Nonsteroidal Anti-Inflammatory Drugs in the Acute Treatment of Migraines
Peer Tfelt-Hansen
Paul Rolan
Given the widespread availability of analgesic/nonsteroidal anti-inflammatory drugs (NSAIDs) without prescription, it is likely that by the time most migraine patients consult a physician they have tried at least one of these drugs. This makes them probably the most widely used class of drugs for the acute treatment of headache and migraine, and also the class with the largest number of individual drugs. Whereas aspirin has been used for the treatment of migraine and other headaches for many years, the newer NSAIDs were introduced in migraine therapy based mainly on indirect evidence of the involvement of prostaglandins in the pathophysiology of the migraine process. However, subsequent controlled trials have demonstrated the efficacy of the NSAIDs in migraine therapy.
PHARMACOLOGIC BACKGROUND
NSAIDs possess anti-inflammatory, analgesic, and antipyretic properties. The principal types of drugs are listed in Table 49-1. Acetaminophen is included in this list despite its relative lack of anti-inflammatory activity because its action is thought otherwise to share a common central mechanism with other drugs of this class (38). They exert their effect by blocking cyclooxygenase (COX), thereby inhibiting the synthesis of prostaglandins from arachidonic acid (Fig. 49-1), but they have little or no effect on lipoxygenase and therefore no effect on the formation of leukotrienes. Both prostaglandins and leukotrienes are involved in the inflammatory process (38). Recently, it has been found that there are two forms of COX, COX-1 and COX-2. The conventional NSAIDs are generally non-selective inhibitors of both enzymes. COX-1 is widely distributed and is involved in homeostatic mechanisms. In contrast, the expression of COX-2 is markedly increased in areas of inflammation. There has been a recent flurry of development of selective COX-2 inhibitors on the hypothesis that these drugs will be as effective as the nonselective inhibitors but may be safer, and is discussed in this chapter.
Prostaglandins are associated with the development of pain that accompanies injury or inflammation. The NSAIDs, which inhibit the synthesis of these prostaglandins, are usually classed as mild peripheral analgesics, and a consideration of the type of pain that they suppress is important. They are particularly effective in settings in which inflammation has caused sensitization of pain receptors to normally pain-free mechanical or chemical stimuli. This sensitization appears to result from a lowering of the threshold of the polymodal nociceptor situated on C fibers (38). Although generally described as peripherally acting analgesics, an additional inhibitory effect on the central nociceptive system also may be responsible for their analgesic effect (6,7,47). The mode of action of the central effect of NSAIDs is unknown, but possible relevant effects include the following (6,10):
1. inhibition by NSAIDs of prostaglandin synthesis in brain neurons;
2. prolongation of catecholamine and serotonin turnover in brain neurons; and
3. blockade of the release of serotonin in response to noxious stimuli.
NSAIDs also inhibit platelet COX with consequent inhibition of the formation of thromboxane A2, a potent aggregating agent. The NSAID can either bind reversibly to this enzyme or, as in the case of aspirin, for the life of the platelet from acetylation (8 to 11 days) (38). This effect on platelets can sometimes result in a prolonged bleeding time.
TABLE 49-1 NSAIDs Evaluated as Acute Migraine Treatments | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Possible Mode of Action in Migraine
A role for prostaglandins in migraine genesis was examined by infusion of the two vasodilating prostaglandins prostaglandin E1 (4,9) and prostacyclin (25,64) to either healthy volunteers or migraine sufferers. Although the infusions induced flushing and a vascular headache, the headache resembled migrainous symptoms in only a few patients (64). Furthermore, intravenous infusion of prostacyclin to eight migraine patients induced only one migraine-like headache, and in two subjects given the infusion after a migraine attack had started, only a short-lived worsening occurred, suggesting that vasodilating prostaglandins were not the sole mediators of vascular headache in these patients (64). Another possible mechanism for the efficacy of NSAIDs in migraine prophylaxis is based on their effect in opposing the suggested hyperaggre-gability of platelets in migraine. However, neither mechanism is currently thought to be central in migraine genesis, and their efficacy may be a result of inhibition on the sterile inflammatory process caused by neurogenic vascular inflammation (8; see Chapter 33). However, the relatively poor efficacy of indomethacin in migraine (68) might be taken as evidence against this possibility. Another possible explanation for the beneficial effects of aspirin and NSAIDs in the treatment of migraine attacks is their analgesic effect or more specific effects on the trigeminal (44) and antinociceptive (28) systems in the brainstem and thalamus (40).
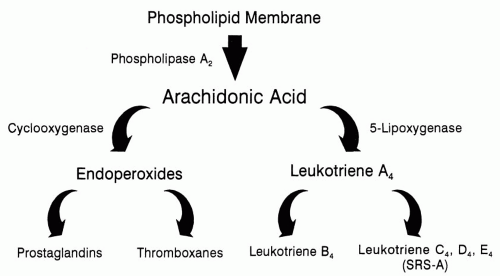 FIGURE 49-1. Principal metabolic pathways of arachidonic acid. NSAIDs block COX, thereby inhibiting the synthesis of prostaglandins from arachidonic acid, but have little or no effect on lipoxygenase and therefore no effect on the formation of leukotrienes (31). |
Pharmacokinetics, Route of Administration, and Role of Formulation
In the treatment of migraine attacks the important pharmacokinetic consideration is the speed of absorption. NSAIDs are generally well-absorbed after oral administration with a time-to-peak plasma concentration (tmax) of less than 2 hours (38). However, gastric stasis in migraine has been shown to slow the rate of drug absorption (81). Some NSAIDs have been reformulated as more soluble salts to speed absorption (e.g., lysine aspirin salt, diclofenac-K, naproxen sodium) or as encapsulated liquid preparations (e.g., ibuprofen liquigels, diclofenac softgel). An alternative strategy is to use a prokinetic/antiemetic drug such as metoclopramide (see Chapter 52). Unfortunately, there are few data available that directly compare the pharmacokinetics of these new formulations with conventional formulations during a migraine attack, probably because of the difficulty in undertaking such studies. Thus, the majority of such information comes from healthy volunteers. Nevertheless, it seems appropriate to choose the most rapidly absorbed formulation of each active ingredient. Aspirin is absorbed very quickly, with a tmax of less
than half an hour, and is metabolized quickly to salicylic acid (38,70). Naproxen sodium has a tmax of 1 hour, and naproxen has a tmax of 2 hours (38,59).
