Low Cerebrospinal Fluid Pressure
Steinar T. Vilming
Bahram Mokri
POSTLUMBAR PUNCTURE HEADACHE
Definition of Post-Lumbar Puncture Headache
International Headache Society (IHS) code and diagnosis: 7.2.1 Postdural (postlumbar) puncture headache
World Health Organization (WHO) code and diagnosis: G44.88 Headache associated with other specified disorders
Short description: Bilateral headache that develops within 5 days after lumbar puncture (LP) and disappears within 1 week. Headache occurs or worsens in the upright position and disappears or improves after resuming the recumbent position.
Other terms: postlumbar puncture headache, postdural puncture headache, postmyelogram headache
Essex Wynter in 1889 and H. Quincke in 1891 performed the first dural punctures, and a vast amount of literature followed on the distressing headache that may ensue. Postlumbar puncture headache (PPH) and other headaches due to low cerebrospinal fluid (CSF) pressure are unique because of the postural character, occurring or worsening when assuming the erect position.
Pathophysiology
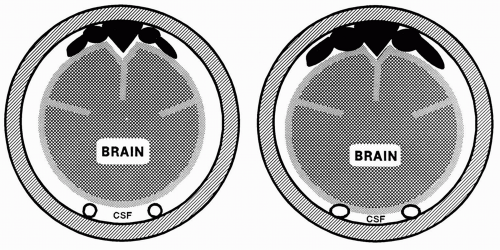
The exact cause of PPH remains elusive. The favored “leakage theory,” which was proposed at the beginning of this century, implies that post-LP leakage of CSF through a dural rent leads to a decreased CSF pressure and volume, whereby the cerebral veins dilate and the brain is deprived of its CSF cushion (72). The consequent gravity-dependent downward sagging of the brain causes traction on the distended and distorted pain-sensitive anchoring veins (the sagittal sinus and its tributary veins) and pressure on equally pain-sensitive large arteries at the skull base and the tentorium (Fig. 114-1). Several facts support this theory.
A dural rent is caused by a Quincke-cut needle and it has the form of a nearly opened tin lid hinged on one side (Fig. 114-2). Complete sealing of a rent may take more than 14 days (22). Small rents caused by thin needles heal more rapidly than larger rents, and rents made through the thickest parts of the dura retract more quickly than rents in the thinner parts (22,32). Penetrating the dura with the bevel of a Quincke needle parallel rather than transverse to the longitudinal axis of the dural cylinder reduces the incidence of PPH, possibly because such a technique creates the smaller apertures (29). It has been suggested, although unproven, that a rent created by an oblique needle insertion or a penetration through a richly vascularized area of the dura might be more likely to heal (32,57).
CSF is normally produced at a rate of about 0.3 mL per minute, but despite its great renewal capacity, a low CSF volume and pressure may be maintained by CSF leakage, which could be continuously observed by direct inspection isotope studies weeks and even months after a spinal tap. Epidurally lost CSF is absorbed through the intervertebral foramina (32).
CSF pressure closely parallels the venous pressure at all levels of the intracraniospinal system. In the erect human, intracranial CSF pressure is negative at the vertex, approximately 150 mm H2O. In the horizontal position, intracranial CSF pressure is positive at all levels, normally 50 to 180 mm H2O. Removal of 30 mL CSF regularly induces headache in the erect position concomitant with a reduction of the vertex CSF pressure down to approximately 220 to 290 mm H2O. The headache is ameliorated by restoration of the CSF volume or tilting toward the horizontal position and augmented by jugular compression (44,93). In some PPH patients, CSF pressure is zero or low when repunctured (57,82), and intrathecal infusion of saline relieves the headache by restoring the pressure (60). In a controlled clinical study, the average reduction in CSF pressure after lumbar puncture (LP) was significantly greater for patients with headache compared with patients without headache (95). In another study, however,
only three of five PPH patients had a low CSF pressure with repuncture after 24 hours, and a low CSF pressure was found in 7 of 37 patients who had not developed PPH (47). Thus, the association between PPH and low CSF pressure is not invariable, and other factors may play some role.
only three of five PPH patients had a low CSF pressure with repuncture after 24 hours, and a low CSF pressure was found in 7 of 37 patients who had not developed PPH (47). Thus, the association between PPH and low CSF pressure is not invariable, and other factors may play some role.
