Immediate Management of Life-Threatening Conditions
Evaluate the patient’s entire airway with direct visualization while maintaining immobilization of the cervical spine (C-spine) with a cervical collar. The patient should remain fully immobilized until spinal column injury is ruled out.
Diligent continuous monitoring of the airway should be performed for any patient with significant maxillofacial or neck trauma, as airway compromise can be abrupt. Keep a low threshold for intubation of any patient with impending airway obstruction. Soft tissue swelling and edema may result in delayed airway compromise. Warning signs include hoarseness, subcutaneous emphysema of the neck, laryngeal pain, visible edema, or the presence of an expanding hematoma.
Perform a jaw thrust to allow for ventilation while aggressively clearing and suctioning the obscuring material. The chin lift maneuver is contraindicated in any patient with potential cervical spinal trauma. Rapid-sequence intubation (RSI) with in-line C-spine stabilization is the preferred method of securing an airway in any patient without contraindications. Avoid using paralytics if the patient’s facial trauma might preclude successful bag-valve-mask ventilation. Intubation with sedatives alone is an alternative. Fiberoptic and videolaryngoscopic intubations are difficult in maxillofacial trauma patients secondary to poor visualization resulting from blood, secretions, and vomitus in the airway. LMA should only be considered as a bridging device when immediate ventilation is needed and only used until a definitive airway can be established. Surgical airways and direct laryngoscopy are still the best options for definitive airway management. Nasogastric (NG) or orogastric tube placement if facial trauma is present, should be performed after intubation for gastric decompression.
Hoarseness, dysphonia, edema, persistent pain below the hyoid bone or crepitance over the thyroid cartilage implies a laryngeal injury. Presence of these signs necessitates a definitive airway. Endotracheal intubation is not contraindicated but may be difficult in this situation secondary to disruption and displacement of normal anatomic structures. If direct laryngoscopy is impossible, a cricothyroidotomy with prompt revision to a tracheostomy is the preferred alternative.
Tension pneumothorax or persistent air leak from chest tube may indicate a tracheal or bronchial injury. A chest X-ray may demonstrate signs of an occult upper airway injury by demonstration of mediastinal air. Bronchoscopy may be necessary for definitive diagnosis. Endotracheal intubation is not contraindicated in injury to the trachea below the cricothyroid membrane and should be attempted. Preparations for a surgical airway should be ongoing simultaneously. Tracheotomy below the trauma is the preferred alternative and should be performed immediately after the initial attempt at endotracheal intubation fails. Endotracheal or tracheostomy tubes may also be placed during diagnostic bronchoscopy if necessary.
Dashboard trauma to the neck in motor vehicle accidents and “clothes-line” injuries from motorcycle or skiing injuries can sever the soft tissue of the neck and the tracheal cartilage leaving a defect sufficient for intubation. Often this site is the laryngotracheal junction adjacent to the cricoid cartilage. Intubation of this defect is the preferred method of securing an airway in these patients, as endotracheal intubation will often result in the tube exiting the neck through the defect. A small-lumen (6.0 or smaller) ET tube can be inserted directly into the wound. If impossible, convert to tracheotomy.
See Chapter 24.
After securing an airway, monitor gas exchange with periodic arterial blood gases. Patients with concomitant lung injury may require higher Fio2 and positive endexpiratory pressure (PEEP) to maintain oxygenation. Cervical cord transection resulting in paralysis of the diaphragm or intercostal muscles precludes a strong cough making it difficult to tolerate secretions. Aggressive suctioning may be necessary.
Neck trauma with vascular injury may present with moderate to large hematomas, a pulsatile stable hematoma, pulse deficits, or a bruit. Look for any mediastinal changes on chest X-ray. Expanding hematomas can cause rapid airway compromise and necessitate intubation. Never remove impaled foreign bodies, as they may be preventing massive hemorrhage.
Direct firm pressure is the mainstay of stopping bleeding on the face and neck. Circumferential neck dressings are contraindicated as they may act as a noose if edema or hematomas worsen and will inevitably increase intracranial pressure (ICP).
If direct pressure alone fails, clamping with hemostats or suturing with a “figure of eight” stitch can control arterial bleeds. Direct visualization of the artery must be achieved before this is attempted to avoid vagus or phrenic nerve injury. Never blindly clamp large amounts of tissue.
