Rocking Bed and Pneumobelt
The rocking bed and pneumobelt are noninvasive ventilators that were developed and saw their greatest use during the latter years of the polio epidemics but are used rarely today. They both rely on the effect of gravity to assist diaphragmatic motion and are particularly well suited to patients with severe diaphragmatic weakness or paralysis. Neither one should be used in the management of acute respiratory failure, and both have limited present-day applicability. Despite the similarities, there are also important differences, such as portability and suitability for nocturnal versus daytime use. This chapter reviews the historical development, mechanisms of action, and present-day uses of the rocking bed and pneumobelt. Glossopharyngeal breathing, another noninvasive approach to ventilator assistance, is discussed briefly at the end of the chapter.
The conceptual groundwork for development of the rocking bed was laid during the early 1930s by Eve,1 who described the use of manual rocking to assist ventilation in two patients with acute respiratory paralysis. The technique consisted of placing the patient supine on a stretcher that was pivoted on a fulcrum placed at waist level. The patient then was rocked up and down approximately 45 degrees in either direction. Eve noted that the “weight of the viscera pushed the flaccid diaphragm alternatively up and down,” achieving artificial respiration.1 The technique was adopted subsequently by the British Navy as the recommended means of resuscitation for drowning victims.2 Later studies demonstrated that this tilting method compared quite favorably with other resuscitation methods of the day, and it remained an acceptable means of resuscitation until mouth-to-mouth resuscitation gained acceptance during the 1960s.3,4
Automatic rocking beds were first introduced as ventilatory aids during the late 1940s. Wright5 was the first to describe the management of respiratory insufficiency using an oscillating bed that had been designed originally to assist circulation. This experience led to the development of the McKesson Respiraid rocking bed, which was accepted by the Council on Physical Medicine and Rehabilitation in 1950.6 Intended mainly as an aid to weaning patients with poliomyelitis from dependence on the tank respirator,7 it facilitated nursing care and enhanced patient freedom but was quite noisy, bulky, and heavy (455 kg).6,7 The Emerson rocking bed (J. H. Emerson Co., Cambridge, MA), also introduced during the late 1940s, was quieter and lighter than the McKesson bed and became the dominant model during the 1950s. Hundreds of rocking beds were manufactured between 1950 and 1960 (Emerson JH, personal communication), but after introduction of the Salk and Sabin vaccines and control of the polio epidemics, demand fell drastically. Many survivors of the polio epidemics continued to use rocking beds for ventilator support, sometimes for decades,8 but most have since died or switched to other ventilators, and present-day use is rare.
The intermittent abdominal pressure respirator or insufflator (pneumobelt) was introduced at the end of the polio epidemics in an attempt to address the limitations of existing ventilators.9 The pneumobelt was designed to allow complete freedom of the upper extremities and mouth during use in the sitting position and was intended mainly as a daytime ventilatory aid during meals or wheelchair use. Several modifications of the pneumobelt have been reported since the original description, but these never gained wide acceptance. These modifications include a piston-like device that compresses the abdomen while the patient sits in a wheelchair10 and a combination of the pneumobelt and intermittent positive-pressure breathing.11 Like the rocking bed, the pneumobelt has seen only limited use since control of the polio epidemics.
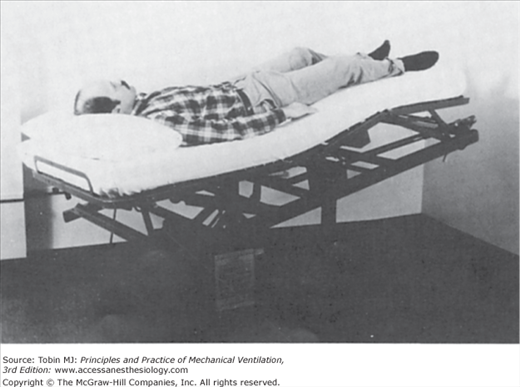
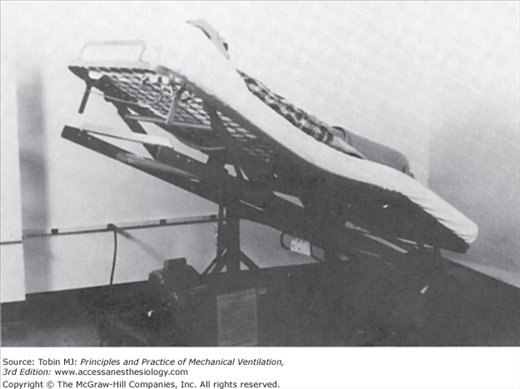
Eve compared the rocking-induced motion of the abdominal viscera within the thorax with that of a piston within a cylinder.1 As the head moves down, the viscera and diaphragm slide cephalad, assisting exhalation (Fig. 17-1). In the foot-down position, the abdominal contents and diaphragm slide caudad, assisting inhalation (Fig. 17-2).
