Nerve Mapping in Adults
William F. Urmey
Carlos A. Bollini
Fernando Cacheiro
Introduction
Nerve mapping in adults refers to the use of a surface stimulating electrode to outline the course of an underlying peripheral nerve or neural plexus. Nerve mapping can serve as a surrogate method to the use of conventional anatomical surface landmarks for the performance of peripheral nerve blocks. Conventionally, blocks of peripheral neural or plexuses have been performed following the identification of previously described or published surface landmarks, which serve as approximate starting points for invasive exploration with a block needle. Exploration with the block needle proceeds until the identification of an appropriate endpoint, following which injection of local anesthetic results in a high rate of success. Two types of such endpoints exist: 1) anatomical endpoints that rely on the identification of anatomical structures that are closely related to the nerve, and 2) functional endpoints that rely on neural function or response to mechanical or electrical stimulation by the block needle. Functional endpoints include mechanical paresthesia (sensory response to mechanical stimulation) as well as motor response to electrical stimulation, comprising the two most frequently utilized endpoints in peripheral or plexus blockade.
Designated anatomical landmarks simply serve as a starting point for invasive needle exploration, independent of the technique used. Anatomical landmarks have limitations. They vary from patient to patient, and are dependent on patient size or body habitus. Published anatomical landmarks often include measured angles and distances in centimeters that are not normalized or adapted to patient size or variations in anatomy. Such landmarks can only serve, at best, as an approximation.
Nerve mapping, in contrast to previously described anatomical landmarks, involves the use of electrical nerve stimulation and thus yields useful information prior to needle insertion. This allows for prelocalization of the targeted nerve or plexus prior to invasive search with the needle. Nerve mapping has in common with ultrasonography or other imaging techniques the ability to yield information noninvasively to facilitate nerve location. This chapter focuses on the science of nerve stimulation, in particular transcutaneous nerve stimulation for nerve mapping or prelocation of nerves in adults. The recently published technique of indentation percutaneous electrode guidance (PEG) of the block needle will be discussed as it applies to enhancement of the concept of nerve mapping and subsequent final location and injection of the targeted nerve or plexus.
History
Luigi Galvani first demonstrated that an electrical charge could result in an electrical stimulation and resulting muscular contraction in 1780. However it was not until 1850 when the underlying physiology was studied in depth by Von Helmholtz, who performed numerous experiments using isolated nerve/muscle preparations. In 1912, Perthes described the technique of electrical stimulation using a selective peripheral nerve stimulator with a nickel-insulated needle to assist in regional anesthetic neural blockade. Although there was strong interest in regional anesthesia and anesthetic techniques in the beginning of the twentieth century, this interest faded for a period. A resurgence in regional anesthetic techniques occurred later in the century, which has increased dramatically to the present day. In 1955, Pearson was the first to use an insulated needle to successfully locate motor nerves by electrical stimulation. In 1962, Greenblatt and Denson used a self-built electrical nerve stimulator to assist in peripheral nerve and plexus blocks. They demonstrated that the motor component of mixed nerves could be stimulated without causing pain. In 1969, Magora, using an electrical stimulator with an ammeter, determined that 0.5 mA was a suitable stimulation threshold for successful blockade of the obturator nerve. In 1980 Raj et al. re-introduced the idea of nerve stimulation to assist in the performance of peripheral nerve blocks, ushering in the modern era of the electrical nerve stimulator. A review article was published in 1985 by Pither, et al. that covered the experience to that date of the use of electrical nerve stimulators in regional anesthesia, focusing on the characteristics of nerve stimulators, needles, basic science, clinical technique, and applications of the techniques.
