Musculoskeletal Pain
Pain in the Shoulder
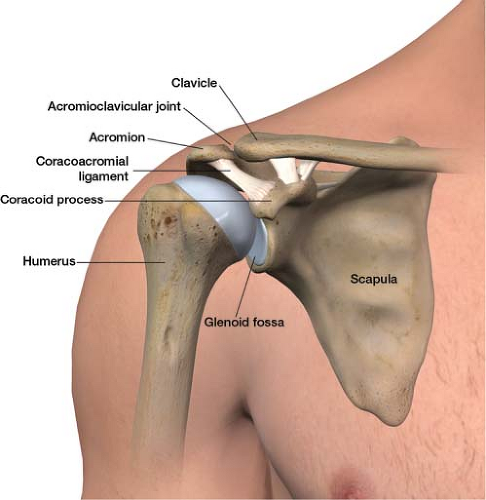
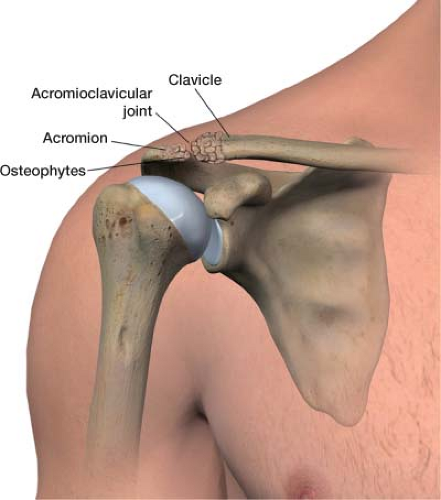
The shoulder is a common location of pain. In this ball-and-socket joint, the ball is the top, rounded part of the humerus, and the socket is the outer edge of the scapula (the glenoid fossa, Fig. 1-1). The joint is held together by muscles, ligaments, and tendons. The ball is too big for the relatively flat socket. This design allows the shoulder to be the most movable joint in the body but at the same time most prone to dislocation. Pain can come from the shoulder joint itself or may be
referred—from diseases affecting the gallbladder, heart, or cervical spine.
referred—from diseases affecting the gallbladder, heart, or cervical spine.
This section will focus on common sources of chronic pain originating from the shoulder itself. They include (1) bursitis, (2) arthritis—both glenohumeral and acromioclavicular (AC), (3) rotator cuff injury, and (4) adhesive capsulitis (frozen shoulder).
Bursitis
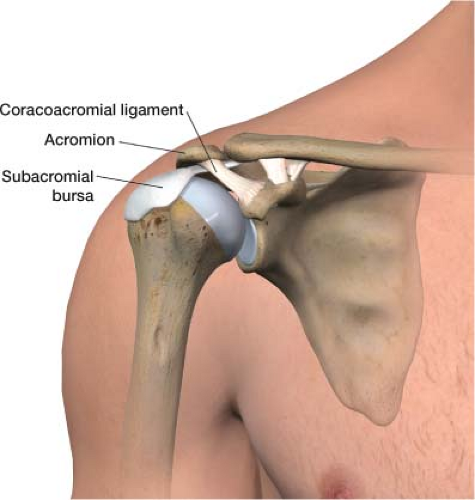
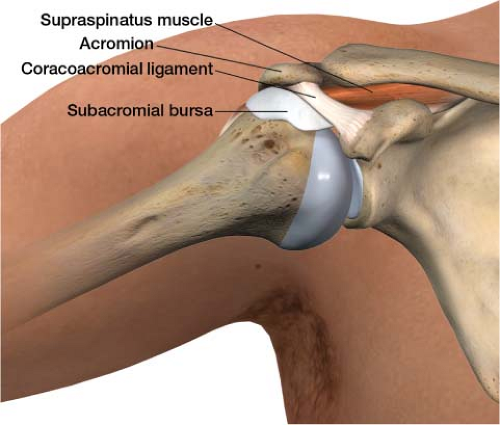
A bursa is a, fluid-filled sac that functions as a gliding surface to reduce friction between tissues of the body. The major bursa of the shoulder is the subacromial bursa. The shoulder’s subacromial bursa (Fig. 1-2) separates the supraspinatus tendon (one of the four tendons of the rotator cuff) from the coracoacromial ligament. When the arm is resting at the side, the bursa lies laterally below the acromion. When the arm is abducted, it moves medially beneath the acromion (Fig. 1-3). When subjected to increase friction and overuse the subacromial bursa can become inflamed. Pain is usually of slow onset. Discomfort occurs in the shoulder or upper arm at the site of the bursa. On examination, the pain is worse when the patient abducts the arm, specifically from 70 to 100 degrees.