CSF serves to buoy about 97% of the weight of the slightly denser brain (61). By magnetic resonance imaging (MRI), it has been shown that the CSF volume is significantly reduced in nearly all patients 24 hours after LP and that there is a trend toward a greater reduction in those who develop PPH than in controls (36). This loss of CSF causes the thin-walled veins to distend, which has been observed directly through a cranial window in cats (31). Also, the brain appeared edematous and cyanotic, and the arteries were constricted slightly. These findings agree with the Monro-Kellie doctrine with Burrow’s modification, which postulates that blood volume increases when the CSF volume is reduced and vice versa (37). Elevated blood volume is due exclusively to a venous dilation, since the venoarterial reflex, which occurs within seconds of CSF removal, causes the arteries to constrict and keeps cerebral blood volume unaltered.
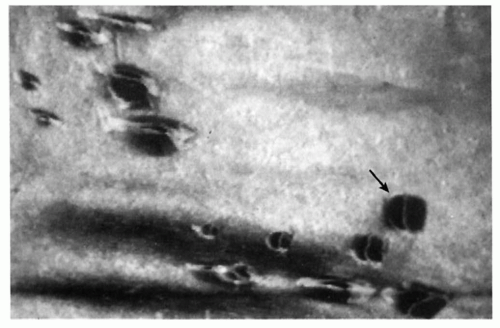 FIGURE 114-2. Effect of dural puncture with Quincke needles of different sizes from 20 to 29 gauge. The typical “tin-lid effect” is visualized, and one example is given (arrow). From Dittmann et al. (23). |
Clinical Features
IHS diagnostic criteria for postdural (postlumbar) puncture headache (revised International Headache Classification of Headache Disorders [ICHD-II]) are as follows:
A. Headache that worsens within 15 minutes after sitting or standing and improves within 15 minutes after lying, with at least one of the following and fulfilling criteria C and D:
1. Neck stiffness
2. Tinnitus
3. Hypacusia
4. Photophobia
5. Nausea
B. Dural puncture has been performed.
C. Headache develops within 5 days after dural puncture.
D. Headache resolves either:
1. Spontaneously within 1 week
2. Within 48 hours after effective treatment of the spinal fluid leak (usually by epidural blood patch)
PPH occurs within 2 days (range: minutes to days) after LP in approximately 90% of patients (83). It usually lasts a week, but a duration of several weeks or even months has been reported (44,60,79,82,83), probably because of a persisting fistula. PPH with early onset seems to last longer and tends to be more severe than PPH with a later onset (35,88). PPH is posture dependent, usually starting to increase within 20 seconds when the patient assumes an
upright position, reaching its maximum within another 30 seconds, and subsiding within 20 seconds of assuming recumbency (Fig. 114-3) (83). The time course of PPH is fairly stable until the last 2 days of its course, when the headache severity usually starts to subside, the patient’s mobility increases, and the time required for headache to develop on rising increases (84).
upright position, reaching its maximum within another 30 seconds, and subsiding within 20 seconds of assuming recumbency (Fig. 114-3) (83). The time course of PPH is fairly stable until the last 2 days of its course, when the headache severity usually starts to subside, the patient’s mobility increases, and the time required for headache to develop on rising increases (84).
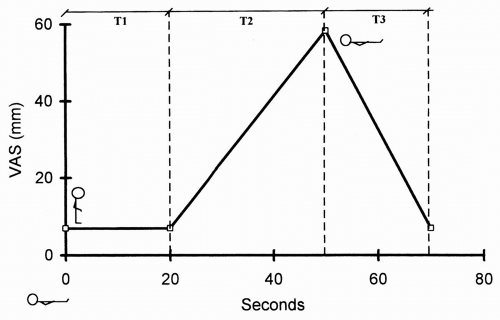 FIGURE 114-3. Headache severity on a 100-mm visual analogue scale (VAS) related to time; median values from 79 patients. The body position of the patient is indicated. The pain is minimal when the patient is in the recumbent position, but pain starts to increase after 20 seconds when the patient is in the upright position (T1). The time to maximal pain is 30 seconds (T2). When the patient lies down, the pain decreases to its lowest level within 20 seconds (T3). From Vilming and Kloster (83). |
PPH is usually described as aching, dull, deep, constricting, or throbbing, and it is most frequently frontal but often occipital, fronto-occipital, or generalized (1,44,79,82). More than half of PPH patients have associated symptoms, and the more severe the PPH, the more frequently the symptoms occur. Dizziness and nausea, occasionally with vomiting, are most prevalent. Auditory difficulties and tinnitus are not infrequent and may be caused by leakage of perilymphatic fluid from the cochlea to the cerebrospinal space through a cochlear aqueduct, which is functionally open in about 50% of adults (48,90), resulting in a Ménière-like syndrome. Blurred vision and other visual disturbances are quite infrequent. Cranial nerve lesions, usually the abducens nerve, have been reported (1,79,82,88).
