CHAPTER 116
Lateral Epicondylitis and Medial Epicondylitis
(Tennis Elbow, Golfer’s Elbow)
Presentation
In lateral epicondylitis, the patient complains of pain in the lateral elbow that frequently radiates down the lateral aspect of the forearm. Because the lateral epicondyle is the bony origin of wrist extensors, patients are usually involved in an activity that requires repetitive wrist extension, such as tennis or mechanical work. Occasionally, the patient can recall a specific injury to the area, but more often the pain is of gradual, insidious onset. Most patients relate symptoms to activities that stress the wrist extensor and supinator muscles, and especially to activities that involve forceful gripping or lifting of heavy objects. Even holding lightweight objects such as a cup may be difficult. There is tenderness to palpation over the origin of the extensor carpi radialis brevis tendon immediately anterior, medial, and distal to the lateral epicondyle. This tenderness is more pronounced with resisted wrist extension while the elbow is in extension or when the forearm is pronated.
Patients with medial epicondylitis complain of pain over the medial epicondyle and the proximal forearm. The pain may radiate down the medial aspect of the forearm. Medial epicondylitis has been associated with activities involving repetitive forearm pronation and wrist flexion, again related to this being the insertion point for wrist flexors. It occurs frequently in baseball pitchers and is also related to golf, tennis, bowling, racquetball, archery, weightlifting, and javelin throwing. It is also associated with occupations such as carpentry, plumbing, and meat cutting. Onset is usually insidious, but there may be an inciting event. The patient may also complain of a weak grasp and pain with repetitive wrist flexion and pronation. There will be tenderness to palpation just anterior to the medial epicondyle at the origin of the pronator teres and flexor carpi radialis muscles. Resisted wrist flexion and forearm pronation while the patient’s elbow is in extension will reproduce symptoms.
What To Do:
 Obtain a careful history that includes inquiry into activities that may be causing overuse injury to the elbow. Also ascertain information about the patient’s general health that may reveal an alternate source of tendinopathy, such as psoriasis, a sexually transmitted disease, gout, or the use of a fluoroquinolone within the past 3 months.
Obtain a careful history that includes inquiry into activities that may be causing overuse injury to the elbow. Also ascertain information about the patient’s general health that may reveal an alternate source of tendinopathy, such as psoriasis, a sexually transmitted disease, gout, or the use of a fluoroquinolone within the past 3 months.
 Physical examination should concentrate on localizing the precise site of musculotendinous tenderness but should also include neck examination to help rule out cervical disease.
Physical examination should concentrate on localizing the precise site of musculotendinous tenderness but should also include neck examination to help rule out cervical disease.
 Initial treatment begins with the immediate, temporary cessation of offending activities. Complete immobilization or inactivity is not recommended. The affected elbow is iced or ice massaged for 5 to 15 minutes, two to four times per day, for its local vasoconstrictive and analgesic effects.
Initial treatment begins with the immediate, temporary cessation of offending activities. Complete immobilization or inactivity is not recommended. The affected elbow is iced or ice massaged for 5 to 15 minutes, two to four times per day, for its local vasoconstrictive and analgesic effects.
 Prescribe a nonsteroidal anti-inflammatory drug (NSAID) if it is not contraindicated by allergy, bleeding, gastritis, or renal insufficiency. One recent trial suggests that a 7-day treatment course with a once-daily, 100-mg ketoprofen topical patch can provide pain relief without the adverse events associated with systemic delivery of an NSAID (at a much higher cost to the patient). Always advise patients to take NSAIDS with food and plenty of clear fluids to help alleviate stomach discomfort and to protect kidney function. Prescribing a histamine blocker or proton pump inhibitor can also be helpful.
Prescribe a nonsteroidal anti-inflammatory drug (NSAID) if it is not contraindicated by allergy, bleeding, gastritis, or renal insufficiency. One recent trial suggests that a 7-day treatment course with a once-daily, 100-mg ketoprofen topical patch can provide pain relief without the adverse events associated with systemic delivery of an NSAID (at a much higher cost to the patient). Always advise patients to take NSAIDS with food and plenty of clear fluids to help alleviate stomach discomfort and to protect kidney function. Prescribing a histamine blocker or proton pump inhibitor can also be helpful.