Treatment involves rest and a nonsteroidal anti-inflammatory drug (NSAID). A cortisone injection at the bursa effectively reduces inflammation and pain.
Arthritis
Glenohumeral
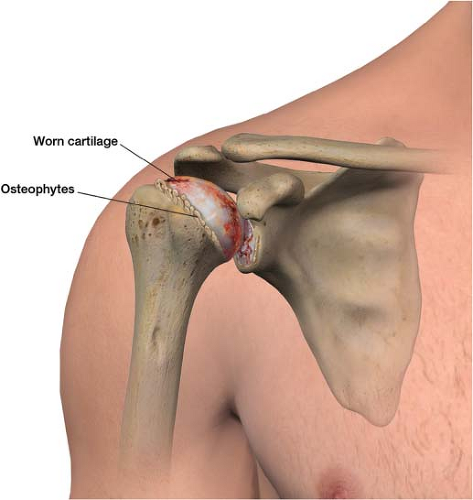
The primary cause of osteoarthritis is normal wear and tear. It can also occur when a significant trauma disrupts the cartilage covering the proximal humerus. In osteoarthritis, the joint surface degenerates and the subchondral bone remodels,
leading to pain and decreased range of motion (Fig. 1-4). Patients describe the pain as slowly progressive, diffuse, and deep in the joint; movement makes it worse. Physical examination may reveal crepitus and, in advanced cases, decreased range of motion. Radiography may show only subtle changes to the bone in a patient with clinical manifestations of pain from arthritis. Until there is more advanced destruction, x-ray results may be underwhelming. Magnetic resonance imaging (MRI) can provide greater evidence of articular cartilage wear.
leading to pain and decreased range of motion (Fig. 1-4). Patients describe the pain as slowly progressive, diffuse, and deep in the joint; movement makes it worse. Physical examination may reveal crepitus and, in advanced cases, decreased range of motion. Radiography may show only subtle changes to the bone in a patient with clinical manifestations of pain from arthritis. Until there is more advanced destruction, x-ray results may be underwhelming. Magnetic resonance imaging (MRI) can provide greater evidence of articular cartilage wear.
Painful symptoms are treated with NSAIDs and/or a cortisone injection and physical therapy. If conservative means do not control the shoulder pain, shoulder replacement may be a proper treatment option.
Acromioclavicular
Arthritis in the shoulder can also develop between the acromion and the clavicle (Fig. 1-5). The AC joint is superior to the glenohumeral junction. On examination, to elicit AC joint pain, have the patient bring the affected arm across the chest, which compresses the AC joint.
Treatment of AC arthritis is the same as for glenohumeral arthritis except that the cortisone injection is placed into the AC joint.
Rotator Cuff Injury
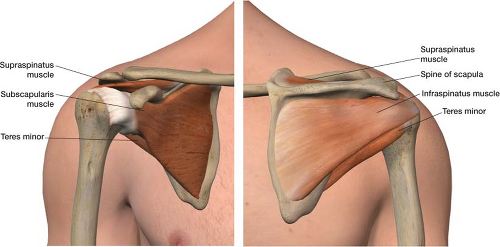
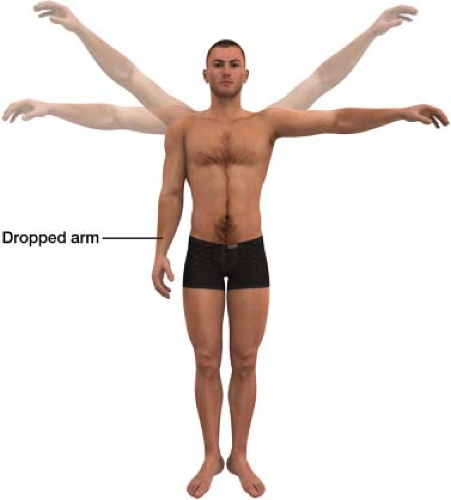
The rotator cuff is a group of four tendons that attach the scapula to the humerus: The supraspinatus, infraspinatus, teres minor, and subscapularis. They form a “cuff” over the posterior aspect of the proximal humerus (Fig. 1-6). The supraspinatus tendon is most frequently involved in tears. Rotator cuff injuries span a spectrum of pathologies, from mild tendinitis to massive tears. Younger patients usually report a history of trauma, whereas older patients present with a gradual onset of shoulder pain. They often describe pain as being located over the posterior aspect of the shoulder; overhead activities make it worse. The drop arm test helps detect rotator cuff pathology: The patient fully abducts the arm in the extended position (Fig. 1-7). The patient is asked to slowly lower the arm to the side. If the patient is not able to lower the arm slowly and smoothly to the side, it may be because of rotator cuff dysfunction. MRI is the imaging technique of choice.
