Chapter 33 Non-invasive ventilation
Non-invasive ventilation (NIV) is a valuable therapeutic option in the management of acute and chronic respiratory failure – for some diagnoses it is the preferred option. Successful use of NIV in acute respiratory failure (ARF) was first published in 1936,1 and the use of NIV predates the introduction of laryngoscopy (early 1900s) and the widespread use of positive-pressure mechanical ventilation (MV) via an endotracheal tube (1950s).2
NIV is defined as ventilatory support without an (invasive) endotracheal airway. It has an increasingly important role in the short-term management of readily reversible ARF,3,4 and in chronic respiratory failure due to obstructive sleep apnoea (OSA) and neuromuscular disease.
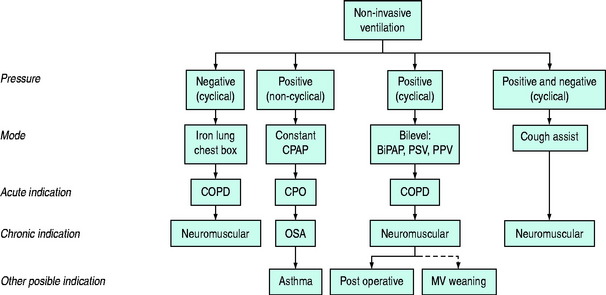
NIV may be achieved either through the delivery of positive airway pressure (Pao) or the application of a negative-pressure generator to the chest (‘chest box’ or cuirass) or body (‘iron lung’). A conceptual framework is shown in Figure 33.1. This chapter deals primarily with the use of positive-pressure NIV to treat ARF.
Negative-pressure generators may be used for the management of acute or chronic respiratory disease.5 Major limitations to the use of negative-pressure generators include the induction of OSA, lack of fractional inspired oxygen (FiO2) control, equipment bulk and size.6 However, external negative-pressure generators suit some patients with chronic respiratory failure, particularly as there is no oral or nasal prosthesis.
The clinical efficacy of NIV depends upon: (1) the mode used; and (2) the nature and severity of the underlying respiratory disorder. Correctly applied, NIV can reduce morbidity and mortality, whereas inappropriate application may delay definitive therapy and adversely affect outcome. An understanding of the physiologic rationale for NIV will assist the clinician in understanding the indications and benefits, and predict the side-effects of the various NIV modes.7,8 Many of the general issues regarding ventilation are discussed in Chapter 27, and this chapter will focus on those issues specific to NIV.
PHYSIOLOGY OF NIV
See Chapter 27 for a more detailed explanation.
This relationship may be rearranged into its individual components, as follows:
where E is the respiratory elastance (inverse of compliance), V is the volume of gas, R is the respiratory and circuit flow-resistance,  is the inspiratory flow rate and PEEPi is the sum of the extrinsic and intrinsic PEEP (≈Pthres).
is the inspiratory flow rate and PEEPi is the sum of the extrinsic and intrinsic PEEP (≈Pthres).
BILEVEL POSITIVE AIRWAY PRESSURE (BPAP)
BPAP allows separate settings for inspiratory (IPAP) and expiratory (EPAP) airway pressure levels, and is conceptually similar to PSV plus CPAP. Respiratory frequency is usually determined by the spontaneous rate but may be time-cycled and independent of patient effort. In some patients BPAP may not be as effective in reducing Pmus as the combination of PSV plus CPAP.2,12
PATIENT–VENTILATOR INTERACTION
This is discussed in Chapter 27, and subdivided into: (1) triggering of inspiration; (2) inspiration; and (3) cessation of inspiration. The only aspect that is specific to NIV arises from mask leaks that may interfere with the ability to sense the end of expiration because there is continued ‘expiratory’ gas flow.
