Nonadrenergic Vasopressors in ECC
Helmut Raab
Martin Dünser
Volker Wenzel
It had been axiomatic that increased vasoconstriction during CPR improves coronary perfusion pressure and thereby immediate resuscitation success; however, data indicates that vasoconstriction can be excessive. Postresuscitation left ventricular dysfunction is well documented and is a difficult-to-manage problem in the intensive care unit. Accordingly, the stunned left ventricle may be unable to tolerate the increased systemic vascular resistance immediately after resuscitation; therefore, heart failure and malignant ventricular arrhythmias may occur.
There is long-standing concern that administration of epinephrine during resuscitation may result in detrimental effects during the postresuscitation period.
Nonadrenergic vasoactive peptides such as arginine vasopressin hold promise, since they may raise perfusion pressure without the beta-receptor–mediated side effects of adrenergic vasopressors.
A better knowledge of nonadrenergic vasopressors, their underlying mechanisms of action, and their usage in critically ill patients has the potential to save many lives.
Nonadrenergic Pressors
There is a long-standing concern that administration of epinephrine during resuscitation may result in detrimental effects during the postresuscitation period. For example, laboratory studies employing epinephrine during cardiopulmonary resuscitation (CPR) showed increased myocardial oxygen consumption,1 ventricular arrhythmias,2 ventilation–perfusion defects,3 and postresuscitation myocardial dysfunction.4 Therefore, nonadrenergic vasoactive peptides such as arginine vasopressin hold considerable promise, since they may raise perfusion pressure without the beta-receptor–mediated side effects of adrenergic vasopressors. Another intriguing possibility is that they may act synergistically when administered together with catecholamines, and that concomitant use of adrenergic drugs and nonadrenergic vasoactive peptides may allow lowering of the dosage of each agent.
Arginine Vasopressin as an Endogenous Stress Hormone
A number of fundamental endocrine responses of the human body to cardiac arrest and CPR have been investigated5,6,7,8 and are summarized by Gazmuri (see Chapter 26). Circulating endogenous arginine vasopressin concentrations were found to be high in patients undergoing CPR. In addition, vasopressin levels in successfully resuscitated patients have been shown to be significantly higher than in patients who died.5 This may indicate that the human body discharges arginine vasopressin as an adjunct endogenous vasopressor to epinephrine in life-threatening situations such as cardiac arrest in order to preserve homeostasis. In a clinical study of 60 out-of-hospital cardiac arrest patients, parallel increases in plasma arginine vasopressin and endothelin during CPR were found only in surviving patients.6 Thus, plasma concentrations of arginine vasopressin may have a more important effect on CPR outcome than previously thought. These observations prompted several investigations to assess the role of arginine vasopressin in the management of CPR in order to improve patient outcome.
The Physiology of Arginine Vasopressin
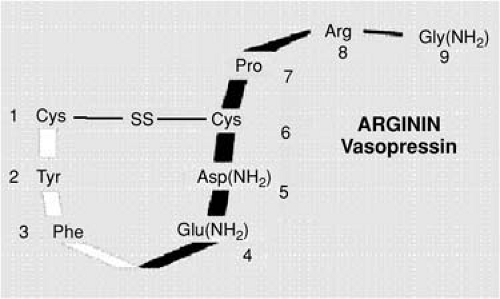
Arginine vasopressin is a nonapeptide, an endogenous hormone with osmoregulatory, vasopressor, hemostatic, endocrinologic, thermoregulatory, and central nervous effects (Fig. 27-1). The hormone is produced in the magnocellular and parvocellular nuclei of the hypothalamus and stored in neurosecretory vesicles of the neurohypophysis.9 It is secreted upon osmotic, hemodynamic, and
endocrinologic stimuli. While only 10% to 20% of the total hormonal pool of arginine vasopressin in the neurohypophysis can be readily released, the time from synthesis to secretion into the circulation is ∼1.5 hours.10 Once released, the plasma half-life of arginine vasopressin is 4 to 20 minutes. Dose-dependent clearance occurs through arginine vasopressinases in the liver and the kidneys.11,12,13
endocrinologic stimuli. While only 10% to 20% of the total hormonal pool of arginine vasopressin in the neurohypophysis can be readily released, the time from synthesis to secretion into the circulation is ∼1.5 hours.10 Once released, the plasma half-life of arginine vasopressin is 4 to 20 minutes. Dose-dependent clearance occurs through arginine vasopressinases in the liver and the kidneys.11,12,13
The most important signals for the secretion of arginine vasopressin are increased plasma osmolality, decreased arterial pressure, and reduced cardiac filling.
