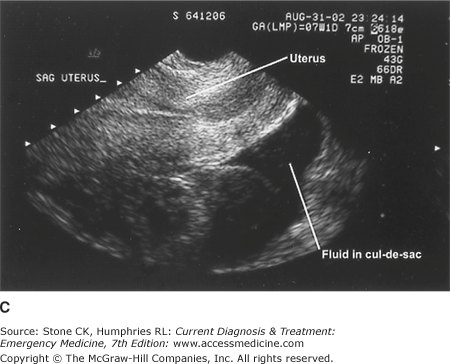
Endovaginal and transabdominal sonography have become key diagnostic tools in the differentiation of normal (see Figures 38–1 and 38–2) from abnormal early pregnancy (Figure 38–4). Occasionally, a mass can be seen in the adnexa or cul-de-sac, or products of conception can be visualized outside the uterine cavity, and ectopic pregnancy can be readily diagnosed (see Figure 38–4).
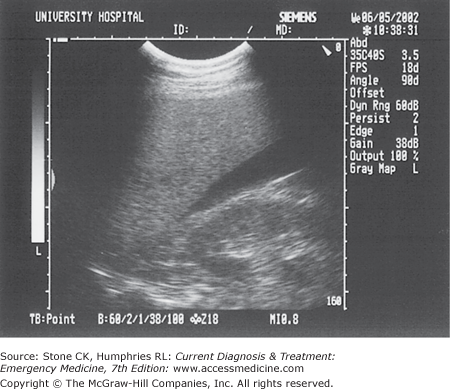
Ultrasound is often useful in excluding an ectopic pregnancy by ruling in an intrauterine pregnancy. If the patient reports a history of infertility treatments, avoid making premature conclusions because the possibility of a heterotopic pregnancy (ie, simultaneous intrauterine and ectopic) has been reported to be as low as 1 in 4000. With an hCG of 6000–6500 mIU/mL, an intrauterine pregnancy can be visualized transabdominally 94% of the time. Likewise, a yolk sac can be identified at the discriminatory hCG values of 1000–1500 mIU/mL utilizing endovaginal sonography. With endovaginal scanning, a small intrauterine collection of blood, or pseudosac, may be seen associated with an ectopic pregnancy. In very early pregnancy, at levels below the discriminatory values, the uterus may appear empty. Fluid in Morison’s pouch on transabdominal scanning strongly suggests ruptured ectopic pregnancy, usually requiring operative intervention (Figure 38–5).
Laparoscopy or laparotomy may be necessary to make a definitive diagnosis of ectopic pregnancy.
Figure 38–4.
Endovaginal ultrasound clearly demonstrating an ectopic pregnancy. A: Longitudinal view of the uterus with a well-defined endometrial stripe and no intrauterine gestational sac. A gestational sac is noted posterior to the uterus. B: Transverse view of the uterus and right adnexa also demonstrating an extrauterine gestational sac. C: Longitudinal view demonstrating free fluid in the cul-de-sac.
Treatment of possible ectopic pregnancy is determined by the patient’s risk factors for ectopic pregnancy (ie, infertility treatments, history of tubal ligation, or pelvic inflammatory disease), hemodynamic stability, and physical examination findings. Sonography is important in the evaluation of pregnant patients with either abdominal pain or vaginal bleeding (see Figure 38–3). Quantitative hCG results may help in the interpretation of ultrasound findings. In addition, Rh-negative mothers should receive Rho(D) immune globulin.
Obtain emergency pelvic sonography if hemodynamic stability allows. If the quantitative hCG value is greater than 1500–2000 mIU/mL in a patient with an empty uterine cavity on endovaginal ultrasound, ectopic pregnancy should be strongly suspected. An adnexal mass or extrauterine products of conception may or may not be readily identified. A large amount of pelvic or intraperitoneal fluid is highly suggestive of ectopic pregnancy (Figures 38–4C and 38–5). If ultrasound is unavailable for evaluation of a patient with a positive pregnancy test, physical findings worrisome for ectopic pregnancy include adnexal tenderness or an adnexal mass. However, do not be misled by a lack of peritoneal signs during your examination.
Prevent or correct hemorrhagic shock by inserting 2 large-bore (≥16-gauge) intravenous catheters and infusing crystalloid solution for volume replacement. Type and crossmatch for 2–4 units of packed red blood cells. Insert a Foley catheter, and send urine for analysis.
Obtain emergency obstetric consultation, and prepare the patient for surgery. Obtain CBC, serum electrolyte, blood urea nitrogen, creatinine, coagulation profile, and other studies as required.
Vaginal bleeding, pelvic pain, and tenderness without explanation may be present in a patient with a positive pregnancy test.
Insert an intravenous catheter, and send blood for CBC and crossmatching. Obtain pelvic sonogram. A transvaginal sonogram may not show definite evidence of an ectopic pregnancy, but worrisome signs include fluid in the cul-de-sac or an empty uterus with a quantitative hCG at or above the discriminatory zone. Urgent gynecologic consultation is recommended in these situations.
Vaginal bleeding or pelvic pain is present. The results of physical examination and laboratory studies are normal. Some authors have developed clinical criteria for prediction of ectopic pregnancy. Suggested low-risk clinical criteria (ectopic pregnancy risk <1%) for patients with pain or bleeding include absence of signs of peritoneal irritation on palpation, no cervical, adnexal, or uterine tenderness, and no abdominal or pelvic pain other than in the midline.
