Modality
Advantages
Disadvantages
Spinal anesthesia
• Better analgesia in the early postoperative period
• Prolonged analgesia with the addition of morphine (150–300 mcg; 4–10 mcg/kg)
• Attenuates neuroendocrine response and prevents DVT
• Cost effective
• Reliable and rapid onset
• Unable to control the rate of spread
• Limited duration
• Difficult to perform in uncooperative patients
• Spine abnormalities (kyphosis and scoliosis) and previous spine instrumentation may prevent placement
• Contraindications: patient refusal; clotting abnormalities; hypovolemia and systemic infections
• Potential adverse events: severe hypotension, neuraxial hematoma, abscess formation, total spinal anesthesia, postdural puncture headache, nerve dysfunction, and damage.
• Neuraxial opioids can cause respiratory depression, nausea, pruritus, and urinary retention.
Epidural analgesia
• Benefits similar to spinal anesthesia
• May slowly dose epidurals
• Prolonged the duration of analgesia
• Similar disadvantages as spinal anesthesia
• Early ambulation may be delayed
• Additional costs to perform and maintain epidural
• Risk of muscle weakness and falls
Peripheral nerve block
• Limited cardiovascular or pulmonary side effects
• Proximal blocks (lumbar plexus + sciatic nerve blocks) can surgical anesthesia or analgesia depending on the dosing
• Superficial blocks (femoral nerve blocks and adductor canal blocks)
• Potential for local anesthetic systemic toxicity
• Requires technical skill and additional costs to perform and maintain continuous PNB
• Proximal blocks (lumbar plexus) carry the same risks of a neuraxial block (hematoma, spinal, or epidural drug spread)
• Risk of falls (minimized with adductor canal blocks)
Local infiltration analgesia
• Easy to administer
• Cost effective
• Analgesia equivalent to neuraxial techniques and peripheral nerve blocks
• No motor weakness as a result of the technique
• Cannot be performed in intact joint
• Risk of infection if sterile precautions are not ensured
• Single injection blocks have limited duration of action
Wound infiltration with local anesthetics has been practiced for several decades due to its simplicity, ease of administration, and effectiveness [25]. Since a single injection has a limited analgesic duration, a multitude of techniques have been used in the last decade to prolong analgesia which includes local infiltration analgesia (LIA), continuous or intermittent injections through the wound catheters and liposomal local anesthetic formulations. Local infiltration analgesia (LIA) also known as High Volume Local Infiltration Analgesia (HV-LIA) is a form of wound infiltration which commonly refers to the administration into the surgical field of large volumes of local anesthetics with or without added adjuvants perioperatively.
In this chapter, we will first present the techniques and the evidence regarding local infiltration analgesia for total knee replacement from an orthopedic surgeon’s perspective, and then we will discuss and summarize the efficacy and implications of LIA, for total knee replacement other orthopedic procedures.
Historical Perspective
In the ensuing years following the discovery of local anesthetic properties by Carl Koller in 1884, [26] cocaine was primarily utilized for topical anesthesia and regional nerve blockade [27]. Carl Ludwig Schleich is credited with introducing and standardizing the technique of “infiltration anesthesia ” in 1892 [28, 29]. His technique involved infiltrating the different layers of the surgical wound with a series of overlapping injections as the surgery proceeded. The earliest cases of infiltration analgesia also revealed the first cases of complications associated with the technique. Schleich noted local anesthetic toxicity after using higher concentration of cocaine (2 and 5 %) and hence recommended the use of dilute solutions (0.001, 0.1, and 0.2 %) and larger volumes (to a total dose of 50 mg). He also noted improved analgesia when cocaine was combined with morphine. Although frowned upon at the time, we have come to realize that all of these ideas apply to LIA even today. Infiltration techniques were found to be efficacious for a wide variety of surgeries subsequently and have been accepted as a part of practice [30–36]. The initial description of local anesthetic infiltration and infusion following lower limb arthroplasty was performed by Bianconi et al. in 2003 (see below). They infiltrated 40 ml of 0.5 % ropivacaine for wound infiltration intraoperatively followed by an infusion of 0.2 % ropivacaine at 5 ml/hr. [37] Local infiltration analgesia was the term coined by Dr. Dennis Kerr and Dr. Lawrence Kohan for high volume local anesthetic infiltration, performed in a systematic way during total knee arthroplasty [16]. The infiltrate is usually a cocktail of a long-acting local anesthetic (ropivacaine), an NSAID (ketorolac ), and a vasoconstrictor (epinephrine ), with or without a corticosteroid.