The most important signals for the secretion of arginine vasopressin are increased plasma osmolality, decreased arterial pressure, and reduced cardiac filling.14 Any reduction in blood volume or venous return stimulates the secretion of arginine vasopressin via activation of stretch receptors located in the left atrium and pulmonary arteries (Gauer–Henry reflex). Activation of baroreceptors in the aortic arch and carotid sinus further augments such secretion via the glossopharyngeal and vagal nerves. Baroreceptor stimulation is the primary and most important mechanism for arginine vasopressin release in hypotensive states and cardiac arrest.15 In acute hypotension, there is an exponential relationship between plasma levels of arginine vasopressin and the decrease in arterial blood pressure. Whereas small reductions in blood pressure (∼5%–10% from baseline) usually have only minor or no effect on plasma levels of arginine vasopressin, a 20% to 30% decline in arterial pressure results in concentrations of arginine vasopressin that are severalfold higher.16 Similarly, unless blood volume decreases by >10% and results in diminished arterial blood pressure, volume depletion produces little elevation in plasma levels of arginine vasopressin.17 However, the secretion of arginine vasopressin can also be directly stimulated by hypoxia, endotoxin, low concentrations of norepinephrine and angiotensin, or hypoglycemia.18
Arginine Vasopressin and its Pharmacologic Effects
Peripheral effects of arginine vasopressin are mediated by different arginine vasopressin receptors; namely V1a, V1b, and V2 arginine vasopressin receptors. V1a receptors are located on smooth muscle cells in arterial blood vessels and induce vasoconstriction by an increase in cytoplasmic ionized calcium via the phosphatidyl-inositol-bisphosphonate cascade.19 On a molar basis, arginine vasopressin was shown to be a severalfold more potent vasoconstrictor than norepinephrine and angiotensin II.20 In contrast to those of catecholamine-mediated vasoconstriction, the effects of arginine vasopressin are preserved during hypoxia and severe acidosis.21
Arginine vasopressin–mediated vascular effects differ substantially within particular vascular beds.
However, arginine vasopressin–mediated vascular effects differ substantially within particular vascular beds. Physiologically, most arterial beds exhibit vasoconstriction in response to arginine vasopressin.22,23 Vasopressor effects are strongest in the muscular, adipose, cutaneous, and probably also the splanchnic vasculature. In a porcine CPR model, Voelckel et al.24 found a significantly lower blood flow in the superior mesenteric artery in pigs resuscitated with arginine vasopressin when compared to epinephrine; there were no differences in hepatic or renal blood flow. Like oxytocin-mediated paradoxical vasodilatation of vascular smooth muscle, vasodilatation after arginine vasopressin has been described not only in the pulmonary, coronary, and vertebrobasilar circulation but, interestingly, also in the mesenteric vascular bed, suggesting a dose-dependent response.25,26,27,28 The underlying mechanisms for such an arginine vasopressin–mediated vasodilatation seem to be nitric oxide–dependent.26 Russ and Walker reported that stimulation of V1 receptors can release nitric oxide, presumably from the endothelium of some vascular regions.29 Recently, there is increasing evidence of hemodynamically relevant V1 receptors on cardiomyocytes. In vitro and animal experiments have demonstrated an increase of intracellular calcium concentration and inotropy after stimulation of myocardial V1 receptors.30,31
