Fig. 22.1
Organization of Emergency Department Regional anesthesia Panel A. (1) Acute pain service/anesthesiologist. This is an obvious partner with emergency clinicians. There are few scenarios where the anesthesiology service has the capacity to cover the ED in a timely manner for unforeseen acute injuries at all hours. To realize the goal of a seamless continuum of optimal care, collaboration and partnership is essential. (2) Nursing, pharmacy, and logistical support. Collaborative training and protocol development facilitates efficiency and safety. Important areas for nursing education and training include indications for regional anesthesia, recognition and treatment of local anesthetic toxicity, compartment syndrome evaluation, and postblock care. Crucial pharmacy issues include maintaining availability of various local anesthetic agents, establishment of guidelines for multimodal analgesia, and maintaining lipid rescue capacity [25]. A well-stocked area with appropriate blocks needles and equipment helps promote safety and efficiency. Nursing can be a valuable partner to develop a system quality assurance and follow up. (3) Trauma/general surgeon. Blocks are best used as part of multimodal analgesic bundle. The concept of early use of blocks in the trauma may be new to some surgeons. Development of ED trauma pain protocols that integrate regional anesthesia is helpful [35]. (4) Ultrasound machine. A modern, well-maintained, appropriately cleaned machine with linear and curved array transducers should be readily available for rapid use at the bedside. (5) Patient selection. Blocks should be matched to injury, contraindications excluded, and a collaborative plan for integration of the block into the longitudinal plan of care made before any block is placed. Patient, provider, and machine should be ergonomically positioned with an unobstructed line of site. (6) Documentation. The undifferentiated emergency patient may have numerous consultant exams. Delaying blocks for consultant exams should be avoided by establishing a consensus for preblock extremity and neurologic exam that is sufficient, comprehensive, and clear so that all involved consultants can trust in it. The time of block should be marked on the extremity with marker pen to avoid later confusion in regards to neurologic deficits. Thorough documentation of block details should be available to all participating providers

Fig. 22.2
Organization of Emergency Department Regional anesthesia Panel B. (7) Orthopedist. Close partner in evaluating for compartment syndrome and neurologic injury. Collaborative research, training, journal clubs, and protocols promote effective integration of emergency and orthopedic pain management. (8) Monitoring. Local anesthetic toxicity risk can be lessened with meticulous ultrasound-guided technique, use of the smallest possible quantity, and use of less cardiotoxic agents such as 2-chloroprocaine and lidocaine . Bupivacaine holds the greatest risk of toxicity and should be used only in settings adequately prepared to identify and treat LAST. Continuous cardiopulmonary monitoring is recommended for all bocks. (9) Informed consent. ED nerve blocks are only performed on awake patients able to comprehend the risks and benefits. (10) Preparation for complications. Any ED performing regional blocks should be prepared to rapidly initiate lipid rescue without delay in cases of LAST. Standard resuscitation equipment should be at hand. (11) Emergency physician. Blocks should only be performed by physicians adequately trained to execute the blocks safely. Training pathways begin with simulator and cadaver models and progress to supervised clinical practice, culminating with independent practice and skill maintenance
Fracture Hematoma Blocks
Direct infiltration of the periosteum at the site of an acute bone fracture is referred to as a “hematoma block.” Currently, hematoma blocks are likely the most common form of regional anesthesia for long bone fractures in the emergency department. This technique is most commonly used by orthopedists and emergency clinicians for distal radius fracture analgesia [13, 14]. The hematoma block can be placed by palpation of the fracture site or ultrasound can be used to directly visualize the fracture. Less commonly, hematoma blocks can be applied to a variety of acute fractures including, humerus, clavicle, and femur fractures [15–18].
Overall, several investigations of distal radius fracture hematoma blocks have found good analgesic outcomes without any significant complications, suggesting this is a safe technique [14, 15, 19, 20]. However, the only reported cases of local anesthetic toxicity in the emergency department setting have occurred with hematoma blocks [21–23]. Of note, in both cases, a seizure occurred after injection of subtoxic doses of lidocaine into a distal radius fracture hematoma. The first case involved a 40 kg, 94-year-old woman who received an injection of 10 mL of 2 % lidocaine (200 mg or 5 mg/kg) into the fracture site. She experienced a tonic clonic seizure immediately after injection that lasted for 2 min, resolving spontaneously with no intervention or further complication. The second case, reported by Dezfuli et al. involved a 65 kg 88-year-old woman also with a distal radius fracture who received a hematoma block with a 20 mL mixture of 1 % lidocaine (100 mg) and 0.25 % bupivacaine (25 mg) both without epinephrine [21]. Immediately after injection the patient became unresponsive and was observed to have tonic clonic jerks. The episode lasted for 5 min and resolved spontaneously without intervention or further complication.