 When comfort allows, deep friction massage, muscle stretching, and grip strengthening may help with early rehabilitation.
When comfort allows, deep friction massage, muscle stretching, and grip strengthening may help with early rehabilitation.
 If the patient does not respond to these measures, consider injecting the area with bupivacaine and a steroid. Conflicting data have been published regarding the efficacy of such corticosteroid injections, and although there is likely to be significant pain reduction at 6 weeks after the injection, there appears to be no difference from preinjection pain and pain at 3 months and 1 year. When this modality is elected, you can inject bupivacaine 0.5% (Marcaine), 3 mL, and methylprednisolone (Depo-Medrol), 10 to 20 mg, using a 1¼-inch, 25-gauge needle. Forewarn patients of a possible flare-up of pain when the local anesthetic wears off, which may last for 24 to 48 hours.
If the patient does not respond to these measures, consider injecting the area with bupivacaine and a steroid. Conflicting data have been published regarding the efficacy of such corticosteroid injections, and although there is likely to be significant pain reduction at 6 weeks after the injection, there appears to be no difference from preinjection pain and pain at 3 months and 1 year. When this modality is elected, you can inject bupivacaine 0.5% (Marcaine), 3 mL, and methylprednisolone (Depo-Medrol), 10 to 20 mg, using a 1¼-inch, 25-gauge needle. Forewarn patients of a possible flare-up of pain when the local anesthetic wears off, which may last for 24 to 48 hours.
 The counterforce brace has been found to be helpful and is thought to reduce the load at the lateral or medial epicondyle by preventing the forearm muscles from fully expanding. Braces placed just distal to the epicondyles reduce loads greater than pads placed over the epicondyles (Figure 116-1, A and B).
The counterforce brace has been found to be helpful and is thought to reduce the load at the lateral or medial epicondyle by preventing the forearm muscles from fully expanding. Braces placed just distal to the epicondyles reduce loads greater than pads placed over the epicondyles (Figure 116-1, A and B).
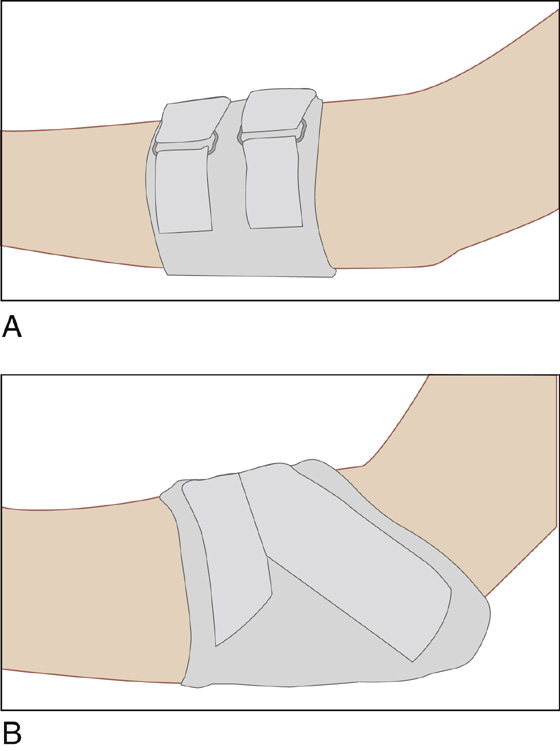
Figure 116-1 A, Lateral elbow brace. B, Medial elbow brace.
 Patients should be informed that recovery often takes several months but that most patients treated with conservative therapy respond successfully without recurrent symptoms. Physical therapy may be considered, but keep in mind that there are no published data proving its efficacy.
Patients should be informed that recovery often takes several months but that most patients treated with conservative therapy respond successfully without recurrent symptoms. Physical therapy may be considered, but keep in mind that there are no published data proving its efficacy.
What Not To Do:
 Do not order radiographs for a classic presentation. Reserve them for questions of bony disease.