In the kidney, V2 receptors are located on distal tubules and collecting ducts. Upon stimulation, they facilitate integration of aquaporines into the luminal cell membrane of the collecting ducts, leading to increased resorption of free water via an adenylate cyclase–dependent mechanism.32 Despite the antidiuretic effect of a continuous infusion of arginine vasopressin, a paradoxical increase of urine output has been reported in patients with advanced vasodilatory shock.33,34,35 It is hypothesized that together with increased renal perfusion pressure, arginine vasopressin selectively constricts efferent glomerular arterioles whereas it dilates
afferent vessels, thus increasing effective filtration pressure in the glomerulus.33
afferent vessels, thus increasing effective filtration pressure in the glomerulus.33
V1b receptors are located on the anterior hypophysis; stimulation induces liberation of ACTH and prolactin.36 Accordingly, Kornberger et al.37 reported significantly higher serum ACTH and cortisol concentrations in animals resuscitated from cardiac arrest with arginine vasopressin as compared with epinephrine. However, in patients with advanced vasodilatory shock, a continuous arginine vasopressin infusion at dosages of 4 IU/hr affected neither serum ACTH nor cortisol concentrations.38 A complex dysfunction of the hypophyseal–adrenal axis in critical illness may explain the lack of effects of the potent stimulator arginine vasopressin on ACTH-producing cells. Nonetheless, arginine vasopressin seems to be able to promote prolactin excretion by stimulating V1b receptors. Additional V1b receptors are expressed on pancreatic islet cells, where they enhance insulin secretion in the presence of high glycemic levels.39
Arginine Vasopressin During CPR
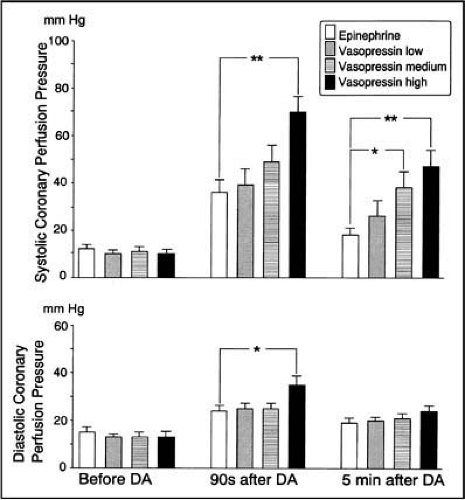
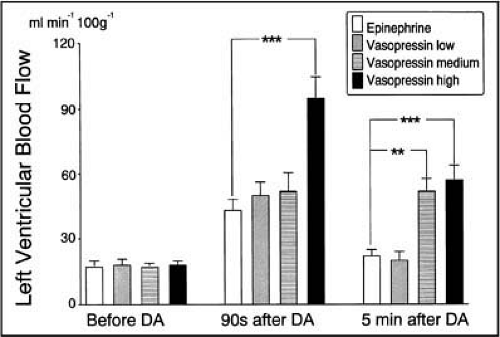
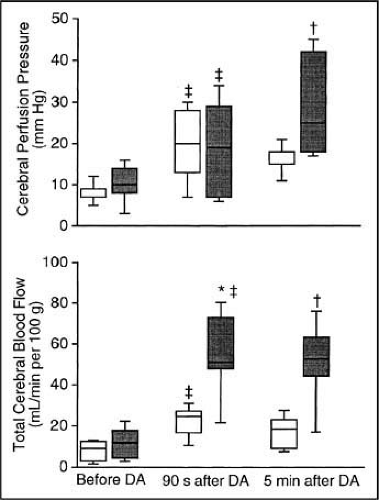
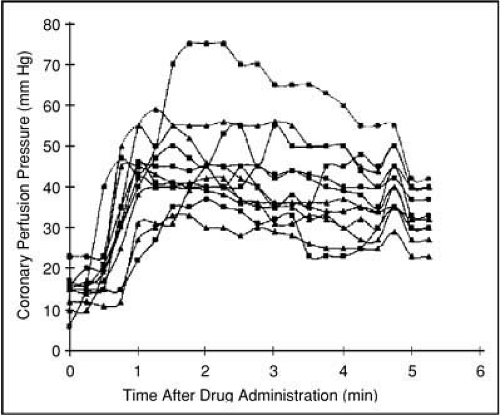
In a porcine model simulating ventricular fibrillation, a dose–response investigation of three arginine vasopressin dosages (0.2, 0.4, and 0.8 U/kg) compared with the maximum effective dose of 200 μg/kg of epinephrine showed that 0.8 U/kg of arginine vasopressin was most effective at increasing blood flow to vital organs40 (Figs. 27-2 and 27-3). Correspondingly, arginine vasopressin significantly improved cerebral oxygen delivery during CPR when compared with a maximum dose of epinephrine41 (Fig. 27-4). Furthermore, the effects of arginine vasopressin on vital organ blood flow lasted longer after arginine vasopressin than after
epinephrine (∼4 versus ∼1.5 min); indeed, it was found that significantly more arginine vasopressin animals could be resuscitated.42 The same dose of intravenous and endobronchial arginine vasopressin resulted in similar coronary perfusion pressures 4 minutes after drug administration.43,44 Intraosseous versus intravenous arginine vasopressin administration led to comparable arginine vasopressin plasma levels, hemodynamic variables, coronary perfusion pressures, and rates of return of spontaneous circulation (ROSC)45 (Fig. 27-5). Therefore, intraosseous arginine vasopressin might be a valuable alternative form of administration during CPR, when intravenous access is delayed or not available.