Surgeon’s Perspective: Local Infiltration Anesthesia in Total Knee Arthroplasty
Total knee arthroplasty (TKA ) can be associated with substantial pain in the perioperative period. Pain that is inadequately controlled may impair mobility, reduce the ability to participate in rehabilitation, and reduce patient satisfaction. In addition, in some patients, inadequately controlled pain may result in the development of chronic pain. Traditional general anesthesia combined with patient-controlled opioid analgesia may be associated with undesirable side effects, including postoperative nausea and vomiting, hypotension, urinary retention, respiratory depression, delirium, and postoperative infections. For many surgeons, local infiltration anesthesia (LIA) in recent years has become a key element of the pain management paradigm for total knee arthroplasty patients.
Interest in local infiltration anesthesia among orthopaedic surgeons has increased since the first trials were published, demonstrating its efficacy as a technique. Subsequently, multiple trials comparing LIA to placebo, peripheral nerve blocks and central neuraxial blocks, were performed which has established the role of LIA in arthroplasty surgery. Busch et al. [38] completed one of the first randomized clinical trials evaluating the use of local infiltration analgesia. Sixty-four TKA patients were randomized to receive either; a periarticular intraoperative injection containing ropivacaine , ketorolac , epimorphine, and epinephrine or to receive no injection. Other aspects of perioperative pain management were standardized between the two groups. The patients who had received the injection used significantly less patient-controlled analgesia at 6 h, 12 h, and over the first 24 h following surgery. In addition, they had higher visual analog scores for patient satisfaction and lower visual analog scores for pain during activity, immediately following surgery and four hours after the operation. No cardiac or central nervous system toxicity was observed in patients who received the injection. Similarly, Vendittoli et al. [39] evaluated patients who received perioperative LIA combined with self-administered morphine, compared to a group of patients who received self-administered morphine alone. Both groups demonstrated high satisfaction rates and good pain control. However, morphine consumption was significantly lower in the local analgesia group than it was in the control group at 24 and 48 h following surgery. Jiang et al. [40] has completed a review of 21 randomized controlled trials evaluating LIA compared to placebo in total hip and total knee arthroplasty patients. Pooled results showed that the LIA group had better pain relief, less opioid consumption, a larger range of motion, and lower rates of nausea and vomiting, than the placebo group.
The contents and dosing of medications in local infiltration analgesia cocktails has varied significantly in the published literature. The mixture used by Busch et al. [38]1 contained 400 mg ropivacaine (80 mL of 0.5 % ropivacaine at 5 mg/mL), 30 mg ketorolac (1 mL at 30 mg/mL), 0.6 mg of 1:1000 epinephrine (0.6 mL at 1 mg/mL), and 5 mg morphine (0.5 mL at 10 mg/mL) diluted to a volume of 100 mL. Kelly et al. [41] reported on a mixture containing ropivacaine, epinephrine, and ketorolac combined with clonidine, an alpha-2 adrenergic receptor agonist intended to produce synergistic effects, with local anesthetics and opioids. Others have described infiltration cocktails with the addition including steroids (methylprednisolone) and antibiotics (cefuroxime) [42].
