Neck Trauma
Tiffany K. Bee
Martin A. Croce
Injuries to the neck can cause morbidity and mortality. Initial evaluation and management differ depending on the mechanism of injury. This chapter will discuss the evaluation and management of penetrating and blunt neck injuries.
Anatomy: The neck encompasses the area bounded superiorly by the base of the mandible and a line running from the angle of the mandible to the mastoid process of the skull base, inferiorly by the clavicle, anteriorly by the anterior median line that includes the cricoid cartilage and posteriorly by the anterior margin of the trapezius.
The neck contains a diversity of vital structures in a relatively small space. Vital portions of many organ systems are represented in the neck.
Respiratory
Trachea
Larynx
Cardiovascular
Carotid arteries
Jugular veins
Vertebral arteries
Neurologic
Cervical spinal cord
Vagus nerve
Phrenic nerve
Recurrent Laryngeal nerves
Digestive
Pharynx
Esophagus
Endocrine
Thyroid
Parathyroids
Musculoskeletal
Spine and its ligaments
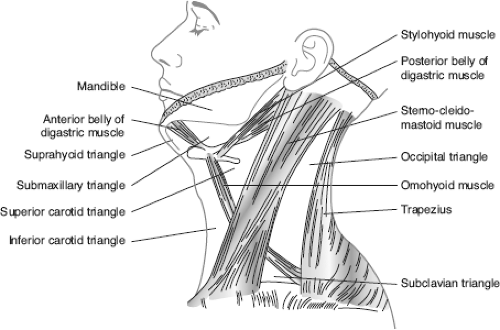
Historically, the neck is divided into triangles mainly by muscle location. The anterior triangle is bounded by the median line of the neck anteriorly, the anterior margin of the sternocleidomastoid muscle laterally, the inferior portion of the mandible superiorly, and the clavicles and manubrium inferiorly. The posterior triangle is bounded by the sternocleidomastoid muscle anteriorly, the anterior edge of the trapezius posteriorly, the middle third of the clavicle inferiorly and superiorly between the attachment of the sternocleidomastoid and trapezius to the occiput (Fig. 27-1).
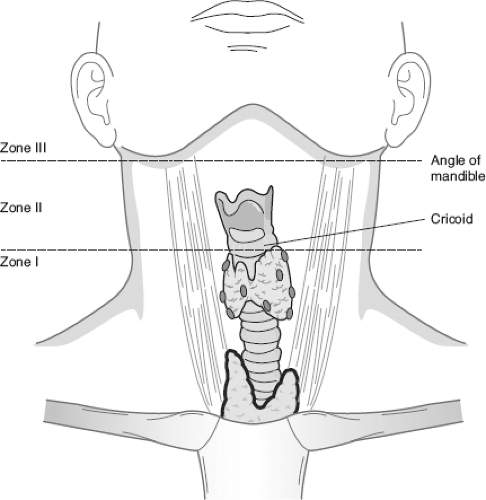
The neck is divided into zones in trauma situations (Fig. 27-2).
Zone I: Clavicle to cricoid injuries. Structures include the lung apices, trachea, brachiocephalic vein, subclavian artery, common carotid artery, thoracic duct, cervical nerve roots, and esophagus.
Zone II: Cricoid to angle of the mandible. Structures include common carotid and vertebral arteries, jugular veins, esophagus, thyroid, cervical spine, pharynx, trachea, and larynx.
Zone III: Angle of mandible to skull base. Structures include external carotid and internal carotid arteries, vertebral arteries, jugular veins, salivary glands, cranial nerves IX–XII, and hypopharynx.
Penetrating Neck Injury
I. Introduction
No longer is platysmal penetration an absolute indication for neck exploration. Instead, diagnostic testing and observation is used in many cases absent of signs of vascular or aerodigestive disruption and with hemodynamic stability. A major vascular injury may be easily identified but injury to the aerodigestive, neurologic, or musculoskeletal system may be more difficult to identify, but is nonetheless life-threatening. A multidisciplinary approach to these injuries is often necessary bringing in the expertise of trauma surgeons, interventional radiologists, ear, nose, and throat surgeons, plastic surgeons, neurosurgeons, and oral maxillofacial surgeons.
II. Initial Evaluation
A systematic evaluation should be performed. A rigid cervical collar is not necessary unless blunt trauma occurred or neurologic signs or symptoms are present. The “ABCD” evaluation, well described in the initial trauma evaluation, is the cornerstone in initial care.