NSAIDs and muscle relaxants remain the first-line symptomatic treatment. Physical therapy is also important. It may be necessary to consider a corticosteroid injection to decrease pain and inflammation as well as allow further advancement in physical therapy treatment. The patient should limit activity that involves high-tensile loads for 2 weeks after injection, because the tendon is potentially at risk for further tearing; common daily activities are not limited. Whether to proceed with surgical repair of the rotator cuff depends on the age, activity level, and functional needs of the patient.
Adhesive Capsulitis
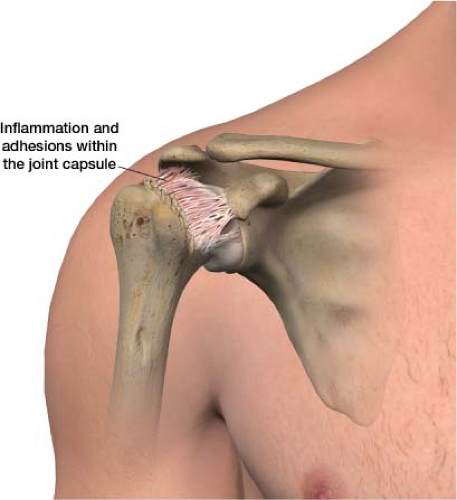
In adhesive capsulitis, abnormal bands of fibrous tissue grow within the joint capsule. There is also a lack
of synovial fluid, which lubricates the joint (Fig. 1-8). This condition affects about 2% of the general population and occurs most frequently in women between the ages of 40 and 70. It affects 10% to 15% of people with diabetes. This disorder is characterized by a restricted range of motion and pain. It is known to develop after a shoulder is injured or immobilized for an extended period of time. Arthrography shows diminished joint volume. Routine radiographs are generally normal.
of synovial fluid, which lubricates the joint (Fig. 1-8). This condition affects about 2% of the general population and occurs most frequently in women between the ages of 40 and 70. It affects 10% to 15% of people with diabetes. This disorder is characterized by a restricted range of motion and pain. It is known to develop after a shoulder is injured or immobilized for an extended period of time. Arthrography shows diminished joint volume. Routine radiographs are generally normal.
Muscle relaxants in combination with an opioid can be helpful. Physical therapy is useful. Cortisone injections with a local anesthetic usually allow the patient to participate more fully in physical therapy. However, because the joint space is so narrow, insertion of medication into the joint can be difficult. Therefore, a suprascapular nerve block may be advisable. The suprascapular nerve provides both motor and sensory innervation to the shoulder. Blocking this nerve alleviates pain so that physical therapy is less of a problem. If participation in physical therapy is limited, even with a pre-physical therapy shoulder injection or suprascapular nerve block, gentle manipulation under anesthesia to increase range of motion may be necessary.
Pain in the Elbow
Tendinitis
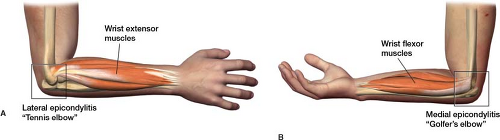
Lateral Epicondylitis (tennis elbow)
Tennis elbow is an idiopathic condition of middle-aged people in which the outer part of the elbow becomes painful and tender (Fig. 1-9). It is commonly associated with playing
tennis, although the condition can occur in nontennis players. The lateral epicondyle is the site of origin of the wrist extensor muscles. Gripping and resistance to wrist extension movement are painful.
tennis, although the condition can occur in nontennis players. The lateral epicondyle is the site of origin of the wrist extensor muscles. Gripping and resistance to wrist extension movement are painful.