In order to understand the essential components of a local infiltration anesthetic cocktail, Kelley et al. [41] evaluated 150 patients who received one of four different periarticular injection mixtures when undergoing TKA . The patients were divided into four groups based on the mixture received. Group A received ropivacaine , epinephrine , ketorolac , and clonidine; Group B received ropivacaine, epinephrine, and ketorolac; Group C received ropivacaine, epinephrine, and clonidine and Group D was the control. They found that patients who had received periarticular injections containing ropivacaine, ketorolac, and epinephrine with or without clonidine had substantially less pain in the immediate postoperative period than did those patients who received injections containing ropivacaine and epinephrine alone. This suggested that ketorolac was a key component that should be considered for inclusion in all local infiltration cocktail mixtures.
The technique of administration of local infiltration analgesia in the operating room has also varied in the published literature. In the description by Busch et al. [38], the injection of the cocktail was divided into distinct phases. The first portion of the injection occurred just prior to component implantation. At that point in the procedure, 20 mL mixture of the 100 mL cocktail is injected into the posterior capsule and medial and lateral collateral ligaments (Fig. 24.1). This is completed prior to component implantation to give better access to the posterior aspect of the knee to allow for effective posterior capsular injection. Care is taken to avoid excessive infiltration in the posterolateral corner in the area of the common peroneal nerve. Once the components have been implanted and the cement is curing, 20 mL is injected into the quadriceps and retinacular tissues (Fig. 24.2). Finally, after component implantation is complete and prior to closure, the remaining 60 mL is infiltrated into the fat and subcutaneous tissues. Subsequent authors have included the addition of infiltration into the medial and lateral periosteum, meniscal remnants, PCL, pesanserinus, and illiotibial band [41, 42].

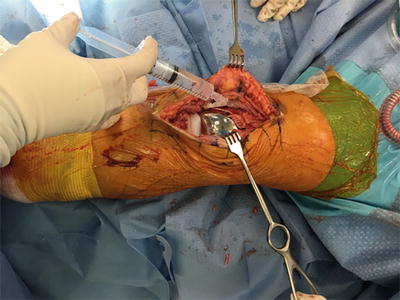

Fig. 24.1
Injection of local anesthesia infiltration into the posterior capsule of a total knee replacement. Injection is completed prior to placement of the definitive implants to allow easy access to the posterior aspect of the knee
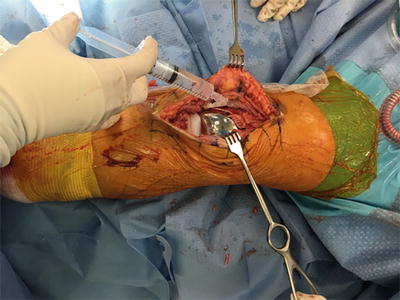
Fig. 24.2
Following definitive component placement infiltration of the quadriceps and retinacular tissues as well as the fat and subcutaneous tissues superficially
Local infiltration anesthesia has been prospectively compared to peripheral nerve blocks (PNB) in a number of studies. In one of the first such trials, parvataneni et al. [42] evaluated 60 patients in a prospective study comparing local infiltration anesthesia to femoral nerve block (FNB) combined with patient-controlled analgesia (PCA) . The LIA group had an improved ability to perform a straight leg raise on postoperative day 1 (63 % vs. 21 %). Similar pain scores were demonstrated between both groups during their postoperative hospital course. The results suggested that LIA provides pain control equivalent to that of FNB with the added advantage of maintaining quadriceps motor strength. Similarly, Spangehl et al. [43] compared patients receiving LIA to a group of patients who received a continuous femoral nerve block and single shot sciatic nerve block. Although pain scores were lower on the day of surgery in the PNB group, they were similar for the remainder of the hospital stay. The patients in the PNB group experienced more acute postoperative falls and lower quadriceps function measured by the ability to perform a straight leg raise on postoperative day 1 (24 % vs. 79 %). In addition, the patients receiving PNBs had more peripheral nerve dysesthesias at 6 weeks postoperatively.