There is only limited data on the uptake of local anesthetic after hematoma block into the systemic circulation. Quinton et al. evaluated arterial lidocaine concentrations among nine patients undergoing hematoma blocks for distal radius fracture analgesia with 1 % and 2 % lidocaine [23]. Among the patients blocked with 2 % lidocaine, the mean peak level of arterial lidocaine was 2.6 μg/mL which is similar to serum lidocaine levels after brachial plexus blockade. Patients blocked with 1 % lidocaine had significantly lower mean peak concentration of 0.85 μg/mL. Peak levels occurred 10–15 min after injection. Use of relatively dilute lidocaine (1 %) and avoidance of more potent local anesthetics, such as bupivacaine, may be a practical safety measure for routine practice.
Finally, hematoma blocks do involve entry into a sterile anatomic space and can rarely introduce infection. Bassu et al. reported a case of osteomyelitis following a hematoma block for distal radius fracture reduction despite the use of sterile precautions [24]. Contaminated skin, open fractures, immune compromise may pose additional risks for infection and may not be appropriate for a hematoma block .
Promoting Regional Anesthesia Safety and Efficiency with an Emergency Department Block Cart
A dedicated block cart is a convenient and effective way to create space to organize practical materials related to emergency regional anesthesia, such organization promotes an organized, consistent practice to accepted standards of safety [25] (Fig. 22.3). Block cart contents may include:
Reference materials and textbooks on regional anesthesia.
Phantoms for practicing ultrasound guidance.
Specific, procedure related, protocols, checklist, and guidelines.
Block-specific equipment including:
Materials to ensure sterility such as drapes, gloves, probe covers, sterile gel, skin cleansers.
Block needles of varying lengths.
Extension tubing.
Syringes.
Local anesthetics and intralipid.
Resuscitation equipment .
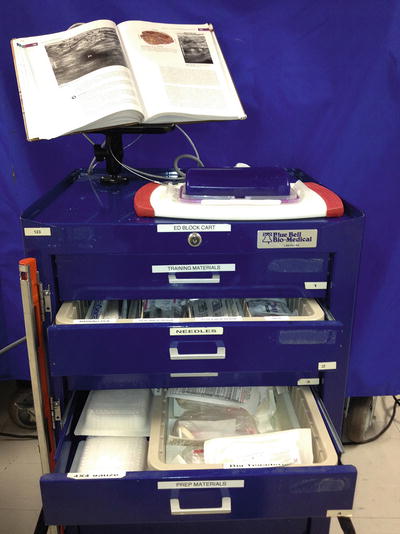
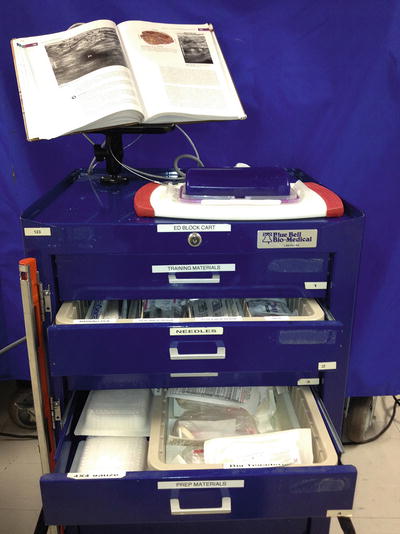
Fig. 22.3
Emergency department block cart. The emergency department block cart can serve multiple functions to promote safety and reduce potential complications. Educational and simulation materials for practice and continuous learning support staff to maintain and advance skills. Convenient location of all the necessary supplies and documentation sheets promotes efficiency and enhances provider adoption of best practices
Emergency Department Regional Anesthesia Documentation
Clear and comprehensive documentation assures that all providers caring for a patient understand what block was done, when it was done, and what type of local anesthetic was used. This understanding will guide appropriate safety precautions to prevent adverse block-related events such as falls from attempting to ambulate with a block or compression necrosis to an insensate arm pressed against the railing of the hospital bed.
Without effective communication and documentation emergency nerve blocks can cause potentially dangerous confusion around possible neurologic injuries. If a clinician renders a limb insensate, but a clinical team member is not aware the block was placed, it can trigger distracting, and potentially harmful confusion. Effective communication and documentation is particularly important for the emergency trauma patient who may have multiple consulting services and an evolving set of injuries. Without proper communication and documentation, the loss of sensory and motor function could be mistakenly considered a new focal neurological deficit triggering evaluation for cord injury or stroke.
