Neural Blockade for Surgery to the Head and Neck
Ban C. H. Tsui
Derek Dillane
Brendan T. Finucane
Regional anesthesia techniques for the head and neck region are diversified. The majority of head and neck surgical procedures are amenable to some form of regional anesthesia, including being used as the sole anesthetic (stand-alone), as a component of a balanced general anesthesia technique, or for effective postoperative pain control. In addition, regional block procedures in this area can serve both in a diagnostic role and for the therapeutic management of acute and chronic pain syndromes. Head and neck regional blockade is effective in the management of somatic pain, and the techniques can range from local infiltration to field blocks to specific nerve blocks. This chapter briefly reviews the major clinical uses of head and neck regional anesthesia with respect to the wide range of relevant surgical disciplines. Specific regional techniques are described in detail in Chapters 17,18,19, and are discussed in this chapter only where applicable.
Ophthalmic Surgery
Conventional prerequisites for intraocular surgery under regional anesthesia are globe and conjunctival anesthesia; globe, lid, and periorbital akinesia; and intraocular hypotonia (1). Because of the widespread use of phacoemulsification techniques, surgical requests for total akinesia and lowered intraocular pressure have decreased (2). Despite retrobulbar anesthesia being originally regarded as the gold standard in ocular anesthesia, major complications of the technique are well documented (3). These include globe perforation, retinal vascular occlusion, retrobulbar hemorrhage, optic nerve damage, and even cardiac and respiratory arrest (4,5,6). Greater emphasis is now placed on safety during eye block, and this has led to the evolution of several newer techniques, even at the price of incomplete akinesia. These techniques may be beneficial in anterior segment surgery, in particular cataract surgery, which 2 million patients undergo each year in the United States (7). However, some surgeons may express a wish for more complete anesthesia, especially for posterior segment surgery and for individual patients. Analgesic requirements are highest for evisceration and less so in order from enucleation through to ablation surgery, glaucoma surgery, complicated cataract surgery, and uncomplicated cataract surgery (8).
Eye Surgery
Classically, retrobulbar anesthesia is assumed to be more successful than peribulbar anesthesia. If a sufficient volume of injectate is used however, both techniques appear to have similar efficacies (9). The Atkinson “up and in” position of gaze for retrobulbar anesthesia was abandoned when Liu and co-workers (10) and Unsold and co-workers (11) demonstrated that this position placed the optic nerve nearer the path of the needle and increased the risk of nerve injury. Patients are now asked to hold the eye in the primary or neutral position (10,12,13). Some advocate for the addition of a facial nerve block with retrobulbar anesthesia to prevent blinking due to the extraocular course of the superior branch of the facial nerve to the orbicularis oculi muscle (see Figs. 19-6,19-7,19-8,19-9) (14). However, when hyaluronidase is used with local anesthetics in higher volume, effective spread through the orbital septum occurs, resulting in complete eyelid immobility (15).
Peribulbar anesthesia appears less hazardous by avoiding the risk of injury to the major structures in the intraconal space. This superiority in safety has never been proven because of the very low rate of complications and subsequent lack of power of comparative studies (2). A larger volume is needed with peribulbar anesthesia (6–12 mL) to allow spread into the intraconal space, and to the lids to provide block of the orbicularis muscle and lids immobility. The classical technique for peribulbar anesthesia involves two injections, inferotemporal and supernasal. Comparative studies confirm that a single-injection technique is effective, provided the volume of injection is sufficient (16) (see Fig. 19-12). Some authors recommend avoiding the superior nasal injection site as the distance between the orbital roof and the globe is reduced at this location, thus increasing the risk of perforation (17). The medial canthus is proposed as an alternative puncture site, and a second injection may be performed here for supplementary anesthesia in the case of a failed first injection. Spread of local anesthetic within the corpus adiposum of the orbit is unpredictable, and an additional injection is required in up to 50% of peribulbar blocks in order to achieve akinesia (18,19). This is the main disadvantage of peribulbar anesthesia (20).