Approved for use in the United States EXPAREL (Pacira Pharmaceuticals, Inc., San Diego, CA, USA) is a slow releasing bupivacaine medication designed to reduce the risk of bupivacaine toxicity and provide an extended duration of postoperative pain relief following surgery. Bramlett et al. [44] examined four varying doses of liposomal bupivacaine (133, 266, 300, and 532 mg) compared with a control of nonliposomal bupivacaine (150 mg). Treatment with liposomal bupivacaine was associated with greater analgesia while patients were at rest after surgery compared with bupivacaine although this was seen only in the cohort receiving a dose twice the recommended value (532 mg). Subsequent studies have failed to demonstrate significant benefits in morphine consumption, pain scores, knee range of motion, length of stay with the use of liposomal bupivacaine compared to LIA [45–47]. Furthermore, it is important to consider the cost of liposomal bupivacaine compared to traditional techniques. Wholesale costs for a vial of EXPAREL266 mg/20 mL is $14.25 compared to a 10 mL vial of 0.25 % bupivacaine HCl costing $0.29 [48]. Therefore, current available evidence shows no benefit to the use of liposomal bupivacaine compared to a traditional LIA cocktail for the management of pain following total knee arthroplasty.
In conclusion, from a surgeon’s perspective, local infiltration analgesia is an effective strategy for management of pain following lower limb total joint arthroplasty and can be easily employed by all surgeons without the need for specialized training or equipment. LIA can be easily combined as a part of multimodal postoperative pain management protocols. It should continue to be a component of pain control paradigms for the majority of patients undergoing total joint arthroplasty .
Why Is LIA Popular for Arthroplasties and Can It Be Used for All Joint Surgeries?
Proximal joints of the limbs such as shoulder, hip, and knee have multiple nerves supplying the joints. Upper limb surgeries are effectively covered by brachial plexus blocks since the ensuing motor blockade is not much of a concern for postoperative physiotherapy and rehabilitation.
Proximal lower limb surgeries on the one hand require the patients to actively mobilize after surgery. Ankle and foot surgeries on the other hand does not have the same concerns as that of hip or knee surgeries since they are typically advised not to weight bear for the first couple of days and hence analgesia in these cases can be effectively accomplished with popliteal sciatic nerve block with or without saphenous nerve block. Traditional approaches for hip and knee analgesia have employed neuraxial techniques (intrathecal opioids, epidural analgesia) or peripheral nerve blocks (lumbar plexus or femoral nerve blocks with or without sciatic component) to ensure effective analgesia. The accompanying motor blockade is a cause for concern in lower limb surgeries since they not only interfere with physiotherapy but also may pose a risk for patient falls [49, 50]. Hence, a site-specific modality such as LIA may be suitable for such proximal lower limb surgeries. The popularity of local infiltration analgesia is due to its low cost and ease of administration by the surgeons intraoperatively without the need for regional anesthesia experts to initiate the intervention. LIA being site specific in its action is supposed to lack the motor weakness seen with PNB and thereby may permit early ambulation and physiotherapy.
The following safety concerns need to be considered before LIA:
What concentration and total volume of LA is appropriate for the patient?
Can the joint clear local anesthetic in a reasonable period of time in order to avoid toxicity?
Do we need single injection or continuous catheter?
Is the articular cartilage intact after surgery?
Are there factors influencing the risk of local and systemic toxicity?
All local anesthetics are chondrotoxic and hence should not be injected into an intact joint (see section “Chondrotoxicity ”). Fortunately, the articular surfaces are removed in total joint arthroplasties and hence the chondrotoxic effect is not of much concern in these situations. The LIA is avoided in situations when there is a chance of an intact synovial or joint cartilage remaining, such as arthroscopic surgery, unicompartmental knee replacement, hip resurfacing arthroplasty, hand and foot surgery among others [25, 26].
Anatomical Consideration
It is essential to know the neuro-anatomy of the joint for the success of the LIA technique since not all areas within a joint have the same amount of mechanoreceptors or free nerve endings. Hence, the technique of LIA should target the areas of higher innervation compared to others.