Send blood for quantitative hCG. If a pelvic sonogram demonstrates an intrauterine pregnancy, and the patient is at low risk for a heterotopic pregnancy (ie, no fertility medications or procedures), discharge the patient with 24–48 hours follow-up. Other patients who can be managed as outpatients with close gynecologic follow-up include those with quantitative hCG below the discriminatory zone (1000 mIU/mL) with an empty uterus and no abnormalities on endovaginal ultrasound suggestive of ectopic pregnancy. Patients with an isolated quantitative hCG below 1000 are not necessarily low risk because nearly one-third of patients with ectopic pregnancies have a quantitative hCG level below 1000 mIU/mL. A decision based only on a single hCG value below the discriminatory values lacks specificity and needs to be carefully evaluated.
Discharge the patient from the emergency department to outpatient care with a definitive follow-up appointment for reevaluation within 1–2 days. Give the patient written instructions explaining that ectopic pregnancy is a possible diagnosis and she must be alert to the following symptoms, which would require that she return to the hospital immediately: (1) increased vaginal bleeding, (2) increased pelvic or abdominal pain, or (3) syncope.
- Vaginal bleeding in early pregnancy
- Pelvic and back pain common
- Variable pelvic examination findings
- Quantitative hCG and pelvic ultrasound
- Exclude ectopic pregnancy
At least 20% of all pregnancies terminate in abortion, usually because of serious defects in the ovum. Half of abortions occur before the 8th week of gestation and another quarter before the 16th week. Many of these early spontaneous abortions go unnoticed as a delayed menstrual period. Nevertheless, early spontaneous abortions are also a common cause of visits to the emergency department.
Fetal demise and failed expulsion of the products of conception from the uterus, with a closed cervix, is termed missed abortion. If this state persists for longer than 4–6 weeks, the patient is at increased risk for infection and disseminated intravascular coagulation. Table 36–4 describes the various types of spontaneous abortion.
| Type | Symptoms and Signs |
|---|---|
| Threatened abortion | Mild, transient uterine cramps with minimal transient vaginal bleeding. |
| The cervix is long and closed. | |
| Uterine size is compatible with the presumed length of pregnancy.a | |
| Symptoms of pregnancy continue, and the conceptus remains viable | |
| Inevitable abortion | Persistent uterine cramps and moderate vaginal bleeding. |
| The cervical os is open (ie, a 0.5-cm [3/16-in] diameter sponge stick passes easily). | |
| Passage of some or all of the products of conception is inevitable or is about to occur; ie, fetal or placental tissue is found in the vagina or protrudes through the cervical os, or the patient gives a history of passage of tissue. | |
| Symptoms and signs of pregnancy disappear. | |
| Incomplete abortion | Uterine cramps and vaginal bleeding are persistent and excessive. |
| Symptoms of pregnancy may disappear. | |
| Products of conception are noted in the vagina, or the patient gives a history of passage of tissue. | |
| Complete abortion | Uterine cramps markedly diminish or stop. |
| Vaginal bleeding ceases. | |
| The entire conceptus is expelled. | |
| Symptoms of pregnancy disappear. | |
| Missed abortion | The products of conception are retained. |
| Symptoms and signs of pregnancy abate, and results of pregnancy tests change to negative. | |
| Brownish vaginal discharge (rarely, frank bleeding) occurs. | |
| Uterine cramps are rare. Examination shows a small and irregularly softened uterus. | |
| Ultrasonography fails to demonstrate a live fetus; ie, fetal heart motion is absent. |
Almost all patients have a history suggesting possible pregnancy:
- Sexual intercourse
- Period of amenorrhea or abnormal menses
- Nausea and vomiting; breast tenderness
- Uterine cramps and vaginal bleeding
- Passage of fetal or placental tissue (incomplete or complete abortion)
Caution: Pelvic examination should be performed on all patients with suspected abortion and on all pregnant patients with vaginal bleeding who have reached less than 20 weeks’ gestation. Extreme care, however, must be exercised in examining patients in the second trimester; instruments should not be introduced into the cervical os. Beyond 20 weeks’ gestation, pelvic examination should be done by an obstetrician because of the increasing risk of placenta previa.
In the first trimester of pregnancy, an hCG level that does not double in 48 hours suggests fetal demise or an abnormal pregnancy. Real-time ultrasonography, using abdominal or vaginal probes, can be diagnostic, for example, demonstrating a fetus without heartbeat or movement. Pathologic examination of tissue expelled by the uterus confirms passage of the products of conception.
Blood typing and antibody screening are required in all patients with abortion of any type. If patients are Rh-negative, give Rho(D) immune globulin (RhoGAM 300 mcg IM, many others), within 72 hours after any event in which fetal–maternal transfusion may occur, including abortion.
Advise the patient to rest. Do not use hormones, douches, or tampons. The patient should not engage in coitus. Ultrasound may reveal a gestational sac or evidence of fetal cardiac activity. Discharge instructions must include follow-up instructions and indications for return to the emergency department, including passage of fetal tissue, severe vaginal bleeding greater than one pad per hour, significant abdominal or pelvic pain, or fever. The patient should also be given adequate analgesia.
Hospitalize the patient if hypovolemia or anemia is present or if the pregnancy is past the first trimester. Treat hypovolemia if present. An obstetrical or gynecological consult should be obtained to perform possible suction curettage or dilation and curettage.
The patient may be discharged to home care if vital signs and hematocrit are stable and if vaginal bleeding is clearly decreasing. Pain must also be clearly decreasing and the cervical os closed. A physician must differentiate a complete abortion from an incomplete abortion. Several clues can help the physician determine that a complete abortion has occurred:
- A reliable history.
- Ultrasound revealing a clean uterine stripe.
- The products of conception are brought to the physician and confirmed by pathology. If pathology is not readily available, a physician can differentiate between blood clots and products of conception by rubbing the specimen between a wet gauze pad. Unlike blood clots, true products of conception will not dissolve.

Full access? Get Clinical Tree