Dipty Mangla and Ashish Sinha
1. Total normal cerebral blood flow (CBF) is
A. 25 mL/100 g/min
B. 50 mL/100 g/min
C. 100 mL/100 g/min
D. 150 mL/100 g/min
2. The factor associated with maximum increase in intracranial pressure (ICP) is
A. Increased central venous pressure to 14 mm Hg
B. Hypercarbia with PaCO2 of 50 mm Hg
C. Ventilation with positive end–expiratory pressure (PEEP) of 5 cm H2O
D. Bucking and coughing on endotracheal tube
3. Cerebral perfusion pressure (CPP) (mm Hg) in a patient with intracranial pressure (ICP) of 12 mm Hg, central venous pressure (CVP) of 15 mm Hg, and mean arterial pressure (MAP) of 70 mm Hg will be
A. 58
B. 55
C. 52
D. 48
4. Treatment of a patient with mannitol can lead to all the following, except
A. Oliguria
B. Hypotension
C. Hypervolemia
D. Hypokalemia
5. A patient is undergoing craniotomy for subdural hematoma. During the procedure, the surgeon requests lowering the intracranial pressure. All the following can be used, except
A. Mannitol
B. Hyperventilation
C. Steroids
D. Furosemide
6. The desired level of PaCO2 in a neurosurgical patient is
A. 30 to 35 mm Hg
B. 25 to 30 mm Hg
C. 20 to 25 mm Hg
D. 15 to 25 mm Hg
7. An absolute contraindication for electroconvulsive therapy (ECT) is
A. Hypertension
B. Pheochromocytoma
C. Aortic aneurysm
D. Stroke
8. Signs of air embolism in a patient include all, except
A. Hypertension
B. Heart murmur
C. Arrhythmia
D. Decreased EtCO2
9. A 65-year-old male is undergoing surgery for medulloblastoma in the posterior fossa of brain. Approximately 1 hour into surgery you notice arrhythmias on the monitors. The next step will be
A. Inform the surgeon
B. Give β-blockers
C. Administer lidocaine
D. Give 100% oxygen
10. Nitrous oxide should be avoided in patients with
A. Subdural hematoma
B. Brain tumor
C. Closed head injury
D. Pneumocephalus
11. The following fluid should be avoided in a patient undergoing craniotomy
A. Lactated Ringerés
B. Normal saline
C. Dextrose 5%—normal saline
D. Hetastarch
12. Most sensitive method to detect air embolism is
A. Transesophageal echocardiogram (TEE)
B. Decreased end-tidal carbon dioxide
C. Increased end-tidal nitrogen
D. Mill wheel murmur
13. Best measure to reduce cerebral oxygen consumption includes
A. Administration of barbiturates
B. Hyperventilation
C. Administration of opioids
D. Institution of hypothermia
14. All of the following decrease cerebral blood flow (CBF), except
A. Etomidate
B. Propofol
C. Thiopental
D. Ketamine
15. In a patient undergoing craniotomy, the transducer of arterial line should be zeroed at the
A. Level of hypothalamus
B. Level of heart
C. Level of external auditory meatus
D. Level of atmosphere
16. Jugular venous oxygen saturation
A. Estimates oxygen extraction
B. Is unaffected by systemic hypoxia
C. Involves placement of catheter through inferior vena cava
D. Monitors global oxygenation of both cerebral hemispheres
17. The effect of ischemia on somatosensory-evoked potentials (SSEPs) is
A. Decreased latency, decreased amplitude
B. Increased latency, increased amplitude
C. Decreased latency, increased amplitude
D. Increased latency, decreased amplitude
18. A patient with spinal injury, sustained 3 hours ago, comes to the OR for exploratory laparotomy. Anesthetic management of the patient includes which of the following?