Most of the joints in body follow Hilton’s law with some exceptions [51]. Hilton’s law states that “The same trunks of nerves whose branches supply the groups of muscles moving a joint furnish also a distribution of nerves to the skin over the insertions of the same muscles; and what at this moment more especially merits our attention the interior of the joint receives its nerves from the same source.” The adaptation of this law is that not all the muscles crossing a joint give articular branches but the source of articular innervation and the overlying skin is derived from the same source supplying the agonist and antagonist muscles acting across a joint.
Innervation of the Hip Joint
The main innervators of the hip joint are the femoral nerve via the nerve to rectus femoris, the sciatic nerve via the nerve to the quadratus femoris and branches from the anterior and posterior divisions of the obturator nerve. The skin over the hip joint is supplied by the lateral femoral cutaneous nerve with contributions from the dorso-lumbar nerve (T12-L1) . A majority of the innervation is to the joint capsule compared to the intra-articular structures. The femoral nerve covers the antero-lateral aspect of the hip capsule while the obturator covers the medial aspect of the hip. The sciatic nerve and the superior gluteal nerve together cover the posterior aspect of the hip capsule.
Inside the joint, the acetabulum has the highest amount of sensory innervation followed by the periosteum surrounding the proximal femur. A few studies have recently looked at the distribution of the sensory nerve endings and mechanoreceptors within the hip joint and have consistently found the antero-superior and postero-superior aspect of the acetabular labrum [52] to contain the highest amount of receptors. This is followed by the postero-inferior and the antero-inferior part of the labrum. The rest of the intra-articular components including ligamentum teres have very little contribution to nociception.
Innervation of the Knee Joint
The knee receives innervation from the femoral, sciatic, and obturator nerves through its various branches. Inside the knee joint, several regions have higher neuro-sensory perception compared to others areas [53]. These include (1) The suprapatellar pouch and quadriceps tendon; (2) The medial and lateral retinaculum; (3) The patellar tendon; (4) The medial and lateral collateral ligaments along with the menisci; (5) The tibial attachment of PCL and the femoral attachment of ACL. It is important to cover these areas of increased nociceptive and proprioceptive inputs for the success of LIA.
Equipment and Technique of Injection
The success of LIA like that of any other technique depends on the operator’s performance and variability with infiltration technique is a problem especially with newcomers. Traditionally, a “moving needle” technique has been recommended using a non-cutting small gauge needle (22 Ga) attached to a syringe containing the LIA cocktail and injected in small aliquots of 2–3 ml in different tissue planes. The goal of the technique is to deliver a majority of the drugs into those tissues with increased neuro-sensory perception. A staged fashion of infiltration where the LIA is begun with incision and continued until the closure of the wound is widely adapted. Use of smaller syringes with control for aspiration before injection should be used in areas of potential complications such as in the posterior knee area.
Composition of LIA
Different mixtures have been utilized for infiltration in the studies and include a long-acting local anesthetic such as ropivacaine or bupivacaine; morphine, ketorolac , and epinephrine are added variably. Currently, we do not know definitively as to which component provides the maximum analgesia benefit in the cocktail. The adjuvants added to the local anesthetic can show either an additive or synergestic effect with the local anesthetic. Epinephrine is added to the mixture to delay and minimize the systemic LA absorption but it additionally benefits patients due to its hemostatic effects thereby minimizing wound hematoma and the need for drains. The epinephrine is also known to possess alpha-2 adrenergic agonistic effects which may have a synergistic analgesia effect on local anesthetic. The addition of opioids to the mixture is based on animal and limited human evidence of increased expression of peripheral opioid receptor population at the surgical site [54]. The NSAID’s are added for their local anti-inflammatory properties and analgesia effects. Whether the adjuvant effect is true in humans and whether the same can be achieved using systemic route of administration was studied by Spreng et al. [55]. The patients in their study were randomized to receive either epidural analgesia, LIA with ropivacaine, epinephrine, morphine 5 mg, and ketorolac 30 mg (LIA) or LIA with ropivacaine, epinephrine, and IV morphine and ketorolac (LIA-IV). LIA showed considerably better analgesia and lower opioid consumption compared to epidural or LIA-IV. Although further evidence is needed, like any other multimodal drug strategy, the combination of the drugs in the cocktail seems to work best compared to individual components given by different routes. The optimal dose of each of the components also need to be determined for LIA.