Figure 17-2
Rocking bed in 27-degree foot-down position. Sliding of the abdominal viscera and diaphragm caudad assists inhalation. (Used, with permission, from Hill.17)
A number of early studies on the efficacy of rocking compared it as a method of resuscitation with others then used commonly.3,4 These studies used fresh corpses or live subjects with pharmacologically induced paralysis or voluntarily suspended respirations to show that rocking produced tidal volumes ranging from a few hundred milliliters to a liter, and success in the resuscitation of near-drowning victims was reported.2 Later, Plum and Whedon12 found that the automatic rocking bed was not as effective as the tank respirator but produced adequate alveolar ventilation in eleven convalescent patients with respiratory paralysis secondary to poliomyelitis. The bed, however, was unable to sustain adequate ventilation in five patients during the acute stages of respiratory paralysis. Plum and Whedon recommended that use of the rocking bed be reserved for stable patients who are capable of at least some spontaneous breathing, a recommendation that holds true today.
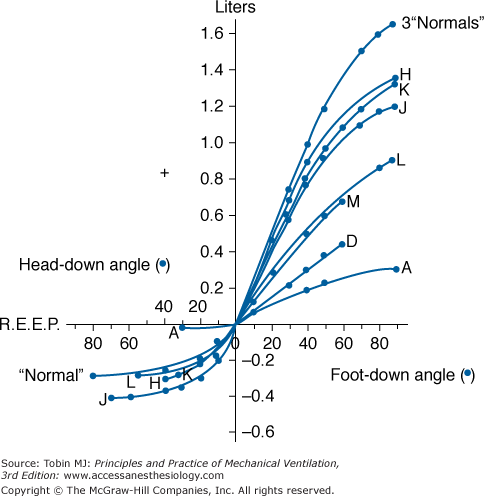
Colville et al13 subsequently examined the physiologic effects of rocking on respiratory mechanics and identified factors responsible for the wide individual variations in tidal volumes generated during rocking. They found that the greatest displacement of the diaphragm occurred during rocking from horizontal to the 40-degree foot-down position (Fig. 17-3). Beyond this angle, relatively little further displacement of the diaphragm occurred. Likewise, relatively little displacement of the diaphragm occurred during rocking from the horizontal to the head-down position. This indicated that in the horizontal position, the resting diaphragm was fairly close to its uppermost position, so the greatest passive motion could be achieved by applying gravitational force in the caudad direction.
Figure 17-3
Relationship between angle of rocking bed and static lung volume in three normal individuals and in patients with poliomyelitis, as indicated by letters. Note that the greatest volume shift occurs between 0 degrees and the 40-degree foot-down angle. Note also the marked variability between individuals. REEP, resting end-expiratory position. (Used, with permission, from Colville P, et al. Effects of body tilting on respiratory mechanics. J Appl Physiol. 1956;9:19–24.)
Along these lines, Joos et al14 found that tidal volumes were greater in some patients when rocking was achieved entirely in the head-up position (5 to 42 degrees above the horizontal plane) rather than between the head-down and head-up positions (10 degrees below to 27 degrees above the horizontal plane). In addition, others found that relatively little increase in minute volume could be achieved by increasing the rate of rocking beyond 15 to 16 rocks per minute.3 At higher rocking frequencies, the tidal volume tended to diminish, negating the effects of the increased rocking rate.
With regard to the large individual variation (see Fig. 17-3), Colville et al13 found that as the compliance of the abdominal wall increased, the greater was the tidal volume during rocking. Thus, rocking was relatively ineffective in patients with severe kyphoscoliosis, who have low abdominal and diaphragmatic compliance and short abdominal lengths. Taken together, these findings indicate that the efficacy of the rocking bed is highly dependent on patient body characteristics and that function is likely to be optimal when rocking is between the near-horizontal and the 40-degree foot-down positions at rocking rates between 12 and 16 rocks per minute. Wider manipulations of rocking rate and arc, however, may be useful in optimizing alveolar ventilation in some patients.