In 1993, Ganta and colleagues reported on the use of a modified electrocardiographic electrode with coupling gel that was used to assist in the performance of interscalene block by prelocation of the brachial plexus using transcutaneous stimulation. In 2002, Urmey and Grossi first described the technique of percutaneous electrode guidance. These investigators used a cylindrical electrically shielded cutaneous electrode to map nerves by transcutaneous stimulation as well as to guide the block needle to the targeted nerve by indentation of the skin using the cylindrical electrode. Also in 2002, Bosenberg and colleagues published a report that many superficial peripheral nerves can be “mapped” prior to skin penetration by transcutaneous stimulation in the 2 to 3.5 mA range. In 2003, Hadzic, et al. analyzed the characteristics of a large number of various commercially available nerve stimulators using an oscilloscopic analysis of the resulting square waves. In 2004, the same investigators examined the significance of anatomical placement of the ground lead as well as the relationship between the electrical pulse amplitude (amperage) and pulse duration. In 2006, Urmey and Grossi published the technique of sequential electrical nerve stimulation, which used a series of alternating pulse durations to increase feedback or information—motor responses—at a distance from the nerve.
Scientific Principles of Electrical Nerve Stimulation
The method of peripheral nerve stimulation for nerve location involves the use of a peripheral nerve stimulator; that is, a direct current (DC) “square-wave” impulse generator. Peripheral nerve stimulators typically supply a constant electrical current, the frequency (Hz), amplitude (mA), and pulse duration (ms) of which can be manipulated in order to assist in location of motor or mixed motor/sensory nerves. Depolarization of the nerve depends on the distance from the electrical field generated at the tip of the stimulating microelectrode needle, the electrical charge, and the stimulation threshold of the targeted nerve. Depolarization and the resulting action potentials will elicit a motor response and movement of varying intensity.
The peripheral nerve stimulator (PNS) consists of four essential components: an oscillator, a constant current generator, a display, and capabilities to control stimulus, intensity, duration, and frequency. The most modern stimulators involve a microprocessor
that is programmed to control these parameters and ensure their accuracy. Most modern units are constant current generators that ensure accurate delivery of a constant current in the face of changes in electrical impedance that occur between anode and cathode.
that is programmed to control these parameters and ensure their accuracy. Most modern units are constant current generators that ensure accurate delivery of a constant current in the face of changes in electrical impedance that occur between anode and cathode.
In order to stimulate a nerve a certain charge threshold must be achieved. The electrical charge applied to the nerve is a product of the current amplitude (mA) and the pulse duration in milliseconds (ms). The threshold for stimulation of the nerve is quantified by the rheobase and chronaxie of the nerve. The characteristic rheobase of a nerve (Fig. 4-1) is the lowest current amplitude with long or indefinite pulse duration applied to depolarize a nerve. Chronaxie is the pulse duration at which the threshold current amplitude is twice that of the rheobase. A pulse duration longer than the chronaxie is not desired because current consumption is increased without decreasing the threshold significantly.
The formula
I = Ir (1 + C/t)
where I = current amplitude, Ir = rheobase, C = chronaxie, and t = pulse duration, illustrates that the current amplitude necessary for nerve stimulation is very dependent on the pulse duration of the stimulus. Larger fibers are more easily stimulated than smaller fibers. Large motor fibers can be stimulated with pulse durations as low as 0.05 ms with very little discomfort.
Nerve Localization
Nerve localization has been achieved by following previously described surface anatomical landmarks. Such landmarks have been widely published and underlie the various techniques used for regional anesthetic blocks. Surface landmarks have been described for many different peripheral nerves or plexuses of nerves. Following identification of landmarks, a block needle has been used to search for a distinct endpoint with the objective of putting the needle tip in the immediate vicinity of the targeted nerve or nerves. Two categories of endpoints exist in practice. Anatomical endpoints are dependent on intimate anatomical relationships of other structures to the targeted nerve or nerves. Examples of regional anesthetic techniques that utilize anatomical endpoints include transarterial or periarterial techniques for brachial plexus block, field blocks, or the use of imaging techniques such as ultrasonographic guidance. Functional endpoints, by contrast, require neural function; that is, a neural response to mechanical or electrical stimulation. The two major functional endpoints that have been used in clinical practice include: 1) a sensory response to mechanical stimulation (i.e., a mechanical paresthesia), and 2) a motor response to electrical stimulation (i.e., a muscular twitch).
The use of motor responses to electrical stimulation has dominated the field of regional anesthesia in recent years. The major difference between the use of a motor response to electrical stimulation and a mechanical paresthesia is that the motor response is a graded phenomenon that yields information about nerve location from a distance, whereas a mechanical paresthesia is an all-or-nothing response requiring contact with the nerve. A mechanical paresthesia supplies no information at distance from the nerve.