Perforation of the globe has an incidence of between one in 350 and seven in 50,000 cases (21,22). The principal risk factors are physician inexperience and a highly myopic eye (22). Edge and Navon demonstrated that myopic staphyloma was the greatest risk factor (21). Vohra and Good, using B-mode ultrasound, observed that the incidence of staphyloma is greater in highly myopic than in slightly myopic eyes (23). Thus an ultrasound measurement of the globe should be performed and if the axial length is greater than 26 mm, then retrobulbar block is contraindicated.
Sub-Tenon or episcleral anesthesia places local anesthetic solution into the episcleral space. One technique that has been described involves a surgical approach using blunt scissors and a curved cannula to infiltrate the sub-Tenon canal through
the conjunctiva at the inferonasal quadrant, allowing the local anesthetic to spread circumferentially around the scleral part of the globe (see Fig. 19-19) (24). High-quality analgesia is produced with relatively low volumes (3–5 mL), and the use of higher volumes (8–11 mL) causes spread to the extraocular muscles, producing effective akinesia (25,26,27,28). Briggs and co-workers performed a comparative study between peribulbar and sub-Tenon anesthesia for cataract surgery. They conclude that sub-Tenon anesthesia reduces the overall level of discomfort associated with the administration of local anesthetic compared with the peribulbar method, in addition to providing superior intraoperative pain control (29). Several prospective studies have found that sub-Tenon anesthesia is as effective or better than retrobulbar injection for cataract surgery (30,31,32,33) or vitreoretinal surgery (34). Roman and co-workers investigated the complications associated with sub-Tenon anesthesia in 109 patients, 76 of whom were having cataract surgery. The investigators reported chemosis involving one quadrant in 39.4% of patients and conjunctival hemorrhages in 56% of patients (35). The occurrence of chemosis is associated with the injection of higher volumes (2). The surgical approach to sub-Tenon anesthesia appears to be the technique of choice as an intraoperative supplemental injection when initial anesthesia is insufficient (2). In a prospective study of 6,000 surgical sub-Tenon blocks, Guise reported no serious complications—7% of patients with subconjunctival hematoma and 6% with subconjunctival edema (36). This approach offers greater safety by avoiding the blind insertion of a needle into the orbit.
the conjunctiva at the inferonasal quadrant, allowing the local anesthetic to spread circumferentially around the scleral part of the globe (see Fig. 19-19) (24). High-quality analgesia is produced with relatively low volumes (3–5 mL), and the use of higher volumes (8–11 mL) causes spread to the extraocular muscles, producing effective akinesia (25,26,27,28). Briggs and co-workers performed a comparative study between peribulbar and sub-Tenon anesthesia for cataract surgery. They conclude that sub-Tenon anesthesia reduces the overall level of discomfort associated with the administration of local anesthetic compared with the peribulbar method, in addition to providing superior intraoperative pain control (29). Several prospective studies have found that sub-Tenon anesthesia is as effective or better than retrobulbar injection for cataract surgery (30,31,32,33) or vitreoretinal surgery (34). Roman and co-workers investigated the complications associated with sub-Tenon anesthesia in 109 patients, 76 of whom were having cataract surgery. The investigators reported chemosis involving one quadrant in 39.4% of patients and conjunctival hemorrhages in 56% of patients (35). The occurrence of chemosis is associated with the injection of higher volumes (2). The surgical approach to sub-Tenon anesthesia appears to be the technique of choice as an intraoperative supplemental injection when initial anesthesia is insufficient (2). In a prospective study of 6,000 surgical sub-Tenon blocks, Guise reported no serious complications—7% of patients with subconjunctival hematoma and 6% with subconjunctival edema (36). This approach offers greater safety by avoiding the blind insertion of a needle into the orbit.