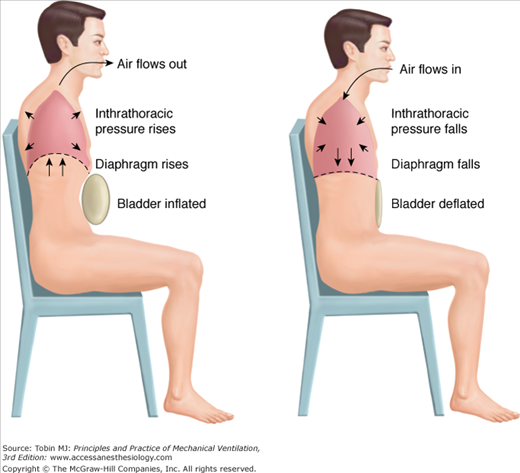
The pneumobelt9 operates by a mechanism similar to that of the rocking bed in that it assists diaphragmatic motion by causing piston-like motions of the abdominal viscera within the thoracic “cylinder.” The major difference is that the pneumobelt assists exhalation by applying positive pressure to the abdominal surface rather than using gravitational force. It consists of an inflatable rubber bladder held firmly over the abdomen by an adjustable corset (Fig. 17-4). Inflation of the bladder squeezes the viscera, forcing the diaphragm cephalad and actively assisting exhalation. On deflation of the bladder, gravity pulls the viscera and diaphragm back to their original positions, assisting inhalation (Fig. 17-5). Because of this dependence on gravitational force, the pneumobelt must be used in a sitting position, optimally at angles of 45 degrees or greater. Below 30 degrees, the ability to assist ventilation is diminished markedly. Thus, nocturnal use of the pneumobelt is limited to patients who can sleep in a sitting position.15
Figure 17-5
The pneumobelt functions by exerting positive pressure on the abdominal viscera, forcing the diaphragm up and assisting exhalation (left). When the bladder deflates, gravity returns the diaphragm to its original position, assisting inhalation (right). (Reproduced with the permission from the American College of Chest Physicians. Hill NS. Clinical applications of body ventilators. Chest. 1986;90:897–905.)
Despite this limitation, the pneumobelt can be a very useful device in appropriately selected patients. The ability of the pneumobelt to augment tidal volume is linearly related to the inflation pressure of the bladder between pressures of approximately 15 and 50 cm H2O. Pressures exceeding 50 cm H2O are rarely tolerated because of abdominal discomfort. As with the rocking bed, the ability of the device to augment tidal volume varies considerably among individuals. Important factors that contribute to the variability among individuals include abdominal and chest wall compliances. High abdominal compliance favors efficient functioning of the device, but high chest wall compliance may allow expansion of the chest wall during bladder inflation, reducing efficiency.9 Thus, like the rocking bed, body habitus is also an important determinant of ventilator efficiency for the pneumobelt. Although thin patients can be ventilated effectively,16 both devices work less efficiently in extremely thin or obese patients and in those with severe kyphoscoliosis. The sitting position in patients with severe kyphoscoliosis often brings the lower rib cage in contact with the thighs, rendering proper positioning of the pneumobelt impossible.
Rocking beds are no longer available commercially. Pneumobelts (small, medium, or large) can be obtained via home medical equipment vendors via Philips Respironics, Inc. (Murrysville, PA). Positive-pressure volume-limited ventilators with sufficient pressure-generating and volume-generating capabilities can be used. Most portable “bilevel” positive-pressure devices, however, are insufficient.
Consisting of a bed frame that is suspended on an axis 100 cm above the ground, rocking beds are bulky (193 cm long by 84 cm wide) and heavy (approximately 136 kg). Although the axis of rotation can be adjusted, they usually are set to rotate 10 degrees in the head-down direction and 27 degrees foot-down. As noted previously, maintaining the rocking arc in the head-up range may improve efficacy in some patients.14 Adjustable cranks allow raising of the head and knees to minimize slippage. Excessive flexion of the hips, however, may impair functioning.14 A foot rest also may be attached to prevent downward sliding, but with proper positioning of the head and knees, this is usually unnecessary.
The most attractive feature of the rocking bed is its ease of application. With use of a foot stool, most patients can position themselves on it with minimal assistance. Paralyzed patients require help from one or two attendants depending on body weight. The patient lies supine with the head and knees raised slightly to maximize comfort. A baseline minute volume is measured using a portable spirometer. Rocking then is commenced at rates between 12 and 16 rocks per minute, again adjusted to optimize patient comfort. The patient is coached to exhale during head-down rocking and to inhale while the head moves up. When synchronization has been achieved, further adjustments in rocking rate may be made to optimize minute volume. An arterial blood-gas determination may be helpful after an hour or two during the initial trial to assess adequacy of alveolar ventilation.
Patients then are encouraged to initiate rocking at bedtime and to extend the hours of use gradually until they are able to sleep through the night. Most patients find the rocking bed quite comfortable and encounter little difficulty in learning to sleep while rocking. Motion sickness is unusual, presumably because the bed rocks in one plane only, but it may disturb some patients. The bed limits daytime mobility, so most patients use it only nocturnally. If daytime ventilatory assistance is necessary, another technique, such as noninvasive positive pressure ventilation or the pneumobelt, is recommended for daytime supplementation.
Application of the pneumobelt is slightly more difficult than that of the rocking bed, usually requiring at least one attendant unless the patient has full upper extremity strength. The corset is positioned while the patient is sitting comfortably. The rubber bladder is positioned over the abdomen with the curved lower border of the corset over the pubis and the horizontal upper border over the xiphoid. Some coverage of the lower rib cage may serve to minimize paradoxical motion of the ribs during assisted exhalation, although some authors have found more efficient functioning if the corset is placed below the xiphoid.16

Full access? Get Clinical Tree