epinephrine (∼4 versus ∼1.5 min); indeed, it was found that significantly more arginine vasopressin animals could be resuscitated.42 The same dose of intravenous and endobronchial arginine vasopressin resulted in similar coronary perfusion pressures 4 minutes after drug administration.43,44 Intraosseous versus intravenous arginine vasopressin administration led to comparable arginine vasopressin plasma levels, hemodynamic variables, coronary perfusion pressures, and rates of return of spontaneous circulation (ROSC)45 (Fig. 27-5). Therefore, intraosseous arginine vasopressin might be a valuable alternative form of administration during CPR, when intravenous access is delayed or not available.
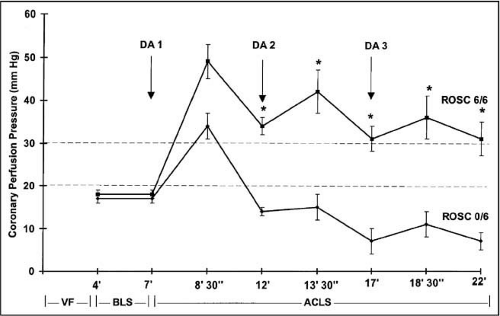
After repeated dosages of arginine vasopressin versus epinephrine were administered in a porcine model, coronary perfusion pressure increased only after the first of three epinephrine injections, but it increased after each of three arginine vasopressin injections.
After repeated dosages of arginine vasopressin versus epinephrine were administered in a porcine model, coronary perfusion pressure increased only after the first of three epinephrine injections, but it increased after each of three arginine vasopressin injections; accordingly, all arginine vasopressin animals survived, whereas all pigs resuscitated with epinephrine died46 (Fig. 27-6). In the early postresuscitation phase of the same model, arginine vasopressin administration resulted in higher arterial blood pressure but a lower cardiac index; a reversible depressant but not critical effect on myocardial function by arginine vasopressin was observed when compared with epinephrine.47 Renal and splanchnic perfusion may be impaired during48 and after49 successful resuscitation from cardiac arrest. Arginine vasopressin impaired mesenteric blood flow during CPR and in the early postresuscitation phase.24 However, neither renal blood flow nor renal function was influenced by arginine vasopressin or epinephrine in this investigation.
