1. Cardiac disease is the leading cause of maternal death in both the United States and the United Kingdom.2,5
a. The combination of cardiovascular disease and cardiomyopathy caused 26% of maternal deaths in the United States between 2006 and 2010.2
b. A large number of deaths from peripartum cardiomyopathy transpire more than 42 days after the end of pregnancy.
c. Chronic hypertension is the most important factor associated with increasing population prevalence of cardiomyopathy in the United States.6
2. Infection led to 13.6% of maternal deaths in the United States between 2006 and 2010.2
a. Influenza was the leading cause of death due to infection in both the United States and the United Kingdom3; prevention strategies include universal influenza vaccination and rapid testing and antiviral therapy for pregnant women exhibiting flu-like symptoms.
b. Genital tract infection caused by group A Streptococcus can lead to septic shock within 2 hours of initial presentation.3,7
3. Noncardiovascular medical conditions contribute to another 12.8% of maternal deaths in the United States.
a. Altogether, indirect causes lead to more than half of maternal deaths in the United Kingdom3 and close to half in the United States.2
b. Poorly controlled preexisting medical and psychiatric conditions are among the most important risk factors for maternal mortality.8
4. Hemorrhage (11.4%) was the leading cause of maternal death in the United States between 1987 and 1990 and continues to be a common cause of maternal morbidity and mortality during the hospitalization for delivery.9
a. The majority of deaths due to hemorrhage are judged to be preventable in multiple confidential mortality reviews.3,10
b. The most common preventable factors involve delays in diagnosis and treatment.9,11
5. Hypertensive disorders of pregnancy (9.4%) may precipitate lethal intracranial hemorrhage; less common mechanisms of death include pulmonary edema and hepatic rupture.
a. In one large health system review, the most common preventable causes of death from hypertensive disorders were failure to adequately control blood pressure and failure to diagnose and treat pulmonary edema.9
b. Protocols for rapid antihypertensive therapy for defined blood pressure thresholds can reduce preeclampsia-related deaths.12
6. Venous thromboembolism (9.3%) includes both cerebral venous thrombosis and pulmonary embolism.
a. Universal thromboembolism prophylaxis with intraoperative sequential compression devices during cesarean delivery (CD) and targeted postpartum pharmacologic anticoagulation is the most important strategy to reduce maternal mortality from venous thromboembolism.12
b. Cerebral venous thrombosis and other serious intracranial pathology should be considered in the differential diagnosis for postpartum headache.3
7. Amniotic fluid embolism (5.3%) is often considered not preventable. Aggressive supportive therapy improves the likelihood of survival.
8. Injury-related deaths are relatively common, but are considered pregnancy-associated and are not included in the statistics for pregnancy-related death.
CLINICAL PEARL Indirect causes are the main reasons for maternal death in the developed world; cardiac disease is the leading cause of maternal death in the United States and United Kingdom.
D. Risk factors
The most potent risk factors for maternal mortality and severe morbidity are clinically significant medical conditions that predate the pregnancy.3,8,13,14
1. Three-quarters of women who died in the United Kingdom between 2009 and 2012 had a preexisting medical condition.3
2. Preconception counseling and intensive multidisciplinary antepartum and intrapartum care may improve outcomes for women with serious medical or mental health conditions that may be aggravated by pregnancy.3,15
3. Insufficient prenatal care may result in suboptimal management of existing medical conditions or delay the diagnosis of pregnancy complications.2,8
4. Advanced maternal age increases maternal risk,16 with a linear trend evident for each 5-year increase in maternal age beyond 34 years.15
5. Racial and ethnic minority groups experience increased risk.8,15
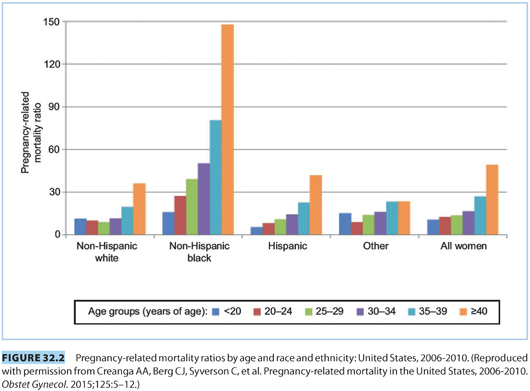
a. In the United States, non-Hispanic black race confers a threefold increase in the risk of maternal death compared with non-Hispanic white women.2,17 The disparity is exacerbated by increasing maternal age. Non-Hispanic black women older than 25 years have a fourfold increased risk of death, as illustrated in Figure 32.2.2
b. Immigrants and nonnative speakers experience high rates of both maternal death and substandard care.15,18,19
6. Obesity (body mass index [BMI] ≥30 kg per m2) increases risk of death when severe pregnancy complications develop.18 Conversely, very low body weight (<60 kg) may increase risk of hemorrhage-related mortality due to extremely small circulating blood volume.3,8
7. Multifetal pregnancies increase risk of serious complications of pregnancy and maternal death.15,20
8. Cesarean delivery is associated with maternal death.21,22
a. Most maternal deaths following CD are caused by the underlying medical or obstetric disease that indicated the CD; rarely, cesarean surgery causes fatal infection, hemorrhage, or venous thromboembolism.9
b. Cesarean deliveries increase the risk of placenta accreta in subsequent pregnancies and thus contribute to the overall population level risk of maternal death.23
II. Severe maternal morbidity
A. Definitions
1. Severe morbidity refers to serious complications in pregnancy with the potential to cause end-organ injury or maternal death. A practical definition of severe morbidity is either intensive care unit (ICU) admission or the administration of ≥4 units of erythrocytes or whole blood, or both.3
2. Near-miss morbidity includes life-threatening complications that result in severe end-organ dysfunction or failure.14,24
B. Epidemiology
1. Severe morbidity complicates 1.6% of pregnancies in the United States, corresponding to more than 60,000 pregnancies per year.25
2. Near-miss morbidity develops in approximately 0.13% to 0.2% of US hospitalizations for delivery.14,26
CLINICAL PEARL For each maternal death, approximately 50 to 100 women experience a severe morbidity.

Full access? Get Clinical Tree