If bleeding cannot be controlled with direct pressure then consider balloon tamponade. A foley catheter is inserted into the wound in the direction of active bleeding. Inflate the balloon with saline until bleeding stops or resistance develops. Gently pull back on the foley providing traction and compression. The need for FCBT does not imply a definitive vascular injury. If no vascular injury is detected in angiography then balloon catheter can be removed after 48–72 hours in the operating room.
Hypotension (SBP < 90 mm Hg) and shock (cool, pale skin, abnormal mentation) may be due to blood loss (hypovolemic shock) or poor sympathetic tone below a spinal cord lesion (neurogenic/spinal shock). The etiology of shock in the vast majority of trauma patients is hypovolemia.
See Chapter 11 for a more detailed discussion of shock. If hypovolemic shock is present, place two large-bore (16-gauge) intravenous catheters. If this fails, immediately place a triple-lumen central line with the largest internal diameter available. Obtain blood for a complete blood count, coagulation profile, electrolytes, renal function tests, and a type and crossmatch. Immediately infuse 2 L of isotonic crystalloid. If the systolic blood pressure remains below 90 mm Hg, infuse two units of un-crossmatched packed red blood cells (crossmatched if available). Continue administering blood products and crystalloid to improve hemodynamic stability while simultaneously arranging transfer of care to a trauma center.
Hypotension and bradycardia are hallmark signs of neurogenic shock due to spinal cord injury. Sympathetic interruption results in unopposed vagal tone. This must be differentiated from “spinal” shock which is a temporary loss of spinal reflex activity below the level of cord injury. Keeping the patient supine is often adequate to maintain adequate blood pressure, as little sympathetic tone is required. However, in the patient with persistent hypotension, infuse crystalloids to maintain a mean arterial pressure above 70 torr. Vasopressors should be used when hypotension inadequately responds to volume resuscitation. Phenylephrine is the therapy of choice. Atropine can be used for severe bradycardia.
Patients with blunt head trauma or multiple injuries from blunt or penetrating trauma should be assumed to have vertebral column injuries until proven otherwise. Complete immobilization in a cervical collar and on a spine board should be maintained until radiographically and/or clinically cleared. If neurological deficits are present, although controversial, some clinicians will consider starting methylprednisolone within 8 hours of injury. A 30 mg/kg bolus followed by 5.4 mg/kg/h infusion over next 23 hours.
Further Diagnosis and Evaluation
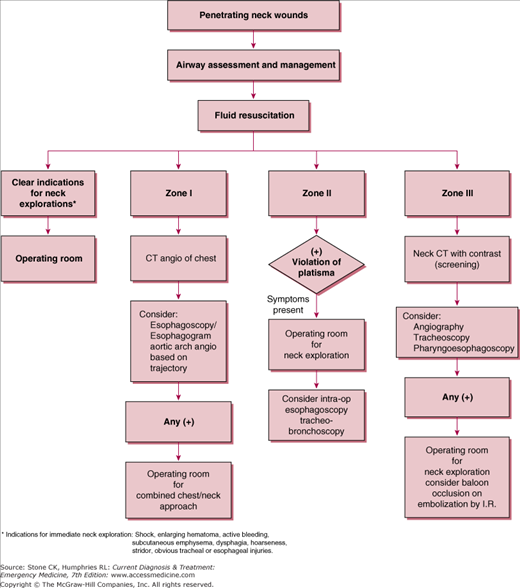
Penetrating neck trauma management will vary depending on the anatomical zone. Please see Figure 23–1.
Stab wounds to the neck can injure a variety of vital structures and require extensive diagnostic tests and/or surgical exploration depending on the location of the injury and associated symptoms. Leave any impaled objects in place as they may be providing local tamponade. If not present, determine the character of the weapon, its length, and the direction of entry to help assess the depth and extent of injury. Avoid nasogastric or orogastric tube placement as this may rupture contained pharyngeal hematomas.
High velocity missiles follow direct trajectory pathways. These bullet wounds can generate blast effect and secondary injury from bullet and bone fragmentation. Low velocity missiles are unpredictable and the path of trajectory does not appear to coincide with entrance or exit wounds. All structures in the neck must be evaluated including the airway, esophagus, vessels, and nerves. Surgical exploration is often necessary as well, depending on location.