Practical Consideration
LIA in Total Hip Arthroplasty [56]
For both direct anterior and posterior approaches, the LIA begins before the placement of the acetabular cup and the femoral liners are placed. Preferably, the capsular attachment to acetabular labrum is infiltrated with 15–20 ml of LIA cocktail from antero-superior to postero-superior aspect. The femoral periosteum, the posterior capsule and the origin of quadriceps muscles are infiltrated with about 30 ml of cocktail before the placement of the implants. Following the insertion of prosthesis, the anterior capsule and adjacent structures are injected with another 30 ml of LAI cocktail. The remaining 20–30 mL of LAI cocktail is infiltrated into the different layers of closure including rectus femoris, fascia lata, and the wound incision.
LIA in Total Knee Arthroplasty [53, 57]
The exact technique of injection varies from one institution to another but the general principles of injection remain the same. The knee arthroplasty at our institute is performed using the posterior stabilized prosthesis with the para-patellar or vastus sparing incision. The menisci are stripped prior to proximal tibial resection after application of knee retractors. The distal femur and proximal tibia are resected using box cuts which also remove the ACL, MCL, and the PCL. With the retractors in situ, certain surgical areas are infiltrated with LIA cocktail which includes the femoral attachment of ACL, tibial attachment of PCL, remnants of menisci, the medial and lateral collateral ligaments. Several milliliters of the cocktail is also injected into the posterior capsule using a smaller syringe and negative aspiration before injection (Fig. 24.1). After cementing the prosthesis, the LIA cocktail is injected into the quadriceps tendon and while the cement is curing, several milliliters of the PAI cocktail are injected into the anterior capsule, the quadriceps tendon, and the suprapatellar pouch. The knee fat pad in the superior and medial aspect of the knee joint is injected by some surgeons before the closure (Fig. 24.2). The surgical wound and the skin flaps are closed in the usual fashion, and the residual LIA cocktail is injected into the wound at the end. A total of 80–110 mL of the cocktail is used depending on the age, comorbidities, and patient weight.
Other orthopedic surgeries: The evidence of LIA in other orthopedic surgeries is sparse. LIA is currently not popular for shoulder surgeries due to concerns of glenohumeral chondrolysis (see section “Chondrotoxicity ”). A single trial has so far evaluated LIA following spine surgery where continuous infiltration with ropivacaine showed no benefit compared to systemic analgesia alone; [58] Arthroscopic surgeries such as ACL reconstruction [59–63] and hip arthroscopy [64] have utilized periarticular and intra-articular local anesthetic injections with analgesic benefits similar to peripheral nerve blocks but it is our practice to avoid LIA in such situations. LIA for unicompartmental knee joint resurfacing has been a point of debate. While there are studies which have shown analgesic benefit of HV-LIA in unicompartmental knee joint surgeries [65, 66], the presence of an intact synovium and articular cartilage in the majority of the joints after surgery is a cause for concern. Since the surgery is being performed due to the degenerative joint disease, steps to avoid any iatrogenic damage to joint are important for both patient safety and medicolegal reasons. Hence, it is our practice to avoid LIA in any of the above situations when the joint cartilage is intact post surgery .
LIA in Arthroscopy Surgeries
A number of benefits have been reported for LIA including lower pain scores at rest and on movement, lower impact on motor power, reduced incidence of falls, early mobilization, improved early functional scores, and reduced length of hospital stay. The literature looking at the benefits of LIA in comparison to other modalities has been ever increasing in the last decade with some reporting the above benefits while others refuting them. A summary of these findings have been reported in 10 systematic reviews in the last few years which are summarized in Table 24.2. Most of the reviews are consistent regarding the analgesic benefits of LIA since this has been consistently looked into in all the trials evaluating it. When the secondary outcomes such as functional scores, length of stay, range of motion, motor power are looked into, the evidence is inconclusive due to the fewer number of studies reporting these outcomes exclusively.