A. Rapid-sequence induction with succinylcholine
B. Hypothermia for better neurologic outcome
C. Managing autonomic hyperreflexia
D. Avoiding corticosteroids
19. The electrophysiological monitor most resistant to anesthetic agents is
A. Somatosensory-evoked potentials
B. Motor-evoked potentials
C. Brain-stem auditory-evoked potentials
D. Electroencephalography
20. The most reliable monitor for neurologic monitoring in a patient undergoing carotid endarterectomy is
A. Electroencephalogram
B. Jugular venous oxygen saturation
C. Awake neurologic exam
D. Stump pressure
21. Anesthetic management of a patient with multiple sclerosis (MS) includes
A. Avoiding hypothermia
B. Avoiding hyperthermia
C. Spinal anesthesia is safe
D. Use of succinylcholine can result in hypokalemia
22. All the following are true for Guillain–Barré syndrome (GBS), except
A. Respiratory paralysis is frequent complication
B. Presence of labile autonomic nervous system
C. Ascending motor paralysis
D. Exaggerated reflexes
23. True statement about autonomic hyperreflexia is
A. Lesions below T10 is responsible for the reflex
B. It can be treated with deep general anesthetic
C. It is associated with vasoconstriction above the site of injury
D. It can be provoked by thermal stimulation
24. A 16-year-old patient with acute lysergic acid diethylamide (LSD) intoxication and head injury comes to emergency room. All the following can be used in anesthetic management, except
A. Propofol
B. Succinylcholine
C. Ketamine
D. Phenylephrine
25. A 25-year-old patient with severe depression is undergoing an electroconvulsive therapy (ECT). The duration of seizure can be increased by
A. Hypoventilating the patient
B. Hyperventilating the patient
C. Administering succinylcholine
D. Administering rocuronium
26. All of the following are contraindications of electroconvulsive therapy (ECT), except
A. Pacemaker
B. Recent stroke
C. Raised intracranial pressure
D. Severe osteoporosis
27. True statement regarding cerebral physiology is
A. Normal cerebral metabolic oxygen consumption is 5 mL/100g/min
B. Normal Intracranial pressure (ICP) is approximately 15 mm Hg
C. Normal cerebral blood flow (CBF) is 50 mL/100g/min
D. Cerebral autoregulation is strictly maintained at blood pressures between 60 and 150 mm Hg in all patients
28. True statement about cerebrospinal fluid (CSF) is
A. It is formed in the third ventricle
B. It is absorbed in arachnoid granulations present in fourth ventricle
C. Total volume of CSF is about 150 mL
D. Major mechanism of formation is by passive diffusion of ions
29. A precordial Doppler can detect a minimal of ___ mL of intracardiac air:
A. 0.1
B. 0.25
C. 0.5
D. 1
30. The only inhalational anesthetic that can cause an isoelectric EEG among the following is
A. Isoflurane
B. Halothane
C. Enflurane
D. Nitrous oxide
31. Intraoperative anesthetic management of a patient undergoing cerebral aneurysm repair includes all, except
A. Maintenance of hypotension
B. Mannitol for facilitating surgical exposure
C. Maintaining mild hypothermia
D. Patient remaining intubated for 24 hours postoperatively
32. Which of the following types of neuromonitoring can be done in a patient undergoing transsphenoidal resection of a pituitary tumor?
A. EEG
B. Motor-evoked potentials
C. Visual-evoked potentials
D. Auditory-evoked potentials
33. The drug of choice for treating nausea and vomiting in a patient with parkinsonism would be
A. Ondansetron
B. Promethazine
C. Droperidol
D. Metoclopramide
34. All the following anesthetic agents can cause seizurelike activity on the electroencephalogram (EEG), except
A. Ketamine
B. Etomidate
C. Enflurane
D. Thiopental
35. The neuromuscular blocking agent relatively contraindicated in a patient with raised intracranial pressure (ICP) is
A. Rocuronium
B. Vecuronium
C. Atracurium
D. Cisatracurium
36. The afferent input for somatosensory-evoked potentials is carried by which spinal cord tract
A. Corticospinal
B. Dorsal columns
C. Spinothalamic
D. Spinocerebellar
37. You are called to evaluate a 50-year-old patient for brain death. All the following are criteria for brain death, except
A. Apnea for 10 minutes
B. Absence of corneal reflex
C. Presence of spinal reflexes
D. Decerebrate posturing
38. A 30-year-old male is found unresponsive outside a supermarket. The emergency response team finds him in ventricular fibrillation. After 10 minutes of CPR, the emergency response team is successful in reviving the patient. In the emergency room, it is decided to cool the patient to 34°C from 37°C. By this measure, the cerebral metabolic demand will decrease by
A. 12%
B. 18%
C. 24%
D. 30%
39. All the following are relative contraindications to a sitting craniotomy, except
A. Right-to-left cardiac shunt
B. Patent foramen ovale
C. Ventriculoatrial shunt
D. Ventriculoperitoneal shunt
40. An 80-year-old female comes to the ER with closed distal radial fracture. On further questioning, she gives a history of stroke about 2 weeks ago. How long should one wait before it can be assumed that her risk of perioperative stroke is same as a healthy 80-year-old?