Immediately operate on those patients with severe active bleeding, hemodynamic instability, expanding or pulsatile neck hematoma, massive subcutaneous air, or air bubbling from wound.
Patients without indication for immediate operation should undergo a primary survey then followed by a full secondary survey:
Inspection-evaluate for hematoma, platysmal penetration (do not probe wound), crepitance, stridor, hoarseness, odynophagia, dysphagia, or tracheal deviation.
Auscultation-listen for a bruit, bilateral breath sounds.
Palpation-feel for a thrill along vessels or subcutaneous emphysema. Determine pulse examination.
Chest radiograph-check for pneumo or hemothorax, pneumopericardium, retropharyngeal air, enlargement of superior mediastinum, or apical cap.
III. Diagnostic Testing
In the hemodynamically stable patient, further evaluation can determine injury. Patients who have dysphonia, dysphagia, retropharyngeal air, odynophagia, hemoptysis, hematemesis, or slight pulse discrepancy require further diagnostic testing. Some centers advocate observation alone if none of the above signs is present. This can vary by institution. At our institution the algorithm in Figure 27-3 is used for penetrating neck injury patients.
Diagnostic testing options available include
Four-vessel angiography, esophagography with or without laryngotracheobronchoscopy (if subcutaneous emphysema or retropharyngeal air). This method is accurate but does put the patient at risk for morbidity due to angiography.
Color flow Doppler imaging. This can aid diagnosis of vascular injury.
Helical CTA. CTA technology is quickly becoming the choice of modalities to detect vascular injury. It may not be reliable for esophageal injury detection, although any retropharyngeal air should trigger further investigation.
Esophagography and esophagoscopy. Contrast esophagography under fluoroscopic guidance has a sensitivity of nearly 90%. Use of barium instead of water-soluble contrast to distend the esophagus is beneficial. Many authors are now reporting good results with flexible esophagoscopy as well.
Observation and physical examination. This may be adequate for vascular injuries in zone II. However, the zone I and III vascular injuries may be missed by physical examination alone. Also esophageal injuries are difficult to determine by physical examination.
IV. Surgical Management of Specific Injuries
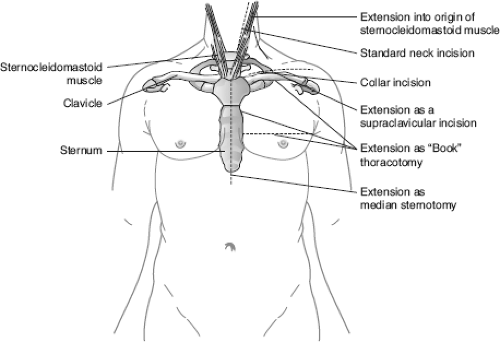
The patient should be positioned supine with the neck extended and rotated opposite the injury side (assuming the cervical spine is cleared). The patient should be prepped earlobe to umbilicus with special attention to the same side lateral chest. A portion of the thigh for a possible saphenous vein graft should also be included.
Vascular injury approaches (Fig. 27-4)
Carotid
Ascertain neurologic status. If patient is comatose but has prograde flow or significant back bleeding, attempt repair. If the patient is neurologically intact, attempt repair. If the patient is unstable, ligation may be necessary.
Obtain exposure by an anterior sternocleidomastoid incision. High carotid injuries may require anterior subluxation of the mandible or division of the omohyoid and digastric muscles. Placement of a Fogarty catheter into the distal artery may also help with bleeding control.
Repair can often be done primarily with some additional length gained by dividing the superior thyroid artery. If the defect is longer than 2 cm, use a saphenous vein graft. Transposition of the external carotid to the internal carotid artery is another option. Prosthetic grafts do not have good patency and should not be used.
Innominate and proximal subclavian arteries
Expose the proximal right subclavian artery and innominate artery through a median sternotomy. A proximal left subclavian artery is approached through a left thoracotomy, although a “trap-door” incision that combines a left anterolateral thoracotomy with a partial median sternotomy and left supraclavicular incision may be needed to fully expose. Resection of the medial clavicle to visualize the thyrocervical trunk helps. In unstable patients, ligate the subclavian artery distal to the take off of the vertebral artery.
Vertebral artery
In a patient with vertebral artery injury, treatment options include surgical ligation or radiologic embolization. Ligate through the C1–C2 interspace for the distal vertebral or a supraclavicular incision with medial clavicle removal for the proximal vertebral.
Venous injury
Ligation is the management of most venous injuries unless easily repaired.
Full access? Get Clinical Tree