than half an hour, and is metabolized quickly to salicylic acid (38,70). Naproxen sodium has a tmax of 1 hour, and naproxen has a tmax of 2 hours (38,59).
For patients with early vomiting during the attack or prominent nausea, a nonoral route many be preferable. A suppository formulation is available for diclofenac. Ketorolac is given intravenously or as an intramuscular injection with a tmax of 45 to 60 minutes (27).
RESULTS OF RANDOMIZED CONTROLLED CLINICAL TRIALS
Placebo-Controlled Trials
A summary of 38 placebo-controlled double-blind randomized trials on the efficacy of NSAIDs or their combinations with either metoclopramide or caffeine in the treatment of migraine attacks are given in Table 49-2. The size of the trials varied from a small crossover trial with only 20 patients to several trials with parallel group design with more than 100 evaluable patients in each treatment group with the bulk of the later trials being larger and apparently adequately powered. Except for five trials (37,41,51,55,77), in which only migraine patients without aura were included, the trials included a mixture of patients suffering from migraine both with and without aura. The crossover design, which causes few problems in trials concerning treatment of the acute attacks, was used in 24 of 38 trials. As indicated in Table 49-1, NSAIDs have been found to have some efficacy in the acute therapy of migraine.
Aspirin, 500 to 1000 mg, was superior to placebo in 13 trials, 1 of which evaluated the intravenous route (20). Aspirin plus metoclopramide was not superior to aspirin in one trial (77) despite improved absorption of aspirin with metoclopramide in migraine having been demonstrated (81). Highly soluble aspirin salts (equivalent to 900 mg) combined with 10 mg metoclopramide were superior to placebo in five trials (11,37,49,54,76) and in one trial were comparable with 100 mg sumatriptan (76). Intravenous aspirin was less effective but better tolerated than subcutaneous sumatriptan (20). For a combination of 600 mg aspirin plus 400 mg acetaminophen and 200 mg caffeine, a therapeutic gain of 26% (95% confidence interval [CI] 21 to 31%) was found in three trials (53), but it should be noted that patients with the most severe migraine attacks were excluded from these trials.
Acetaminophen combined with metoclopramide was superior to placebo in one trial (17), whereas 650 mg acetaminophen alone was no better than placebo (18). A combination of 400 mg acetaminophen and 25 mg codeine was found to be superior to placebo (5).
Tolfenamic acid 200 mg was shown in three trials to be more effective than placebo (34,60,79), and in one of these (60), a rapid-release form was comparable with 100 mg sumatriptan. In a larger trial sumatriptan 100 mg was superior to rapid-release tolfenamic acid (Tfelt-Hansen, personal communication). In one of the other trials (34), tolfenamic acid was comparable with 500 mg aspirin and 1 mg ergotamine, with fewer side effects than ergotamine. In a small crossover trial (n = 10) (32), the addition of caffeine to tolfenamic acid was found to be superior to the addition of pyridoxine to tolfenamic acid, but in a larger double-blind crossover trial (n = 49), the effect of the addition of caffeine to tolfenamic acid was not superior to that of tolfenamic acid alone (79). In contrast, the addition of metoclopramide to tolfenamic acid was significantly, if marginally, better than tolfenamic acid alone (79).
Naproxen was shown to be superior to placebo in one trial (61), whereas in another similar trial the effect of naproxen was only superior to placebo after 2 hours, but not for the whole attack (2). Naproxen sodium, which, because of quicker absorption of the naproxen molecule, should be more suitable than naproxen per se (see Pharmacokinetics section), was superior to placebo in one trial (39).
Ibuprofen 800 to 1,200 mg or 400 mg as an arginine salt was more effective than placebo in three trials (36,47,71). Lower doses as a liquigel formulation (200 to 600 mg) were also found to be effective (45), as were 200 and 400 mg of a conventional formulation (13). In both low-dose trials, there was a trend for 200 mg to be less effective by a small margin. In one trial in children, ibuprofen and acetaminophen were comparable, and both were superior to placebo (35). In another, 7.5 mg/kg was found to effective, but only in boys (52).
Diclofenac as an enteric-coated tablet of 50 mg was found to be of marginal efficacy (55). The more rapidly absorbed potassium salt was evaluated in several trials (12,14,24,57,) as well as a sodium salt softgel formulation (66). Both tested doses of 50 and 100 mg were superior to placebo. In one placebo-controlled trial, diclofenac-K was superior to caffeine and ergotamine tartrate (Cafer-got) (12) and placebo; whereas in another trial diclofenac and Cafergot were equally effective (57). There appeared to be no increase in efficacy with 50 mg compared to 100 mg (14,24), but caffeine 100 mg enhanced the efficacy of the diclofenac sodium softgel 100 mg (66). Sumatriptan 100 mg orally was of similar efficacy to diclofenac sodium softgel 100 mg but was associated with more adverse effects (66). Intramuscular diclofenac (16) was superior to placebo, and although not directly compared with an oral formulation, appeared to give better efficacy (16).

Full access? Get Clinical Tree