In recent years, topical anesthesia has become very popular for cataract surgery, being used in up to 50% of procedures in some series (7). However, intraoperative pain control appears to be more consistent when retrobulbar (37,38) or sub-Tenon anesthesia (39,40) is performed. Conversely, Johnston and colleagues, in a prospective study comparing topical and peribulbar anesthesia, report that topical anesthesia for phacoemulsification was well tolerated, but add that patient cooperation is an important factor in its success (41). In a prospective randomized comparison of peribulbar and topical anesthesia for cataract surgery, Sauder and Jonas (42) found that patient comfort and surgery-related complications did not differ between the two groups, and they recommend the use of topical anesthesia for routine cataract surgery. Ultimately, the use of topical anesthesia should be limited to uncomplicated surgery in cooperative patients. Topical anesthesia is inappropriate whenever phacoemulsification is not possible and total akinesia is required.
Intracameral injection of local anesthetic has been proposed as an adjunct to topical anesthesia but safety issues have been raised about local anesthetic toxicity to the corneal endothelium, which is incapable of regeneration. The American Academy of Ophthalmology in a report on intracameral anesthesia (43) recount the equivocal nature of studies investigating the effectiveness of the technique. It would appear that preservative-free lidocaine 1% is well tolerated by the corneal endothelium but that higher concentrations are toxic. They recommend the use of intracameral anesthesia for supplementary incremental analgesia for patients who cannot tolerate topical anesthesia alone. However, they stress that, although short-term studies seem to indicate safety, the long-term effects of intracameral anesthesia are unknown.
Neurosurgery
Neurosurgery under local anesthesia was originally introduced for surgical treatment of epilepsy during the 1930s. Regional anesthesia is performed to facilitate resection of abnormal brain tissue without damaging surrounding normal tissue. With the assistance of cortical mapping and a conscious patient, this goal can be readily achieved through observing the effects of stimulation on speech and movement areas. Another common procedure performed under local anesthesia is carotid endarterectomy (CEA).
Craniotomy
Requirements for craniotomy include sufficient depth of anesthesia during opening and closing of the bone flap, return to full consciousness during brain mapping, smooth transition between anesthesia and consciousness, as well as immobility and comfort throughout surgery (44). An asleep-awake-asleep technique is usually utilized (45,46).
A skull block involves regional anesthesia to the nerves that innervate the scalp, including the greater and lesser occipital nerves, the supraorbital and supratrochlear nerves, the zygomaticotemporal nerves, the auriculotemporal nerves, and the greater auricular nerves (Fig. 21-1; see also Figs. 17-2, 17-3, and 17-10) (47).
Girvin described his experience with local anesthesia for awake craniotomy using 60 mL of 0.33% bupivacaine with epinephrine 1:200,000 infiltrated into the scalp flap, plus an additional 12 mL of 0.5% bupivacaine for individual nerve blocks (48). More recently, a similar regional technique using ropivacaine up to 4.3 mg/kg with added epinephrine 5 μg/mL has been advocated to provide surgical anesthesia for awake craniotomy (49). Extensive blockade of the scalp bilaterally warranted minimal sedation, which the authors (49) suggest
contrasts with other recognized awake craniotomy techniques that require a period of general anesthesia prior to the wake-up period.
contrasts with other recognized awake craniotomy techniques that require a period of general anesthesia prior to the wake-up period.
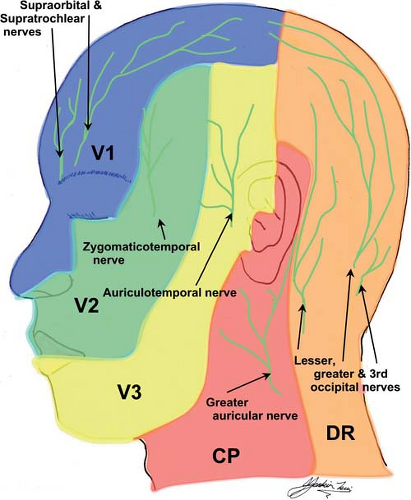 Figure 21-1. Skull block. Nerve block sites for regional anesthesia to nerves that innervate the scalp. |
Blanshard and co-workers reported retrospectively on the feasibility of performing craniotomy in awake patients for removal of intracranial tumors on an ambulatory basis. The investigators provided anesthesia using local infiltration with 2% lidocaine for insertion of the pins for rigid head fixation and 0.25% bupivacaine with epinephrine for the surgical incision. There was only one conversion to general anesthesia out of 241 patients. An overall morbidity rate of 32% was reported including neurologic, systemic, and regional complications. These results are comparable to those of a similar study of craniotomy under general anesthesia (50).