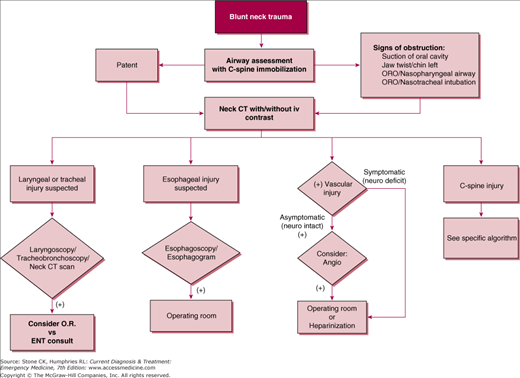
Blunt trauma is most often associated with tracheal, laryngeal, or C-spine trauma due to the ability of each to fracture. Softer structures such as vessels and the esophagus are rarely injured. If injury occurs, it may manifest as hematomas and hematemesis, due to shearing of vessels. Occasionally, blunt carotid or vertebral injury can result in symptoms typically associated with cerebrovascular accidents and have a high associated mortality. Pneumomediastinum can indicate esophageal or airway injury. See Figure 23–2.
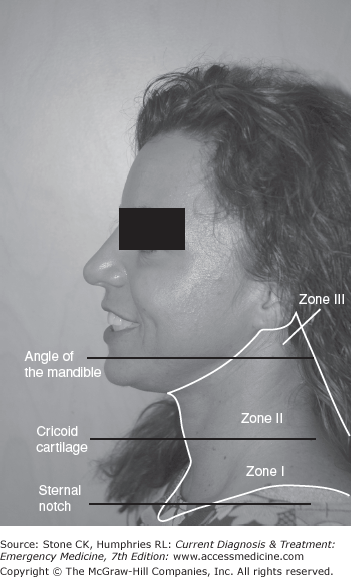
The location of a neck injury is critical to its treatment. Any injury penetrating the platysma should be described as in zone I, II, or III (Figure 23–3) and explored by a surgeon, not in the ED. The inferior border of zone I is the suprasternal notch and clavicles and the superior border is the inferior portion of the cricoid cartilage. Zone II extends from the inferior border of cricoid cartilage to the angle of the mandible. Classically, all zone II neck injuries penetrating the platysma warranted surgical exploration. With the combination of conventional angiography, CT angiography, CT scan, 2D Doppler, and esophagoscopy, exploration is now more selective. Zone III extends from the angle of the mandible to the base of the skull. Zone I and III injuries are not surgically explored. They present the problem of proximal and distal control of bleeding, respectively.
Injuries perforating the airway may manifest with air leak, subcutaneous pneumomediastinum or pneumothorax with persistent air leak despite chest tube placement. Other injuries including laryngeal fracture or tracheal contusion can present with stridor, hoarseness, painful phonation, hemoptysis, or hemothorax. Always monitor the patient’s airway. Bronchoscopy should be performed in any suspected airway injury. A high level of suspicion followed by bronchoscopy will identify the occult injury. Evaluate the C-spine with plain radiographs or CT scan when injury is suspected.
Esophageal injury manifests as hematemesis, dysphagia, odynophagia, soft tissue crepitus, saliva leak from wound, blood in nasogastric tube, prevertebral air on lateral C-spine, or pneumomediastinum on chest X-ray. Esophagogram with water-soluble contrast may reveal the injury but esophagoscopy is often necessary if symptoms persist despite a negative study.
While external bleeding is obvious, vascular injuries may be more insidious. An expanding hematoma may compress the trachea causing dyspnea. Palpate for a pulse deficit, bruit or thrill. Doppler ultrasound may be used as a screening test in low risk patients. Penetrating vascular injuries must be classified into zone I, II, or III. Zones I and III usually require angiography. The use of CT angiography is becoming more prevalent secondary to availability and being able to provide clinician with visualization of adjacent anatomic structures. However, conventional angiography remains the gold standard for identification of vascular injury. A trauma or cardiothoracic vascular surgeon should be involved immediately in suspected vascular injury as decompensation may occur rapidly.
Test all nerves in the neck at risk for injury.
Voice abnormalities, vocal cord asymmetry, hoarseness.
Sternocleidomastoid and trapezius weakness, inability to shrug shoulder of affected side and rotate chin against resistance to the opposite side.
Deviation of the protruded tongue to the side of the injury.
Use of respiratory accessory muscles, asymmetry of the diaphragm on chest X-ray.