Table 24.2
Summary of systematic reviews of LIA in hip and knee arthroplasty
Author name (year) | Number of trials included/number of patients | Comparison | Key outcomes |
|---|---|---|---|
Jiang et al. [40] | 21 studies/1769 16 studies on TKA (1447 patients) 5 studies on THA (322 patients) | HV-LIA versus placebo for TKA and THA | • LIA compared to the placebo had less opioid consumption, better function recovery, lower rates of nausea and vomiting for patients with TKA or THA. • THA: Lower VAS scores with rest at 6 and 24 h and lower VAS scores with movement at 6 h compared to placebo. • TKA : lower VAS scores with rest at 6, 24, 48 h, and lower VAS scores with movement at 6 and 24 h compared to placebo. • Length of hospital stay did not show a significant difference between the LIA and placebo groups for patients undergoing TKA and THA. • Range of motion was significantly greater with LIA during the first 72 h postoperatively in comparison to the placebo group. |
Andersen et al. [67] | 27 studies /888 TKA and 756 THA 14 (LIA vs. Placebo) 5 (LIA vs. PNB) 4 (LIA vs. Epidural) 3 (LIA vs ITM) 1 (LIA vs. systemic analgesia) | LIA versus other modalities in both THA and TKA | • THA: No additional analgesic effect of LIA compared with placebo in THA when a multimodal analgesic regimen was administered perioperatively. • THA: Compared with intrathecal morphine and epidural analgesia, LIA was reported to have similar or improved analgesic efficacy. • TKA : most trials reported reduced pain and reduced opioid requirements with LIA compared with a control group treated with placebo/no injection. • TKA : Compared with femoral nerve block, epidural or intrathecal morphine LIA provided similar or improved analgesia in the early postoperative period. • The use of wound catheters for postoperative administration of local anesthetic was not supported in the included trials, and LOS was not related to analgesic efficacy. |
Xu et al. [70] | 18 studies /1858 | Single injection LIA vs Placebo for TKA | • The VAS values at postoperative 2, 4, 6, 12, 24, and 48 h per patient were significantly lower in the LIA group than in the placebo. • LIA also had less morphine consumption and better early functional recovery including range of motion, time to straight leg raise and 90° knee flexion than the latter group. • No significant difference in length of hospital stay or side effects was detected between the two groups. • This review included a wide variety of LIA volumes and concentration. Heterogeneity in reported outcomes and method of LIA. |
Jime’nez-Almonte et al. [68] | 15 (pairwise LIA vs placebo)/1128 patients; 12 (pairwise PNB vs. Placebo)/732 patients 35 RCT’s for network meta-analysis (comparing LIA or PNB with intrathecal opioids or epidural) | Pairwise and network meta-analysis (LIA vs. PNB for THA) | • No differences between peripheral nerve blocks and local infiltration analgesia in terms of postoperative pain scores and cumulative opioid consumption at 24 h after THA • Use of local infiltration analgesia had a greater probability of being ranked most effective for both outcomes. |
Fan et al. [75] | 8 studies/752 | HV-2LIA vs. PNB for TKA (both single injection and continuous catheter studies included) | • On POD 1: The NRS values for pain on rest were lower in LIA than those in PNB. • No significant difference between the two regarding the NRS score with activity. • On postoperative day 1, the morphine consumption on POD 1 was lower in LAI than that in PNB. • Both subgroups showed no significant difference in knee ROM at 3 months postoperatively. • Opioid-related side effects (nausea/vomiting and dizziness) less, while infection and urinary retention were more in LIA. • LOS was less in LIA compared to PNB. |
Sun et al. [71] | 10 studies /735 patients | Continuous HV-LIA versus placebo in TKA | • Continuous infusion analgesia provided better pain control with rest at 24 h only and with mobilization at 24 and 48 h. • Pain scores at rest were comparable at rest at 48 and 72 h and pain scores on movement were comparable at 72 h. • Continuous infusions increased the rate of infection and the rate of nausea or vomiting. • There were no significant differences in the length of hospital stay, deep venous thrombosis, or duration of surgery. |
