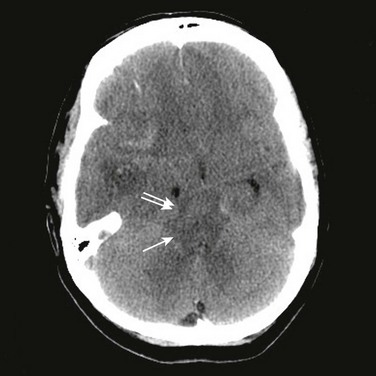
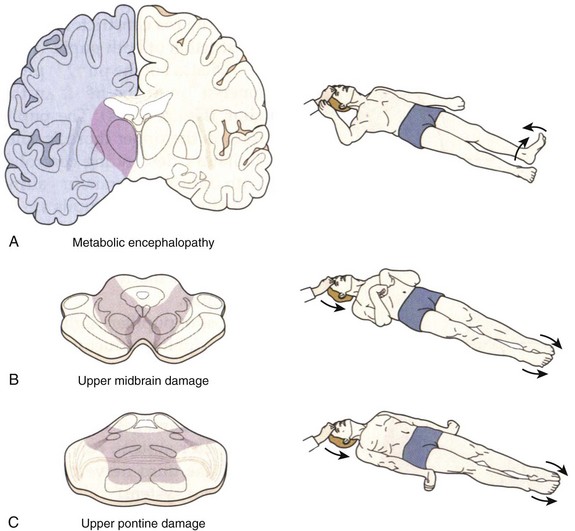
62 The clinical examination in brain death is the most unequivocal in neurology. Most of the time, establishing the diagnosis of brain death on clinical grounds is not a difficult task, as long as providers follow established protocols and guidelines for the interpretation of findings during clinical examination.1,2 However, there may be confusion based on the variability of the interpretation of current guidelines,3,4 hurdles to clinical examination in specific patient populations such as trauma victims, laws from specific jurisdictions, and the changing face of outcomes after severe brain injury in an era of advancements in critical care and resuscitative medicine. In this chapter we will review current procedures and recommendations for the evaluation of comatose patients presumed brain dead, the concept of brain death substantiated by anatomic and physiologic bases, important concepts for the determination of brain death in the setting of novel interventions such as hypothermia and extracorporeal circulation, and how to avoid pitfalls during the evaluation of patients presumed brain dead. The concept of brain death is modern to medicine but the definition of death has historically been associated with physiologic cessation of cardiopulmonary function. With advancements in mechanical ventilation, life support, and resuscitation medicine, a new state in which a patient’s cardiopulmonary functions could be sustained in the absence of neurologic function emerged. In 1959, Mollaret and Goulon described 23 patients with irreversible coma, whose clinical syndrome was characterized by the absence of brainstem function, spontaneous respiratory function, and cardiovascular collapse that ensued without the use of vasopressors, in what became the birth of the concept of brain death.5 In 1963, Harvard neurologists proposed that a patient be certified as dead in the setting of coma, absence of brainstem reflexes, apnea for 30 minutes, and an isoelectric electroencephalogram (EEG) tracing in all leads for more than 30 minutes,6 despite the presence of cardiac function. The first guideline (the Harvard criteria) for deciding brain death was established in 1968.7 This concept has been accepted worldwide, although its fundamental meaning is not exactly globally uniform yet. Some countries, such as the United States, accept the concept of brain death as “whole brain death,” which is defined as irreversible loss of all cortical and brainstem function. The Medical Royal Colleges of the United Kingdom established the definition of brain death on a “lower brain” concept of brainstem death.8 In the opinion of the Royal Medical College, permanent unconsciousness secondary to neuronal death of brainstem structures such as the reticular activating system (RAS) is irreversible.8 In 1981, a Presidential Commission in the United States was formed to address the issue of death by neurologic criteria.9 The President’s Commission established the foundations of the criteria currently used in the United States for the diagnosis of brain death: the cause of brain death should be known and irreversible and no improvement in neurologic condition should occur during a period of observation; the period of observation was left at the discretion of the physician, but periods of 6 to 12 hours were recommended depending on the availability of confirmatory testing such as EEG or cerebral perfusion scans.9 Though the President’s Commission suggested periods of observation of 24 hours for cases of ischemia-anoxia,9 more recent clinical experience in the era of therapeutic hypothermia and published guidelines suggest a period of observation of up to 72 hours in patients with hypoxic-ischemic coma.10 The President’s Commission guidelines for the determination of brain death culminated in a proposal for a legal definition that led to the Uniform Determination of Death Act (UDDA) in 1981. Under the law, the determination of death must be made with accepted medical standards and can be established only if an individual “has sustained either: 1) irreversible cessation of circulatory and respiratory functions, or 2) irreversible cessation of all functions of the entire brain, including the brain stem.” In 1995, the American Academy of Neurology (AAN) published the practice parameter to delineate the medical standards for the determination of brain death.11 The guideline emphasized the three clinical findings necessary to confirm irreversible cessation of all brain functions including the brainstem: (1) known cause and presence of coma, (2) absence of brainstem reflexes, and (3) apnea.11 Despite this publication, there is considerable practice variation in the adherence to the AAN guidelines for the determination of brain death, particularly in areas related to definitions of acceptable core temperature, number of required examinations, ancillary testing to be used,3 and deficiencies in documentation.3 In response to this phenomenon, the AAN published an evidence-based update of the 1995 Practice Parameter12 to answer the main questions related to practice variability in the determination of brain death.3,13 In the United States, most state laws have adopted the UDDA, and some have added their own amendments. All states and the District of Columbia have statutes for determining brain death based on the UDDA, but certain statutes differ in minor points such as the requirement that determination of brain death should be done by two different physicians, the use of confirmatory testing, and the notification of next of kin before the declaration of brain death. To this end, it is important for the practitioner to understand local hospital policies for the declaration of brain death that should abide by the laws of their respective jurisdictions. Additional information about specific status in jurisdictions of the United States can be downloaded from http://www.braindeath.org. The most common causes of brain death in the adult population are traumatic brain injury (TBI), aneurysmal subarachnoid hemorrhage (SAH), hypoxic-ischemic injury, and fulminant hepatic failure.14 It is estimated that the diagnosis of brain death is made at least 25 to 30 times a year in large referral centers, but this number may be lower in nonacademic centers.14 The determination of brain death is based on the UDDA and supported by the AAN Practice Parameter.11,12 The diagnosis is based on the establishment of three main criteria: (1) known cause and presence of coma, (2) absence of brainstem reflexes, and (3) apnea. Therefore, the clinical diagnosis, when considering accepted guidelines, is the most unequivocal in neurology. In general, most jurisdictions require that the determination of brain death be made by a licensed physician, which in most of the cases should be an attending physician who has experience in the assessment of comatose patients and the legal requirements applicable to the jurisdiction of practice. Some centers require the testing to be performed by two different physicians, and some centers require one of these physicians to be a neurologist, neurosurgeon, or critical care specialist. In the United States, 42% of top neuroscience centers required the brain death examination to be documented by a neurologist or neurosurgeon and only 35% required that an attending neurologist or neurosurgeon be involved; of the 42% centers, residents could document the examination in up to 65% of the centers.3 In those circumstances in which the patient is a potential organ donor, the clinical team may not be directly involved with the discussions of organ procurement, as a conflict of interest may be apparent. Practitioners should first determine the cause of coma by history, physical examination, neuroimaging, and laboratory testing. Exclusion of central nervous system (CNS) depressants should be attempted by careful history taking, drug screen testing, and calculation of drug clearance using the rule of five times the drugs half-life (assuming a normal hepatic and renal function) or drug plasma levels below therapeutic ranges.12 In the setting of abnormal hepatic or renal function, or after use of therapeutic hypothermia, caution should be taken before entertaining the diagnosis of brain death based on changes in drug metabolism inherent to these clinical settings, and to avoid catastrophic and embarrassing misdiagnoses.15 In these circumstances, more than recommended times for observation are suggested or the use of confirmatory testing may be sought. The legal limit for ethanol is a blood alcohol content of 0.08%, which is a practical threshold below which an examination to determine brain death could reasonably proceed.12 In those patients exposed to pentobarbital for the management of intracranial hypertension, an accepted level in which a clinical examination can proceed without chance of confounding is 10 µg/mL.12 There should be no temporal administration of neuromuscular blockers and this can be assessed definitely by the presence of train-of-four twitches with maximal ulnar stimulation. Acid-base status and electrolyte levels must not be severely deviated from the norm, but the presence of signs and symptoms of diabetes insipidus does not preclude the diagnosis of brain death; however, treatment with fluids and vasopressors such as vasopressin will target both sodium and blood pressure requirements to allow for adequate neurologic assessment. With more cardiac arrest survivors being exposed to therapeutic hypothermia, practitioners should now achieve a normal core temperature, defined as near-normal temperature or core temperature higher than 36° C, before attempting to determine brain death. Patients should have normal blood pressure, defined as systolic blood pressure (SBP) equal to or higher than 100 mm Hg, as the neurologic examination is usually reliable at this level of blood pressure. A temporal cause of severe brain injury must be established. Irreversibility from neurologic injury is recognized by the extent of the injury, the devastation in neurologic findings, and the lack of improvement. Neuroimaging is useful in establishing an acute neurologic catastrophe that is compatible with the clinical diagnosis. In most cases, a computed tomography (CT) scan will reveal specific findings such as diffuse cerebral edema, mass lesions with severe shift of midline structures, and herniation (Fig. 62.1). Coma is established by the lack of all evidence of responsiveness. That is, eye opening or eye movement to noxious stimuli must be absent. The motor responses to noxious stimuli should not be flexor or extensor but spinally mediated. The clinical differentiation of motor responses may require experience and specific training in neurology or neurosurgery. When flexor posturing of the upper extremities and extension of the lower extremities (decorticate) or extensor posturing of both the upper and lower extremities (decerebrate) is observed, the diagnosis of brain death cannot be entertained and an additional period of observation is recommended (Fig. 62.2). The basis of these responses is related to the patency of the rubrospinal and vestibulospinal tracts, and lower segments of the medulla that connect with the spinal cord.16 Brain death patients typically exhibit spinal cord–mediated motor responses characterized by “en bloc” flexor responses of the lower extremities with flexion of the hip, flexion of the knee, and dorsiflexion of the ankle and toes (the so-called triple flexion response or Babinski en bloc spinal cord sign) (see Fig. 62.2). More complex movements that have been referred to as brain death–associated reflexes (Lazarus sign, spinal man, spinal reflexes, or spinal automatisms) have been described in patients who otherwise meet all other brain death criteria.17 When in doubt, the neurologic examination of a comatose patient becomes equivocal, and in these circumstances, additional observation or a confirmatory test may be warranted.
Neurologic Criteria for Death in Adults
Historical Perspective and Definitions
Determination of Brain Death
Clinical Evaluation of Coma and Prerequisites
Neurologic Criteria for Death in Adults