Optimal Use of A Peripheral Nerve Stimulator for Nerve Location
A peripheral nerve stimulator utilizes an oscillating rectangular wave current generator. By altering the time base on an oscilloscope, these waves can be graphed as “square-waves”; therefore, nerve stimulators are referred to as square-wave generators. These square waves or “pulses” are programmed to occur at a given frequency, typically 1 to 2 Hz (1 to 2 cycles/sec). Most commercially available nerve stimulators today are constant current generators that deliver accurate pulses of electrical current in the face of varying tissue impedances (resistances, capacitances, and inductances). The newest commercially available peripheral nerve stimulators are capable of producing electrical pulses of accurate duration in the 0.1 to 1.0 ms range. They have the capability of continuously and accurately controlling electrical current amplitude in the range of 0 to 5 mA. Armed with modern peripheral nerve stimulators, the regional anesthesia practitioner is able to control the following variables during nerve location: 1) electrical pulse frequency, 2) current amplitude (amperage), 3) electrode conductive area, 4) electrical pulse duration, and 5) tissue electrical impedance.
Electrical Pulse Frequency
The most commonly utilized electrical pulse frequency during peripheral nerve stimulation is 2 Hz. This frequency is the same as that used during train-of-four stimulation used to monitor the degree of motor blockade during general anesthesia. Although most stimulators allow 1 Hz stimulation, 2 Hz stimulation results in more rapid feedback, thus serving to decrease the amount of time required for nerve location. Frequency can be increased above 2 Hz, but above 4 Hz there is inadequate time for the relaxation phase of the action potential, which results in sustained tetanus. Therefore, 1, 2, or 3 Hz are acceptable frequencies during neural location.
Current Amplitude
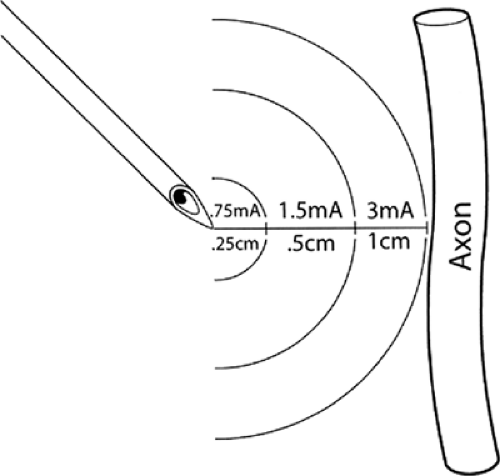
Electrical current transmission between 2 electrodes in a homogeneous medium of constant impedance follows what is commonly referred to as the “inverse square law.” The
relationship between required electrical current was first understood and described by Coulomb in the 1780s. The relationship between the required electrical current to stimulate a nerve and the distance to the nerve follows Coulomb’s law:
relationship between required electrical current was first understood and described by Coulomb in the 1780s. The relationship between the required electrical current to stimulate a nerve and the distance to the nerve follows Coulomb’s law:
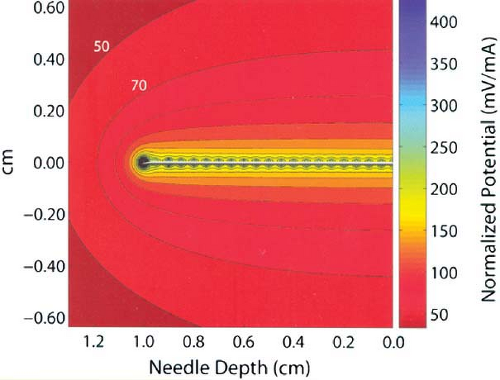 Figure 4-2. As shown in this computer model of an electrical field surrounding a block needle used in nerve location, electrical current dissipates very quickly from the tip of the needle to the inverse square of the distance from the needle tip. Movement of the needle tip just a few millimeters away from the nerve may require several-fold current increases to achieve similar motor response to electrical stimulation. (Reprinted with permission from Johnson CR, Barr RC, Klein SM. A computer model of electrical stimulation of peripheral nerves in regional anesthesia. Anesthesiology 2007;106:323–330.)

Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|