Age and gender influence the incidence of PPH. Data from old studies that investigated large numbers of patients (79,82) and a more recent report (88) indicate that the incidence of PPH is highest among younger patients, perhaps with the exception of prepubertal children (26). Also, the incidence of PPH may decrease with increasing age, usually above 50 or 60 years, perhaps on the basis of narrowed epidural space (81) or reduced elasticity of pain-sensitive cerebral vessels (82). It should be noted, however, that concerns with study methodology and the potential confounding effect of gender cast doubt on the conclusion that the incidence of PPH is reduced with increasing age (79).
The potential effect of gender on the incidence of PPH has been addressed in several studies, but most were not designed specifically for that purpose, and hence the potential for methodologic flaws. In general, the incidence of PPH is higher in women than in men (19,25,79,80, 82,88,95). It is suggested that this observation is on the basis of a higher incidence of PPH in women of childbearing age and does not apply to the prepubertal girls or postmenopausal women (Fig. 114-4). Also, the authors of a large study (n = 300 patients) argued that the apparent reduction in the incidence of PPH with age is gender dependent; that is, the incidence of PPH is reduced in aging women only (88).
The indication for LP may impact the development of PPH. The incidence of PPH following spinal anesthesia (SA) is reportedly lower than that following diagnostic LP (79). Perhaps the requirement that patients post-SA remain on bedrest for several days after the procedure hides cases of short-lasting PPH. Also, it is unclear how the introduction of intrathecal chemicals during SA influences the development of PPH.
Several well-designed controlled studies have indicated that the incidence of PPH decreases with a smaller needle size, possibly because of reduced leakage through smaller rents (Table 114-1) (30,33,43,58,80). It is recommended that a 20-gauge needle or smaller be used for diagnostic
LP (14). Also, an oblique penetration of the dura (40), insertion of a Quincke needle with the bevel parallel instead of transverse to the longitudinal axis of the dural cylinder reduced the incidence of PPH in one study (29), but this was not proved in another (58). The use of atraumatic (blunttipped) needles reduce the incidence of PPH (75,78).
LP (14). Also, an oblique penetration of the dura (40), insertion of a Quincke needle with the bevel parallel instead of transverse to the longitudinal axis of the dural cylinder reduced the incidence of PPH in one study (29), but this was not proved in another (58). The use of atraumatic (blunttipped) needles reduce the incidence of PPH (75,78).
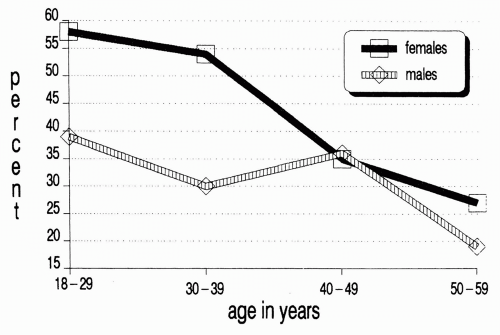 FIGURE 114-4. Incidence of postlumbar puncture headache (PPH) related to age for 150 men and 150 women. There was a significantly higher incidence of PPH in women (p < 0.025) and in patients younger than 40 years (p < 0.005). A significant difference between the two age groups is only shown for women (p <0.005), and the incidence of PPH is significantly different for the two sexes only below the age of 40 years (p <0.01). From Vilming et al. (88). |
TABLE 114-1 Well-Designed Controlled Studies Regarding the Significance of Needle Sizea | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Full access? Get Clinical Tree