Chapter 66
Necrotizing Fasciitis and Related Soft Tissue Infections
Soft Tissue Infections
Layers of Soft Tissue
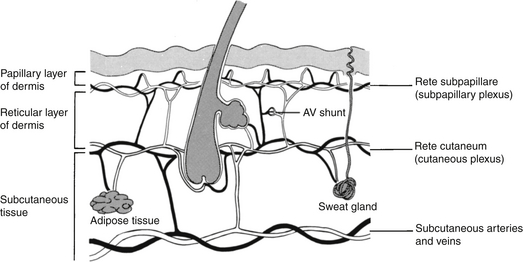
The skin is a two-layer membrane consisting of the epidermis and dermis. These layers are tightly fused above the subcutaneous tissue. When intact, the skin presents an almost impenetrable barrier to microorganisms. However, skin damaged by trauma or disease does not provide nearly as effective a defense. The blood supply of the skin runs horizontally at the junction of the dermis and subcutaneous tissue (Figure 66.1), and it is crucial for maintaining the skin’s integrity.
The deep fascia is a layer of strong connective tissue that overlies and separates major muscle groups. Where present, the deep fascia effectively deters the spread of infection from the superficial fascia into the muscle. Infection that extends to this layer and spreads within the fascial cleft is often termed fasciitis. Where the deep fascia is absent, for example, in the face and scalp, superficial infections can quickly spread into deeper tissues.
Pathogenesis
Another factor leading to the severity of some NSTIs is the contribution of exotoxins from some of the causative organisms. Clostridial infections are complicated by α-toxin, which causes tissue destruction and hemodynamic instability. Infections by Staphylococcus aureus and streptococcal species are complicated by a plethora of toxins. M-surface proteins enhance the bacteria’s tissue adherence and ability to evade host defenses. Exotoxins A and B cause capillary leakage and impaired blood flow. Streptolysin O and superantigen lead to a hyperinflammatory response resulting in severe sepsis or septic shock, which is often unrecoverable.
Thrombosis of deep blood vessels of the affected area is a hallmark of NSTI. However, the skin is able to receive its blood flow largely from the skin around it via the horizontal vascular plexus in the deep dermis (see Figure 66.1), rather than from the tissue beneath, leading to the NSTI’s often underwhelming external appearance.
Clinical Manifestations and Differential Diagnosis
Skin Infections
Most infections confined to the skin are caused by streptococcal and staphylococcal infections. Examples of these types of infections, nonspecifically called pyodermias, include impetigo, ecthyma, and erysipelas (Table 66.1).
TABLE 66.1
Soft Tissue Layers and Infections
| Layer Involved | Infection | Causative Bacteria and Comments |
| Skin | Impetigo | Staphylococcus (bullous form) |
| Group A Streptococcus pyogenes (epidemic form) | ||
| Skin | Ecthyma | Deeper form of impetigo |
| Skin | Erysipelas | S. pyogenes; has distinct violaceous border |
| Skin | Pyoderma | Pseudomonas aeruginosa; typically in immunocompromised hosts; “pyoderma gangrenosa” is a blue-red ulcer surrounding a necrotic base |
| Skin | Embolic ulcers | P. aeruginosa and S. aureus |
| Superficial fascia (Subcutaneous tissue) | Cellulitis | S. pyogenes, usually without preceding trauma; gram-negative bacilli and anaerobes occur with cellulitis resulting from bowel perforations or animal/human bites (see text) |
| Fascial cleft and deep fascia | Necrotizing fasciitis | Clostridial species; mixed aerobes-anaerobes; Vibrio species, S. pyogenes |
| Muscle | Myonecrosis | Clostridial species and other mixed aerobes-anaerobes can produce subcutaneous gas; group A beta-hemolytic S. pyogenes (so-called flesh-eating bacteria) causes necrotizing fasciitis with myonecrosis |
| Abscess | S. aureus; associated with less pain or systemic toxicity; usually occurs after trauma |

Full access? Get Clinical Tree