In a model of prolonged advanced cardiac life support (22 minutes), all arginine vasopressin animals had ROSC, whereas all pigs in the epinephrine and saline placebo group died. Twenty-four hours after ROSC, the only neurologic deficit of pigs resuscitated with arginine vasopressin was an unsteady gait, which disappeared within 3 days. Subsequently performed magnetic resonance imaging revealed no cerebral cortical or subcortical edema, intraparenchymal hemorrhage, ischemic brain lesions, or cerebral infarction, indicating that pigs treated with arginine vasopressin but not those treated with epinephrine recovered fully from cardiac arrest, both anatomically and physiologically, even after prolonged CPR.50
In a model of advanced cardiac life support after 7 minutes of cardiac arrest, the administration of arginine vasopressin—compared with epinephrine or the combination of epinephrine and arginine vasopressin—did not improve the behavioral and cerebral histopathologic outcome.51
Clinical Trials of Vasopressin in Cardiac Arrest
In patients with refractory cardiac arrest, arginine vasopressin induced an increase in arterial blood pressure and, in some cases, ROSC, where standard therapy with chest compressions, ventilation, defibrillation, and epinephrine had failed.52 In a small (n = 40) prospective randomized investigation of patients with shock-refractory out-of-hospital ventricular fibrillation, a significantly larger proportion of patients treated with arginine vasopressin were successfully resuscitated and survived 24 hours compared with patients treated with epinephrine.53 In 1999, a Chinese study group reported a prospective randomized trial comparing two different dosages of arginine vasopressin and two different dosages of epinephrine in 83 patients with in-hospital cardiac arrest. Their findings indicated that high-dose arginine vasopressin (1 IU/kg) significantly increased the rate of ROSC and improved the survival rate compared with standard (1 mg) and high dosages (5 mg) of epinephrine.54 In a large (n = 200) in-hospital CPR trial from Ottawa, Canada, comparable short-term survival was found in both groups treated with either arginine vasopressin or epinephrine, indicating that these drugs may be equipotent when response times of providers are short.55 In another clinical evaluation in Detroit, Michigan, 4 of 10 patients responded to arginine vasopressin administration after ∼45 minutes of unsuccessful advanced cardiac life support and had a mean increase in coronary perfusion pressure of 28 mm Hg.56 This
is surprising, since an arterial blood pressure increase with any drug after such a long period of ineffective CPR management is expected to be minimal.
is surprising, since an arterial blood pressure increase with any drug after such a long period of ineffective CPR management is expected to be minimal.
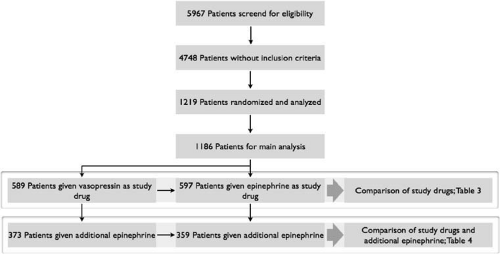
From June 1999 to March 2002, we conducted a large multicenter trial in Austria, Germany, and Switzerland and randomized 1,219 out-of-hospital cardiac arrest patients to be treated with epinephrine or arginine vasopressin57 (Fig. 27-7). Hospital admission and discharge rates were comparable between treatment arms for patients with ventricular fibrillation and for pulseless electrical activity, but patients with asystole were more likely to survive when primarily treated with arginine vasopressin (Table 27-1, Fig. 27-8). However, if patients could not be successfully resuscitated with two injections of arginine vasopressin, additional epinephrine significantly improved hospital admission (P = 0.002) and discharge rates (P = 0.002) when compared with patients who were treated with epinephrine alone (Table 27-2, Fig. 27-9). There was no difference in cerebral performance between groups for the entire trial.
These results could not confirm earlier data suggesting that arginine vasopressin was more effective than epinephrine as a first-line vasopressor drug in the treatment of ventricular fibrillation, pulseless electrical activity, or asystole.40,41,42,46,50,53 Criticism has been raised that arginine vasopressin may improve coronary and cerebral perfusion pressures during CPR with refractory ventricular fibrillation
and pulseless electrical activity, but that it will not improve outcome. Unfortunately we are unable to state whether this phenomenon may be similar to the observations described with high-dose epinephrine during CPR, when increasing epinephrine dosages were effective in the laboratory58 but not in clinical practice.59 It is clearly a principal problem to extrapolate laboratory CPR to the clinical setting, since species differences, comparing diseased patients with healthy laboratory animals, or differences in out-of-hospital CPR compared with laboratory conditions are hardly controllable factors of influence.
and pulseless electrical activity, but that it will not improve outcome. Unfortunately we are unable to state whether this phenomenon may be similar to the observations described with high-dose epinephrine during CPR, when increasing epinephrine dosages were effective in the laboratory58 but not in clinical practice.59 It is clearly a principal problem to extrapolate laboratory CPR to the clinical setting, since species differences, comparing diseased patients with healthy laboratory animals, or differences in out-of-hospital CPR compared with laboratory conditions are hardly controllable factors of influence.
Table 27-1 • European Multicenter Study: Data on Outcome in All Patients | |||||||
|---|---|---|---|---|---|---|---|
|