Mei et al. [74] | 6 studies/306 | HV-LIA vs. FNB for TKA | • Pain scores at rest and narcotic consumption were comparable between LIA and FNB in the first 24 postoperative hours. • Pain scores on movement were better with FNB in the first 24 postoperative hours. |
Albrecht et al. [73] | 14/1122 | LIA vs. PNB for TKA (five trials compared single shot and nine trials compared continuous catheters) | • The primary outcomes of i.v. morphine consumption, pain scores at rest and on movement on postoperative day one (analog scale, 0–10) showed no difference. • No clinical differences in functional outcomes or rates of complications (cardiovascular, neurological, falls, and knee infection). • Range of motion on postoperative day 2, knee society score at 6 weeks and length of stay were statistically different but without direct clinical relevance. |
Yan et al. [69] | 9 Studies/537 | HV-LIA vs. Epidural for THA and TKA | • THA: In the first 24 postoperative hours, resting pain scores were comparable but epidural provided better dynamic pain scores. • THA: At 48–72 postoperative hours, both LIA and epidural provided comparable analgesia both at rest and movement. • TKA : Comparable resting and dynamic pain scores in the first 24 postoperative hours. • TKA : at 48–72 h, LIA provided better analgesia than epidural both at rest and movement. • The range of knee flexion was better with LIA at 24, 48, and 72 postoperative hours (3 studies). • LIA failed to reduce the hospital length of stay (4 studies). |
Hu et al. [72] | 16 studies/1206 | HV-LIA vs. RA (Epidural and FNB) for TKA | • LIA showed significantly lower pain score in the first 24 h at rest. There was a tendency for lower pain scores on movement with PNB but not with EA in comparison to LIA. • No difference in morphine consumption or complication rate between the two groups. • Early functional recovery (Range of motion and Straight leg raise) on POD 1 and 3 weeks was better with LIA group but not at 3 months. • Long-term functional recovery scores were comparable (knee society score). • Length of hospital stay of the LIA group was marginally shorter than that of the RB group. |
Clinical Evidence
Hip Arthroplasty
There have been four systematic reviews evaluating the benefits of LIA in comparison to placebo, epidurals, intrathecal morphine, and peripheral nerve blocks. Compared to placebo [40], LIA has been shown to result in better resting pain scores at 6 and 24 h and better dynamic pain scores at 6 h while it was no better than a placebo beyond 24 h for rest pain and beyond 6 h for dynamic pain. A review by Andersen et al. [67] furthered this evidence by showing that LIA in itself was comparable or superior to epidural, intrathecal, morphine (ITM) or peripheral nerve blocks but was no better than a placebo in the context of background systemic multimodal analgesia treatment regimen. The comparability of LIA with PNB and epidural has been supported by other reviews on the topic [68, 69].
Total Knee Arthroplasty (TKA )
In the last 3 years, nine reviews have looked into the benefit of LIA in TKA . LIA provided longer duration of analgesia following TKA in both rest pain and movement in comparison to the analgesic benefit seen in THA [40, 67, 70]. The LIA provided better analgesia compared to placebo in four reviews [40, 67, 70, 71]. In comparison to epidurals, LIA provided comparable analgesia in the first 24 h and superior analgesia in the 24–48 h period [67, 69, 72]. When LIA was compared to peripheral nerve blocks, the evidence varies regarding the superiority of one technique over the other depending on the review and their included studies. Among the five reviews, Andersen et al. [67] (5 studies) and Albrecht et al. [73](14 studies) noted comparable analgesia both at rest and movement but on the other hand, while noting comparable resting pain scores between the two, Mei et al. [74] (6 studies) and Huet al [72] (16 studies) noted better analgesia with PNB on movement. In contrast, another review by Fan et al. [75] (8 studies) noted better resting pain scores with LIA and comparable pain scores on movement in the first 24 postoperative hours.

Full access? Get Clinical Tree