Do not order radiographs for a classic presentation. Reserve them for questions of bony disease.
 Do not inject corticosteroids repeatedly into the tendon. They cause it to weaken or possibly rupture.
Do not inject corticosteroids repeatedly into the tendon. They cause it to weaken or possibly rupture.
Discussion
The characteristics most likely to result in elbow tendon overuse are age older than 35 years, high activity level (sports or occupational), and demanding activity technique. Medial epicondylitis, commonly referred to as “golfer’s elbow,” occurs much less frequently than lateral epicondylitis, which is diagnosed 7 to 10 times more often.
Although the precise universal pathophysiology of epicondylitis has yet to be established, it is now generally accepted that the injury results from microtearing of the tendon origin at the epicondyle. This progresses to a failed reparative response and subsequent tendon degeneration that ultimately alters the typical musculotendinous biomechanics of the elbow. Because of its relationship to other overuse tendinopathies (see Chapter 132), the more appropriate descriptive terms for lateral and medial epicondylitis are lateral elbow tendinosis and medial elbow tendinosis.
Both tennis elbow and golfer’s elbow usually affect patients who are between 30 and 60 years of age, with a peak incidence in the 40s. An acute onset of symptoms occurs more often in young athletes, and chronic, recalcitrant symptoms typically occur in older patients.
Poor form for the backhand stroke, extending the wrist when striking the ball instead of holding the wrist and elbow immobile, and swinging from the shoulder increase one’s risk for lateral elbow tendinosis. There is some evidence to support that a two-handed backstroke may decrease risk because of improved stroke mechanics. Patients with medial elbow tendinosis who regularly play tennis often exhibit an improper serve and forehand stroke.
Equipment that is properly sized to the athlete is essential, especially in racquet sports, to prevent subsequent bouts of epicondylitis. Correct grip size is calculated by measuring from the proximal palm crease to the tip of the ring finger along its radial border (Figure 116-2). Lighter graphite frames, racquets less tightly strung (manufacturer’s low-range recommendations), racquets with higher string counts per unit area, and a larger racquet head (90 to 100 square inches of hitting zone) will help to minimize injurious vibration and help prevent stressful off-center contact. In golf, clubs of proper weight, length, and grip are similarly important and can significantly reduce the injurious forces generated within the elbow.
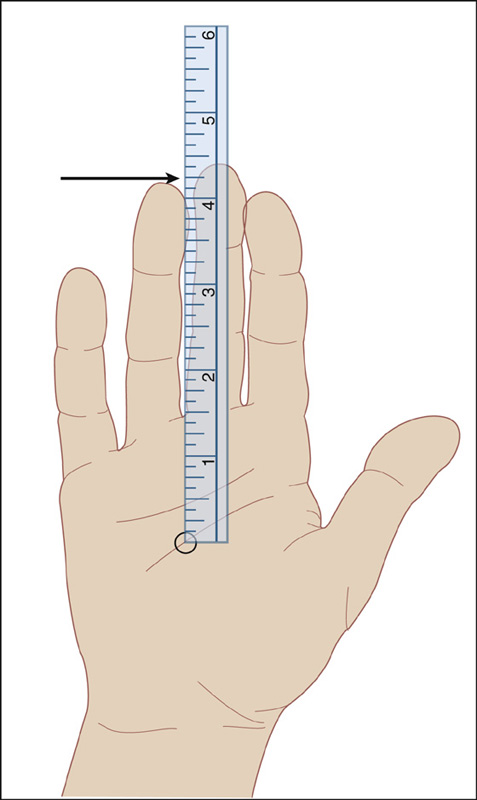
Figure 116-2 Hand-size measurement to determine proper grip handle size—Nirschl technique. (Adapted from Nirschl RP: Elbow tendinosis/tennis elbow. Clin Sports Med 11:851-870, 1992.)
Continued conditioning of the entire body along with the affected extremity is vital to a patient’s successful recovery. Conditioning, including flexibility, strength, and endurance, is best performed with a slow, structured interval program.

Full access? Get Clinical Tree