All penetrating neck trauma deep to the platysma should have immediate surgical consultation and admission to the hospital. Blunt neck trauma with no symptoms of airway, esophageal, vascular, or nervous injury can be discharged safely. Always evaluate the C-spine and chest adequately in any neck injury.
Blunt trauma is the most common form of injury to the face followed by soft tissue lacerations and high velocity missile injuries. CNS involvement is common in missile injuries to the face and should take priority after the patient’s airway, breathing and circulation are assessed.
Mandibular fractures and traumatic facial injuries are often associated with difficult airways. If simple removal of debris and jaw-thrust maneuver fail, secure an airway with endotracheal intubation, cricothyroidotomy, or tracheostomy, in that order of preference. Avoid NG tubes if maxillary trauma exists.
Direct pressure is typically sufficient to stop any facial bleeding but pharyngeal packing may be necessary in some cases. Secure an airway before packing the mouth and pharynx. Avoid clamping facial arteries, as they are adjacent to important and difficult-to-visualize nerves.
Test all nerves of the face at risk for injury. Early diagnosis of nerve injury is crucial, as edema and pain may obscure examination as time passes.
Frontalis muscle: inability to wrinkle the forehead.
Orbicularis oculi: inability to shut eyes tightly.
All smiling muscles: inability to smile widely, wrinkle nose, or elevate the upper lip.
Lower lip depressors: inability to pucker or hold cheeks full of air.
Sensory deficit to any part of the entire face or upper neck.
Sensorineural hearing loss.
Sensory loss to the anterior 2/3 of the tongue.
Deviation of the protruded tongue to the injured side.
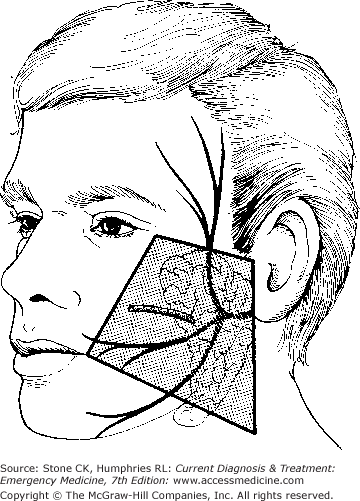
Evaluation of the parotid gland is essential if there is any chance of injury. Laceration of Stensen’s duct results in a difficult-to-repair salivary fistula if left untreated. Probe the duct with a lacrimal probe entering through the buccal opening. If the probe exits through the laceration, surgical repair is necessary. See Figure 23–4 as it demonstrates the area of high probability for Stensen’s duct as well as facial nerve injury. Consultation with a maxillofacial surgeon for any suspected parotid injury is recommended.
The presence of malocclusion suggests a mandible fracture. Inspect and palpate the hard palate, in order to identify any bony irregularity or instability which may be present in maxillary fractures. Check for crepitus upon moving the teeth and for loose or missing teeth, which can be an airway hazard if aspirated. Closely inspect the soft tissues including the lips, tongue, gingiva, buccal mucosa, floor of the mouth, and posterior pharynx for injury.
An irregular pupil or hyphema on gross examination may indicate a ruptured globe. Fundoscopic exam will reveal a difficult-to-visualize optic nerve and posterior pole. Slit lamp exam may demonstrate a shallow anterior chamber. If a ruptured globe is suspected, apply a rigid shield, administer prophylactic antibiotics, and consult an ophthalmologist. Diplopia, enophthalmos, or subcutaneous emphysema may indicate an orbital blowout fracture. Bilateral periorbital ecchymoses (“raccoon eyes”) are a sign of a basilar skull or ethmoid fracture. Diagnose all of these fractures definitively with a facial CT scan. Evert the lids, removing any foreign bodies, and stain the eye with fluorescein to reveal corneal abrasions. All ocular trauma patients should receive a slit lamp exam if possible.
Look into the nares and remove any blood clots or debris that may obscure a clear view. Assess for possible septal hematoma as this requires emergent drainage if present. Palpate the nasal bone for crepitus. Epistaxis is common with nasal injuries and may obscure full examination. Control any active epistaxis with nasal packing. Watch for aspiration of blood from the posterior nasopharynx if the bleeding is significant. Search for CSF rhinorrhea, which would necessitate a CT of the brain and neurosurgical consultation. There is no reliable way to distinguish CSF from thin nasal mucous in the ED.

Full access? Get Clinical Tree