Pinosky advocates the use of a bupivacaine skull block to attenuate the hemodynamic response to craniotomy during general anesthesia (47). Insertion of cranial pins, incision, and periosteal–dural contact can result in tachycardia and hypertension, causing further increases in intracranial pressure (ICP) in patients with intracranial pathology and a higher risk of rupture of intravascular aneurysms. The requirement for additional anesthesia or vasoactive drugs was removed in patients who received a skull block with 0.5% bupivacaine.
The use of scalp nerve blocks has also been recommended to attenuate postoperative pain after craniotomy (51,52). Prospective studies report that 60% to 80% of patients experience moderate to severe pain after craniotomy (53,54). Data on the best analgesic method for this population are scarce. Intramuscular opioids or intravenous (IV) patient-controlled analgesia with morphine is associated with the side effect of sedation, which may be perceived as a neurosurgical complication. Nguyen and co-workers, in a prospective, randomized, and double-blind study reported on the successful use of a ropivacaine scalp block at skin closure, in patients undergoing supratentorial craniotomy (51). The supraorbital and supratrochlear nerves, auriculotemporal and postauricular branches of the greater auricular nerves, and the greater, lesser, and third occipital nerves were blocked using a total of 20 mL 0.75% ropivacaine. The analgesic effect lasted for 48 hours, as demonstrated using visual analog scale scores.
Blockade of the supraorbital and greater occipital nerves can facilitate frame placement during stereotactic neurosurgery (55). Watson and colleagues demonstrated that nerve blocks and subcutaneous infiltration provided comparable anesthesia for frame placement (56). Nerve blocks were less painful than infiltration at both frontal and orbital sites. Supraorbital nerve blocks were associated with more supplementation than either greater occipital nerve blocks or subcutaneous infiltration. Reasons given include straying of the frontal pin of the frame into the region supplied by the zygomaticotemporal nerve in addition to anomalous variation in the anatomy of the supraorbital nerve. The supraorbital nerve may exit the skull undivided, or its lateral and medial branches may exit separately. Failure to block the lateral branch may account for inadequate anesthesia during frame pin placement (57).
Carotid Endarterectomy
Carotid endarterectomy is the one of the most frequent surgical procedure performed to prevent ischemic stroke in patients with severe symptomatic stenosis (>70%–99%) of the extracranial internal carotid artery. A series of large, randomized controlled trials (ECST, NASCET) (58,59,60) have demonstrated the superiority of the procedure over medical therapy in this cohort, and it is of smaller but definite benefit in symptomatic patients with 50% to 69% stenosis (American Academy Neurology Therapeutics and Technology Assessment). However, the procedure itself carries an inherent risk of stroke and mortality, estimated at 5% to 7 % within 30 days of surgery. If the perioperative risks could be reduced, the benefits from CEA would be greater. Regional anesthesia for CEA has been favored by some practitioners for over two decades, but whether it reduces the incidence of these risks remains unproven.
A recent body of evidence suggests that morbidity and mortality may be reduced if CEA is performed under regional anesthesia. Cerebral protection during carotid cross-clamping and the signs that herald hypoperfusion are the principal surgical issues of concern. The use of carotid artery stump pressure measurement, electroencephalogram (EEG), and transcranial Doppler of the middle cerebral artery may be used either alone or in combination to determine which patients require insertion of an internal carotid artery shunt to bypass the carotid cross-clamp. However, these measurements are neither sufficiently sensitive nor specific to accurately detect hypoperfusion, and many patients have their blood pressure pharmacologically elevated during carotid cross-clamping in an effort to maintain perfusion.
