Chapter 68 Maxillofacial and upper-airway injuries
MAXILLOFACIAL INJURIES
Life-threatening haemorrhage and airway obstruction are common complications accompanying severe blunt or penetrating maxillofacial and neck injury. Injuries may be isolated or part of multisystem trauma. Up to 20% of people with facial injury will have life-threatening associated injuries: 15% with closed head injury, 3.5% with airway obstruction and 1.5% with pulmonary contusion and/or aspiration.1–3 Urgent skilled airway management and awareness of other commonly associated injuries to the brain, cervical spine, thorax and oesophagus are paramount in preventing adverse outcomes. This chapter outlines the basic anatomy, pathology, complications and common pitfalls in the emergency management of maxillofacial, upper-airway and non-bony neck trauma.
EPIDEMIOLOGY
Maxillofacial trauma occurs most frequently in the 20–25 years age group, decreasing in frequency either side of this age group. It is three to five times more likely to occur in males than in females. Blunt injury is by far the commonest mechanism, accounting for nearly 97% of all maxillofacial injuries.4 Motor vehicle accidents (MVAs) account for nearly three-quarters of blunt injuries, with falls, physical assault, contact sports and industrial accidents accounting for the remainder. Legislative changes and preventative measures involving drink-driving, seatbelt and airbag use have seen a reduction in the incidence of MVA-related maxillofacial injury.5,6 In multiple trauma patients with an injury severity score (ISS) > 12, maxillofacial injury occurs in up to 17%, with a corresponding mortality rate of 13%.4
ANATOMICAL ASPECTS
Fractures, haemorrhage, soft-tissue damage and oedema are the commonest manifestations of blunt facial trauma. The severity of facial injury is directly related to the velocity of force applied.7 Common fractures of facial bones are maxilla (23%), orbital region (22%), zygoma (16%), nasal bones (15%), mandible (13%), teeth (8%), alveolar ridge (2%) and temporomandibular joint (TMJ) 1%.4
MANDIBULAR FRACTURES
The mandible is a unique, horseshoe-shaped bone that is tubular and weakest where the cortices are thinnest; most fractures occur at vulnerable points, regardless of the point of impact.8 Common sites are the ramus (condylar neck and angle of the mandible) and body at the level of the first or second molar. Multiple fractures are common (64%),8 with body of mandible fractures often being accompanied by fractures of the opposite angle or neck, due to transmitted forces. Mandibular fragments are often distracted due to the action of the lower jaw muscles. Respiratory obstruction may occur after bilateral mandibular angle or body fractures due to the posterior displacement of the tongue – the ‘Andy Gump’ fracture.9,10
MIDFACIAL FRACTURES
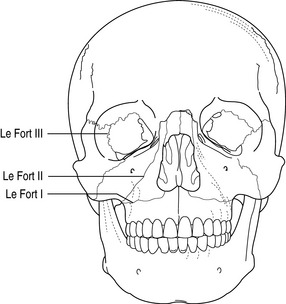
The bones of the middle third of the face are relatively thin and poorly reinforced. Fracture dislocations occur through the bones and suture lines and the facial skeleton acts as a compressible energy-absorbing mass that gives on impact. The series of compartments (nasal cavity, paranasal sinuses and orbits) within the bony framework collapse progressively, absorbing energy and protecting the brain, spinal cord and other vital structures.11 Multiple complex facial fractures usually result and isolated facial bone fractures are rare. Le Fort described three great lines of weakness in the facial skeleton and thus derived the Le Fort classification of fractures12 (Figure 68.1). Le Fort fractures are perpendicular to the three main vertical buttresses of the facial skeleton – the nasomaxillary, zygomaticomaxillary and pterygomaxillary ‘pillars’. Le Fort fractures rarely occur in their pure form with mixed patterns prevailing (e.g. right hemifacial Le Fort I and left hemifacial Le Fort II). Airway obstruction from posterior movement of the soft palate against the tongue and the posterior pharyngeal wall may occur. Oral secretions, blood, bone and tooth debris and pharyngeal wall haematomas may worsen airway compromise.
LE FORT I (ALSO KNOWN AS GUERIN’S FRACTURE)
This fracture involves only the maxilla at the level of the nasal fossa. It follows a horizontal plane at the level of the nose. The fracture separates the palate from theremainder of the facial skeleton (i.e. palate–facial disjunction) and is usually caused by direct low-maxillary blows or by a lateral blow to the maxilla.
LE FORT II
This is the most common midface fracture.13 The maxilla, nasal bones and medial aspect of the orbit are involved which results in a freely mobile, pyramidal-shaped portion of the maxilla (i.e. pyramidal disjunction). The fracture line extends from the lower nasal bridge through the medial wall of the orbit, and crosses the zygomaticomaxillary process. It is caused by direct blows to the mid-alveolar area, or by lateral impacts and inferior blows to the mandible when the mouth is closed.