A. 6 days
B. 6 weeks
C. 6 months
D. 6 years
41. A 28-year-old male is being treated in the ICU for raised intracranial pressure (ICP). All the following measures can aid in decreasing ICP quickly, except
A. Corticosteroids
B. Hyperventilation to PaCO2 of 30 mm Hg
C. Mannitol
D. Head elevation to 30 degrees
42. Which of the following agents will have the least effect on somatosensory-evoked potentials (SSEPs)?
A. Vecuronium
B. Propofol
C. Fentanyl
D. Nitrous oxide
43. Signs and symptoms of raised intracranial hypertension include all the following, except
A. Hypertension
B. Tachycardia
C. Bradycardia
D. Irregular respiration
44. Etomidate in a dose of 0.2 mg/kg can lead to all the following, except
A. Abolish ventilatory response to carbon dioxide
B. Increase amplitude and latency of somatosensory-evoked potentials (SSEPs)
C. Decrease cerebral metabolic oxygen demand
D. Decrease cerebral blood flow (CBF)
45. The most important factor governing cerebral blood flow (CBF) is
A. Cerebral metabolic oxygen demand
B. PaCO2
C. pH
D. Cerebral perfusion pressure
46. The following graph depicts the relationship between cerebral perfusion and
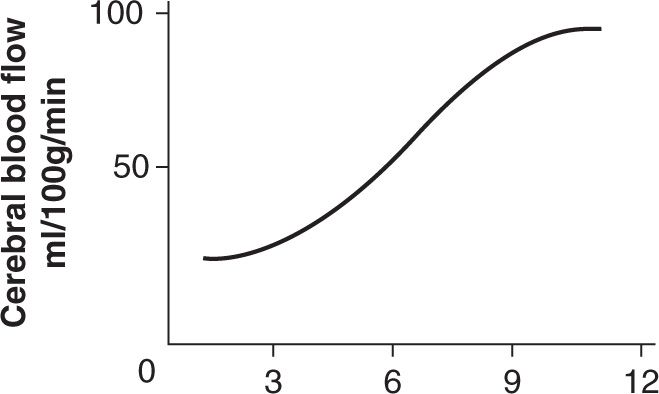
Figure 13-1.
A. PaCO2
B. PaO2
C. Mean arterial pressure
D. Cerebrospinal fluid pH
47. The following graph depicts the relationship between cerebral perfusion and
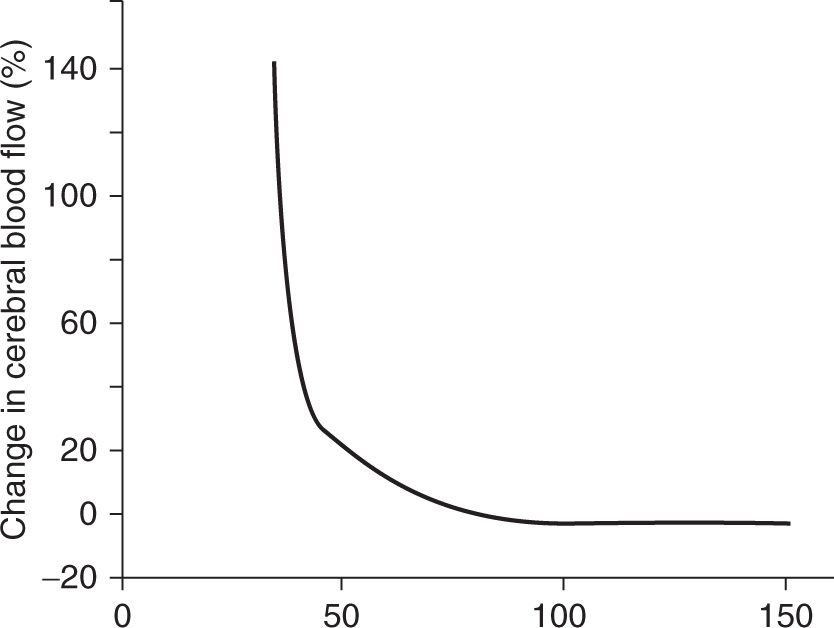
Figure 13-2.
A. PaCO2
B. PaO2
C. Mean arterial pressure
D. Cerebrospinal fluid pH
48. A 45-year-old male is seen in the preadmission testing for pituitary adenoma resection surgery. All the following would be expected if this adenoma was causing acromegaly, except
A. Hypotension
B. Obstructive sleep apnea
C. Difficult airway
D. Hyperglycemia
49. The fastest measure to decrease intracranial pressure (ICP) in a patient is
A. Mannitol
B. Dexamethasone
C. Furosemide
D. Hyperventilation
50. Therapy for cerebral vasospasm includes
A. Hypertension, hypervolemia, hemodilution
B. Normotension, euvolemia, hypocarbia
C. Hypotension, hypovolemia, hypocarbia
D. Hypertension, hypervolemia, hypocarbia

Full access? Get Clinical Tree