The conscious patient having the procedure performed under regional block acts as his own monitor of the adequacy of cerebral perfusion throughout. Any change in speech, cerebration, or motor function indicates the need for immediate shunting. This facilitates the use of selective shunting—some surgeons use a shunt in all CEAs under general anesthesia. Studies (61,62,63) suggest a rate of shunting as low as 10% to 15% in procedures carried out under a regional procedure, which may improve morbidity, as shunting itself carries a risk of stroke (64).
Other advantages of a regional technique include lower cardiovascular morbidity (65), shorter ICU and overall hospital stays, and less expense (66). However, there is insufficient evidence from randomized trials comparing regional and general techniques to prove that one technique is superior to the other. Nonrandomized studies suggest potential benefits as outlined, but these studies may be biased (65).
Regional anesthesia for CEA requires blockade of the second (C2) to the fourth (C4) cervical dermatomes. This may be performed by using a superficial cervical plexus block, a combination of superficial and deep cervical plexus blocks, or, less commonly, by cervical epidural. Most practitioners appear to favor a combination of deep and superficial blocks. The deep block may be performed by single injection at C3 or C4, as described originally by Winnie and co-workers (67), or by the standard three-injection technique (see Fig. 17-11) (68).
Stoneham and colleagues compared the efficacy of superficial block alone with deep block alone (69). No differences were found between the blocks in terms of the amount of supplemental local anesthetic required, although this was influenced by the presence or absence of paresthesia during placement of the deep block. Paresthesiae occurring during deep cervical plexus block placement resulted in a more effective block. In two prospective randomized studies comparing superficial versus combined (superficial and deep) cervical plexus block, no differences were detected in terms of the need for supplemental local anesthesia (70,71). The deep branches of the cervical plexus supplying the neck muscles are not anesthetized with a superficial block. This in theory may lead to difficulty operating on deep structures because of the absence of neuromuscular block. However, there is little evidence to support this (72).
A number of case series support the use of cervical epidural anesthesia (73,74,75,76). However, there is a high incidence
of associated cardiovascular morbidity, respiratory failure requiring intubation in 1%, dural puncture in 0.5%, and alterations in pulmonary function in all recipients (66). Therefore its use is not widely advocated. A single-injection posterior cervical paravertebral block and interscalene cervical plexus block using a nerve stimulator have been successfully used (77,78).
of associated cardiovascular morbidity, respiratory failure requiring intubation in 1%, dural puncture in 0.5%, and alterations in pulmonary function in all recipients (66). Therefore its use is not widely advocated. A single-injection posterior cervical paravertebral block and interscalene cervical plexus block using a nerve stimulator have been successfully used (77,78).
Several potentially life-threatening complications may arise from deep cervical plexus blockade. These include vertebral artery, subarachnoid, or epidural injection. Phrenic nerve palsy leading to hemidiaphragmatic paresis (79) is a common occurrence and may lead to respiratory embarrassment in patients with underlying pulmonary disease. Other well-described complications include Horner syndrome (80,81), stellate ganglion block (66), and hoarseness due to recurrent laryngeal nerve block. There are a number of reports of complete respiratory obstruction due to preexisting contralateral recurrent laryngeal nerve block (82,83). There is no evidence to suggest that a single-injection technique is safer that a three-injection technique or vice-versa (67).
Common problems encountered during CEA usually relate to sedation or incomplete block. Intravenous sedation may lead to obtundation and hypoventilation or agitation. Small-dose IV clonidine may offer an advantage as an adjunct, as well as decreasing the incidence of postoperative hypertension (84). The most common reason for incomplete block is usually incisional pain near the midline mediated by contralateral fibers. Local anesthetic infiltration by the surgeon usually minimizes this problem. Occasionally, pain is experienced during dissection of the carotid sheath, pain which may be mediated by fibers from the ansa cervicalis or vagus nerves (72,85). Again, this is usually alleviated by local anesthetic supplementation. Pain caused by dissection high in the neck or by metal retractors is not prevented by cervical plexus block but may be ameliorated by performing a mandibular nerve block (86).