NSAIDs combined with a brace to reduce strain at the elbow epicondyle is the treatment of choice. A counterforce tennis elbow strap can reduce tension of the muscles as they attach to the lateral epicondyle, especially the carpi radialis brevis. A cortisone injection can be beneficial.
Medial Epicondylitis (golfer’s elbow)
This syndrome is analogous to lateral epicondylitis and involves the wrist flexors on the medial side of the elbow (Fig. 1-9). Pain is exacerbated by offering resistance to wrist flexion.
Treatment is the same as for tennis elbow.
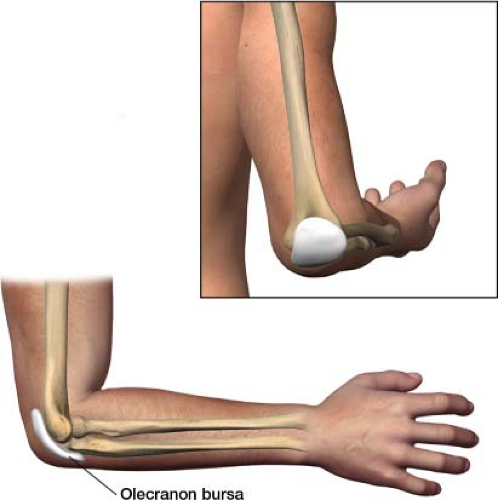
Olecranon Bursitis
The olecranon bursa is a fluid filled sac that lies on the back of the elbow to allow smooth movement of the joint (Fig. 1-10). When the bursa becomes inflamed, it fills with extra fluid and causes pain at the back of the elbow, often accompanied by noticeable swelling at the bony part of the elbow.
An NSAID and a compression bandage are usually all that is necessary. If this is insufficient, the next step is a simple in-office procedure: Drainage of fluid and an injection of cortisone at the bursa followed by a compression bandage.
Traumatic Arthritis
Osteoarthritis is more common in weight-bearing joints, such as the hips or knees. Traumatic arthritis is common in non–weight-bearing joints such as the elbow. The cause is a previous injury—a dislocation or fracture. Patients commonly complain of a locking or grinding sensation.
NSAIDs are usually the treatment of choice, with cortisone injections when needed.
Pain in the Neck (Cervical Spine)
The common sources of pain in the cervical spine are the same as those in the lumbar spine. The treatment algorithms are typically the same as well.
Pain in the Lower Back (Lumbar Spine)
Isolated low back pain is a complaint all practitioners face. In the majority of patients, the pain usually resolves on its own. A patient may need supportive treatment such as over-the-counter Tylenol or ibuprofen for a couple of days until the pain subsides. However, there are people who suffer from low back pain that does not resolve with time and over-the-counter medication. For these patients, it can be difficult to pinpoint the exact cause of chronic low back pain.
Although there is a limit to practitioners’ understanding of certain types of pain, this does not mean that patients do not experience them. It is usually possible to tease out a generator or multiple generators of a patient’s low back pain. There are specific treatment modalities tailored to specific pain generators. As long as practitioners understand pain generators well, they can properly treat back pain.
Four of the main generators of isolated low back pain are (1) muscle and ligaments, (2) vertebral bodies, (3) facet joints, and (4) vertebral discs. A patient may have one of these four as the source of low back pain or a combination of more than one. Low back pain that radiates into the leg is usually caused by compression or inflammation of a lumbar nerve root. This is covered in Chapter 2, Neuropathic Pain.
Muscles and Ligaments
Myofascial pain is probably the most common reason for isolated low back pain. Axial load is the tension administered along the spine when force is applied. The highest percentage of axial weight is carried in the lower back. With increased tension patients may develop muscle spasm (a painful and involuntary muscular contraction) or strain (an acute tearing injury to muscle). These pathological changes can become chronic. Muscle changes include the formation of taut muscle bands, painful taut muscle bands are known as trigger points (Fig. 1-11). Trigger points are thought to exist because of an abnormal neuromuscular junction, which is where the nerve and the muscle connect. This junction is a hyperexcitable region, where each strand of muscle tissue gets information on when to contract. If this charged region becomes overexcited, the muscle remains contracted. Actin and myosin strands remain pulled over each other in a pathological full contraction. A good analogy for visualizing this is the effect of static cling on pants. Too much electric charge causes pants to become bunched up in certain regions whereas sitting flush in others. With careful palpation trigger points may be palpated, an increase in muscle tone is detected.

Full access? Get Clinical Tree