Strategies for Emergency Department Communication and Documentation
Verbally communicate with relevant consultants and the admitting clinical team prior to and after block placement so that they are aware of:
The time the block was placed.
The expected sensory and motor deficit.
The medication used and the expected range of block duration.
Block care precautions such as maintaining nonambulatory status or protection of blocked arm with a sling.
Any monitoring concerns for potential compartment syndrome.
Any procedural complications.
Appropriate Local Anesthetic Selection
Appropriate choice of a local anesthetic (Table 22.1) can improve safety and help prevent several complications [26, 27] including
Prolonged block after clinical need for anesthesia has passed.
Premature resolution of the block.
Local anesthetic toxicity.
Table 22.1
Selection of local anesthetics for emergency regional anesthesia
The Ultra-short & ultra-safe procedural block: 3 % 2-Chloroprocaine Maximum dose = 800–1000 mg (20-30 mL of the 3 % solution) |
Comments 3 % 2-Chloroprocaine is used for ultra-short blocks in the 60–90 min range. This is perfect for reductions or procedures where you would like a brief block. As an ester rapidly metabolized in the blood (<60 s half-life), the risk of toxicity is very low. This low toxicity allows safe use of a high concentration (3 %) that likely contributes to the fast onset of the block Use this med when you as the ED provider are in control of your time and the procedure. It really does wash out quickly, which is great if you completed the procedure, not so great if it wears off before you even get started!!! Example : 20 ml 3 % 2-Chloroprocaine interscalene brachial plexus block for shoulder reduction |
Procedural block where 2–3 h of surgical anesthesia is needed: 1.5 % Mepivacaine Maximum dose = 5-6 mg/kg (20 mL 1.5 % solution) |
Comments Intermediate potency amide perfect for when a several hour window of surgical level anesthesia is needed. Fast onset with 2–3 h of dense surgical anesthesia. Consultants can be unexpectedly delayed and it is very, very disappointing to have a block wear off just as the procedure is starting. Mepivacaine gives dense block and a nice window for this scenario. Mepivacaine does not have a strong vasodilatory affect and is typically used without epinephrine Example : 20 mL 1.5 % Mepivacaine infraclavicular brachial plexus block for distal radius fracture reduction and splinting |
The long block, e.g., hip fracture: 0.5 % Ropivacaine Maximum dose = 3 mg/kg (no more than 30 mL 1.0 % solution or 300 mg total) |
Ropivacaine is lipophilic amide structurally similar to bupivacaine. Based on animal studies that suggest that ropivacaine is less arrhythmogenic and resuscitation in case of overdose more successful, ropivacaine is generally considered a safer alternative to bupivacaine. It remains a powerful local anesthetic that should be used with caution. Clinicians using ropivacaine should know how to recognize and treat LAST and intralipid should be at hand Example : 40 ml of 0.5 % ropivacaine for hip fracture analgesia |
Notably, concern for ischemic complications in distal extremities due to epinephrine-containing local anesthetics has been debunked (Textbox 1).
Textbox 1: Myth Debunked: Lidocaine with Epinephrine is Safe for Anesthesia of Fingers, Nose, Penis, and Toes.
It was once a common teaching that avoiding the use of lidocaine with epinephrine for anesthetizing the distal appendages—fingers, nose, penis, and toes—should be avoided due to risk of ischemic necrosis. This concern dates back to reported cases of gangrene following the use of anesthetic with epinephrine from the late 1900s. Subsequently, several large studies have established the safety of local anesthesia with epinephrine for distal extremities and the penis.
Avoiding a Prolonged Block
Many emergency procedures require a brief period of surgical anesthesia. Using a long-acting local anesthetic such as bupivacaine, will needlessly expose the patient to the risks associated with an insensate extremity, as well as delay identification of any procedure-related nerve injury. For brief painful procedures without need for prolonged analgesia such as a shoulder dislocation reduction, a short-acting local anesthetic such as 2-chloroprocaine is ideal [11].
Avoiding a Premature Resolution of the Block
In the emergency department, procedures may be performed by consultants who may arrive at the bedside to perform the needed procedure according to an unpredictable timeline as they juggle various clinical duties. Placement of a block that then wears off too early is obviously not desired as it exposes the patient to the risks of the nerve block without benefit. In this scenario, such as a large abscess in need of surgical drainage, an intermediate-acting local anesthetic with a 2–3 h window of anesthesia, like 2 % lidocaine or 1.5 % mepivacaine, is ideal [27].

Full access? Get Clinical Tree