Surgery to the Oral Cavity and Nasopharynx
Interventional skills and mastery of the airway are crucial for all anesthesiologists, and airway blockade is one of most important regional blocks to perfect to accomplish these goals. Other common procedures in which regional anesthesia is useful include tonsillectomy and endonasal surgery.
Airway
Awake fiberoptic intubation is a well-established technique in the management of the anticipated difficult airway (87,88). Advantages of this technique of airway control include patient cooperation, spontaneous respiration throughout the procedure, and maintenance of airway patency through conscious control of the airway muscles (89). Several techniques for providing airway anesthesia have been described, including direct application of local anesthetics to the respiratory mucosa using sprays and nebulizers, as well as a variety of nerve blocks. Being airway experts and frequently called upon in the management of difficult airways, these techniques are extremely important for all anesthesiologists in their clinical practices.
A good working knowledge of the neuroanatomy of the nasal and oral cavities, the pharynx, larynx, and trachea is important when manipulating the airway in the awake state. The nasal cavity is entirely innervated by branches of the trigeminal nerve (90). The anterior parts of the nasal cavity and septum are supplied by the anterior ethmoidal nerve, which itself is a branch of the ophthalmic nerve. The remainder of the nasal cavity receives its innervation from branches of the maxillary nerve. The glossopharyngeal nerve provides sensation to the posterior third of the tongue, the fauces and tonsils, the epiglottis, and all of the pharynx. The superior laryngeal nerve arises from the vagus nerve before dividing into internal and external branches. The external branch provides motor innervation to the cricothyroid muscle. The internal branch provides visceral sensory and secretomotor innervation to the larynx above the vocal cords. The recurrent laryngeal nerve, also a branch of the vagus nerve, provides sensory innervation to the laryngeal mucous membranes inferior to the vocal cords and to the upper trachea. It provides motor innervation to all of the laryngeal musculature except the cricothyroid (91).
These nerves participate in a number of brainstem-controlled reflex pathways concerning airway protection (89). The gag reflex is initiated by mechanical and chemical stimulation of areas innervated by the glossopharyngeal nerve (92). A selective bilateral block of the glossopharynx can abolish conduction in the afferent limb of the gag reflex and greatly increase the chances of a successful awake intubation (93). The laryngeal closure reflex can be stimulated by irritation of the sensory area innervated by the internal branch of the superior laryngeal nerve. This reflex can be attenuated by either topical anesthesia or direct nerve blocks (93). The cough reflex is relayed by sensory afferents from the trachea and larynx in the internal branch of the superior laryngeal nerve and the recurrent laryngeal nerve. This can also be blocked by both direct nerve blocks and topical anesthesia (93). The cardiovascular reflex response to airway manipulation is hypertension, tachycardia, and bradycardia. Laryngeal and glottic receptors are responsible for increased sympathetic activity with stimulation of the airway mucosa. This is relayed to the brainstem via the corresponding cranial nerve innervating these areas. The cardiovascular response may be blocked by targeting mechanoreceptor stimulation using topical or regional anesthesia (93).