NON-INVASIVE VENTILATION EQUIPMENT
Equipment design varies according to NIV mode and purpose (e.g. critical care or domiciliary setting), and significant variation in performance characteristics have been documented.12,13 The important characteristics of an efficient NIV circuit include:
Many mask designs are also available and the optimal design depends upon the purpose and mode of NIV and patient anatomy and preference. These include intranasal, nasal, oronasal, full-face and helmet (full-head) masks. Desirable features of a mask include light-weight and transparent materials providing a comfortable air-tight seal with minimal dead space and separate inspiratory and expiratory ports to minimise airflow turbulence and rebreathing.13,14 In lung model studies, expiratory ports over the nasal bridge reduce dead space,15 which may prove to be clinically advantageous.
COMPLICATIONS AND ASSESSMENT OF EFFICACY
Contraindications and complications specific to NIV are listed in Table 33.1. Most patients requiring NIV should be managed in a critical care ward with appropriately trained medical and nursing staff. Although the development of sophisticated, portable, non-invasive ventilators makes iteasy to provide NIV in any environment, its benefits may diminish outside the critical care environment.16,17
Table 33.1 Contraindications and complications of non-invasive ventilation
| Contraindications |
| Complications |
NON-INVASIVE VENTILATION AND ACUTE RESPIRATORY FAILURE2,16,18
CARDIOGENIC PULMONARY OEDEMA (CPO)2,8,19
Over 20 prospective randomised controlled trials of NIV in CPO have consistently demonstrated physiologic improvements in hypoxic and hypercapnic respiratory failure, and a significant reduction in the need for intubation, hospital length of stay and improved survival (95% confidence interval (CI) relative risk (RR) = 0.38–0.90).19 Even though the majority of these patients were managed in a critical care setting the average duration of respiratory support was much shorter for NIV (9 ± 11 hours) than those who required MV.20
The optimal mode of NIV in CPO appears to be CPAP alone. The optimal Pao level remains to be resolved, although 10 cmH2O appeared to be safe and effective in the majority of subjects. Whilst the addition of a differential inspiratory pressure (e.g. bilevel21 and PSV22,23) appears to be as effective as CPAP, it does not appear to provide an additional outcome benefit19 and may increase the rate of myocardial infarction24,25 (95% CI RR 0.92–2.42).19 Bilevel NIV and CPAP have equivalent impact on respiratory parameters, but may have different effects on myocardial function.24,25 CPAP reduces preload and afterload9,10 and myocardial catecholamine release26 but the cyclical Pao (of bilevel NIV) may cause preload and afterload to rise and fall during respiration.2,27
Current evidence supports the routine use of mask CPAP in moderate or severe CPO as standard therapy and as the first-line option for respiratory support.16,28

Full access? Get Clinical Tree


 ) to reverse respiratory acidosis and hypercarbia
) to reverse respiratory acidosis and hypercarbia ) may be viewed as the summation of the individual forces that must be overcome to generate inspiratory flow, namely: elastic work (or ‘stretch’; Wel), flow-resistive work (airflow obstruction; Wres), and threshold work (Wthres). Since the volume component is constant the equation of motion can be written as:
) may be viewed as the summation of the individual forces that must be overcome to generate inspiratory flow, namely: elastic work (or ‘stretch’; Wel), flow-resistive work (airflow obstruction; Wres), and threshold work (Wthres). Since the volume component is constant the equation of motion can be written as:
 .
.
 . Hypermetabolic states (e.g. trauma, sepsis) increase basal
. Hypermetabolic states (e.g. trauma, sepsis) increase basal  , whereas pulmonary and chest wall diseases increase respiratory workload, and neuromuscular disease impairs respiratory muscle effort. NIV may prevent respiratory failure by counterbalancing the respiratory workload and/or reducing respiratory muscle effort, and thus maintain
, whereas pulmonary and chest wall diseases increase respiratory workload, and neuromuscular disease impairs respiratory muscle effort. NIV may prevent respiratory failure by counterbalancing the respiratory workload and/or reducing respiratory muscle effort, and thus maintain  .
.