LE FORT III
This is known as craniofacial disjunction because the fracture line runs parallel to the base of the skull, separating the midfacial skeleton from the cranium. The fracture extends through the upper nasal bridge and most of the orbit and across the zygomatic arch. It involves the ethmoid bone, and thus may transect the cribriform plate at the base of the skull.13,14 These fractures result from superiorly directed blows to the nasal bones.13
TEMPOROMANDIBULAR JOINT
Mechanical TMJ impairment may result from condylar or zygomatic arch fractures and can prevent jaw opening even after muscle relaxants have been administered.15
ZYGOMATIC, ORBITAL AND NASAL FRACTURES
Zygomatic fractures are uncommon, but its attachments to the maxilla, frontal and temporal bones are vulnerable and may be disrupted. When the zygoma is displaced, disruption of the lateral wall and floor of the orbit may ensue. Orbital injury is commonly associated with midface trauma. The severity of injury in the orbital region varies from oedema and ecchymosis of the periosteal soft tissue to subconjunctival haemorrhage and loss of visual acuity or ocular rupture. Blinding injuries reported with facial fractures occur in 3–12% and most are secondary to globe perforation rather than optic nerve injury.16 Orbital blowout fractures occur when pressure is directly applied to the eye, and is hydraulically transmitted via the globe to the interior bony structures. The weaker inferior wall usually fractures, causing enophthalmos, diplopia, impaired eye movement and infraorbital hypoaesthesia. Nasal fractures are common, with epistaxis and septal haematoma being the prime concerns.
HAEMORRHAGE
Haemorrhage following blunt maxillofacial injury is extremely common. Life-threatening bleeding is fortunately rare. Various series have reported the incidence to be between 1 and 10%.1,17–19 Most severe haemorrhage is associated with midfacial fractures although soft-tissue lacerations alone can cause significant blood loss. Swallowing of large quantities of blood may conceal haemorrhage and predispose to aspiration.20
The origin of bleeding in facial trauma is complicated, as the vascular supply is derived from both the internal and external carotid arteries, with anastomoses occurring between them as well as between both halves of the face. The internal maxillary artery, especially the intraosseous branches, is the main source of bleeding in facial injury, because the artery passes within the common Le Fort fracture borders.16 The comminuted nature of maxillary fractures makes the detection of an exact site of vessel damage nearly impossible.16 Branches of the internal carotid artery such as the lacrimal and zygomatic branches, as well as the anterior and posterior ethmoidal arteries, may contribute to bleeding.
ASSOCIATED INJURIES
Basilar skull fracture
The anterior cranial fossa is often involved in craniofacial injuries. Fractures involving the frontal bone, frontal sinus, nasoethmoid complex or fronto-orbital complex result in bone defects in the skull base and can cause dural tears with resultant leakage of cerebrospinal fluid (CSF). CSF fistulae occur in 10–30% of basilar skull fractures.21 The clinical finding of CSF rhinorrhoea is not diagnosticfor anterior cranial fossa lesions, as this represents only the site of exiting CSF. The origin may be from a temporal bone fracture, because CSF from the middle ear discharges into the nose via the Eustachian tube. A middle cranial fossa defect can produce rhinorrhoea through the sphenoid sinus. The vast majority of fistulae present within 1 week of injury. Meningitis in patients with midface fractures is uncommon, despite the fact that approximately 36% of patients sustaining Le Fort fractures with anterior cranial fossa fractures have CSF leaks.22,23
Head and cervical spine injury
The incidence of head injury in those with maxillofacial trauma has been variably reported to be between 15% for severe head injury, increasing to 80% if all grades of head injuries are included.1,4,24 Cervical spine injury has been reported in up to 11% of patients.
The association between maxillofacial and cervical spine injury depends on the mechanism of injury. Falls and motor vehicle accident victims are more likely to have cervical injury than sporting or personal assault victims.25 Cervical spine fracture occurs with mandibular injury in 3%16 and is attributed to forces exerted directly or indirectly from the facial skeleton to the neck. C1/C2 and C5–C7 are at particular risk.
Other injuries
Thoracic (9–40%) and abdominal (5–40%) trauma and limb fractures (30%) are other common coexistent injuries.24,26 Traumatic occlusion of the internal carotid artery (ICA) is a rare complication of maxillofacial trauma occurring in less than 0.5% of patients presenting with blunt maxillofacial injury.27,28 It is usually recognised when a patient develops an unexplained neurological deficit, most often hemiplegia, subsequent to trauma or surgery of the head, face or neck. Assessment of the carotid circulation by CT angiography is a useful investigation if carotid injury is suspected.

Full access? Get Clinical Tree