There is considerable debate in the literature about the most effective means of achieving adequate airway anesthesia. Topical anesthesia may be applied indirectly by spraying with a nebulizer or atomizer, or it may applied directly by swabbing, gargling, inhaling, or via the fiberoptic bronchoscope itself (89). The two most common local anesthetic techniques used to provide anesthesia are the superior laryngeal nerve block for the supraglottic larynx and the transtracheal injection for subglottic structures. The glossopharyngeal nerve block is very effective for obtunding the gag reflex but is not often used in clinical practice. Reasoner and co-workers compared topical anesthesia and nerve blocks for awake intubation in neurosurgical patients with cervical spine instability. Topical anesthesia was administered using nebulized 4% lidocaine (20 mL) and transtracheal injection of 4% lidocaine (3 mL). Nerve block patients underwent bilateral glossopharyngeal and superior laryngeal nerve blocks with 2% lidocaine in addition to a transtracheal injection of 4% lidocaine. They found no difference in patient perception of discomfort during the procedure (94). Similarly, Kundra and co-workers compared nebulized 4% lidocaine with combined superior laryngeal and transtracheal nerve blocks and demonstrated better patient comfort and hemodynamic stability with the combined nerve block technique. However, they failed to show a difference between the two groups with respect to intubating conditions (95). Conversely, Graham and colleagues reported better laryngotracheal anesthesia following translaryngeal injection of lidocaine when compared to nebulization.
Many authors recognize the potential for toxic plasma levels of lidocaine with topical application owing to the relatively large amounts of concentrated solutions used (95,96). It is believed, however, that a large amount of the drug is “wasted” (97), with one group working on the assumption that up to 75% of the nebulized drug is lost (98). The toxic plasma concentration of lidocaine is widely accepted as 5 mg/L (96,99,100,101), and side effects are reported to develop when concentrations reach 4 mg /L. Recent guidelines issued by the British Thoracic Society suggest the total dose of lidocaine applied during bronchoscopy should be limited to 8.2 mg/kg (101).
The glossopharyngeal nerve block can be performed by using either an intraoral or a peristyloid approach (102). If the intraoral approach is used, the patient must have sufficient mouth-opening so that visualization of the posterior tonsillar pillar is possible. Benumof (88) described the use of an anterior tonsillar pillar injection that has been advocated elsewhere because of better exposure to the anterior tonsillar pillar in cases of limited mouth opening and better patient tolerance (103). The peristyloid approach does not rely on reliability of mouth opening but requires access to the lateral neck and the ability to recognize bony landmarks (89) (see Fig. 17-8).
The internal branch of the superior laryngeal nerve may be blocked by either an anterior or a lateral approach (104). Furlan (104), in a study of 50 human cadavers, demonstrated the proximity of the superior laryngeal nerve to the greater cornu of the hyoid bone. The mean distance from internal superior laryngeal nerve to the greater horn of the hyoid bone in a craniocaudal direction was 2.4 mm. The lateral approach uses the greater cornu of the hyoid bone as the target from which the needle is directed inferiorly and advanced 2 to 3 mm, so that the tip rests between the thyrohyoid membrane laterally and the laryngeal mucosa medially (89) (Fig. 17-8). Using an anterior approach, the needle is walked in a cephalad direction off the superior cornu of the thyroid cartilage. Recognized complications include vasovagal response (105,106), which may be explained by spread of local anesthetic to the carotid bulb or the main trunk of the vagus.
Alternative uses for nerve blocks used in providing anesthesia for awake intubation have been described. Sulica and Blitzer reported using bilateral superior laryngeal nerve blocks and transtracheal injection to provide anesthesia for office-based laryngeal surgery including soft tissue biopsy and CO2 laser ablation of respiratory tract papilloma (105). Superior laryngeal blocks have been used in the treatment and prevention of laryngospasm and stridor (107) and to facilitate placement of transesophageal echocardiography probes (108,109).
Tonsillectomy
Post tonsillectomy pain can be severe and remains a significant obstacle to rapid recovery. The pain in adult patients is maximal in the first 5 days (110) and in children a return to normal activity and diet may take up to 12 days (111).
Reported benefits of local anesthetic techniques include diminished perioperative bleeding, postsurgical pain, and nausea in addition to improved surgical planes of dissection (112,113,114,115,116,117). However, there are numerous conflicting reports regarding the efficacy of regional anesthesia for post tonsillectomy analgesia.

Full access? Get Clinical Tree








