Fig. 7.1
Setup of the operating table and the positioning of the patient
The surgeon should be able to move to either side or between the legs as necessary or preferred.
The table should allow inclination or tilting as necessary.
7.1.3 Monitor and Screen Position
Optimal ergonomics call for:
A flat screen placed at 15° below eye level (or at the gaze-down level, i.e., at the level of the surgeon’s elbows).
The monitor placed so that the surgeon’s vision, hands, target, and screen are aligned.
Either several monitors or the video monitors should be mobile and moved according to the site of the pathology to maintain the [ideal] alignment necessary for optimal ergonomic conditions.
7.1.4 Trocar Setup, Creation of Pneumoperitoneum, and Instrumentation
Trocar setup:
Initial trocar layout depends on clinical findings and diagnostic probabilities:
Triangulation is recommended to allow resection and adequate suturing as necessary.
Lateralization of trocar insertion is recommended in case of intestinal distension (intestinal obstruction or ileus secondary to peritonitis or abscess).
Avoid insertion through previous scars (incisions or drainage sites) for the first trocar.
Add additional trocars as needed.
Should allow full and unrestricted exploration of the entire abdominal cavity as necessary
First trocar insertion:
Routine open approach is strongly recommended (without use of the Veress needle), especially when there is considerable intestinal distension.
The periumbilical approach is recommended in case of diagnostic doubt, unless prior surgery indicates otherwise.
Further trocars can be inserted once a preliminary survey of the entire abdominal cavity has shown that there is no need to abort or to convert to a laparotomy.
Two trocars are placed on the right and left and lateral to the rectus muscle sheath at the level of the umbilicus (Fig. 7.2).
Fig. 7.2
Trocar positions for diagnostic laparoscopy
Pneumoperitoneum
Should be established progressively, under close monitoring:
Insufflation should be stopped immediately in case of any drop in blood pressure, unexplained tachycardia, or rise in respiratory pressure.
If the patient stabilizes, laparoscopy can be resumed but with extreme caution (reduced abdominal pressure and close monitoring).
Instruments
30° scopes are recommended:
The 10 mm scope offers better lighting and view.
The 5 and 3 mm laparoscopes offer less trauma but reduced lighting and view.
Essential instrumentation includes:
3, 5, 10, and 12 mm ports
Atraumatic grasping forceps and clamps
Right-angle forceps
Titanium and absorbable clips
At least two needle holders
Energy-driven devices for hemostasis and cutting according to availability and surgeon preference
Scissors
Adequate suction-irrigation device
Suture material and endoloops
Umbilical or vascular tapes
Rubber drains, tourniquets, clamps and bulldog clamps, and bowel and vascular clamps
Plastic bags for the extraction of the operative specimen as required
7.2 Exploration of the Abdominal Cavity
Hemostasis
Active bleeding in unstable patients requires open surgery.
Otherwise, in stable patients:
Small vessels can be closed with clips or with 3/0 monofilament sutures or with modern coagulation devices (ultrasonic devices or Ligasure™).
Large wound surfaces and lacerations of solid organs can be sealed quickly and effectively with autologous fibrin adhesive (Tisseal®, Baxter) and tamponed in combination with a fleece (Hemopatch®, Baxter).
More active bleeding can temporarily be stopped by applying pressure followed by FloSeal® for permanent hemostasis.
7.3 Indications
The wide range of disease that may be diagnosed and treated by emergency laparoscopy includes acute cholecystitis, perforated duodenal ulcer, appendicitis and other causes of acute right lower quadrant pain including adnexal disease, complicated diverticular disease, intestinal obstruction including intussusception, incarcerated or strangulated inguinal or incisional hernia, peritonitis of all origins, iatrogenic perforations, suspicion of mesenteric ischemia, as well as certain postoperative complications.
If the diagnosis is not recognized beforehand, the surgeon should note the area of maximal inflammation, concentration of pus, or blood, as in the case of ruptured ectopic pregnancy.
7.3.1 Acute Cholecystitis
Acute cholecystitis requires cholecystectomy.
Cholecystectomy for acute cholecystitis can be challenging because of:
Inflammation (difficult dissection) of the gallbladder
Increased bleeding
Fragility (perforation is possible)
Adhesion to adjacent organs
Altered anatomy
Timing of operation
Although still debated, most authors agree that early (within 7 days of onset of signs) cholecystectomy appears to be safe and shortens the total hospital stay. In fact, as long as the patient is in good general health and there is no major anesthesia problem, early cholecystectomy can be performed within 48 h from onset.
Delaying cholecystectomy results in significantly higher conversion rates, surgical postoperative complications reoperation rates, and significantly longer postoperative hospital stay, without any advantages.
Of note, the main biliary ducts are at increased risk in acute cholecystitis, and this warrants particular attention.
As the critical view of safety (Fig. 7.3) is more difficult and the demarcation of Rouvière’s sulcus is present in only 70 % of patients, anterograde dissection, intraoperative cholangiograms (Fig. 7.4), and/or the use of indocyanine green is strongly recommended to landmark and delineate the biliary tree. Indocyanine green cholangiography has the advantage of delineation before any dissection takes place.
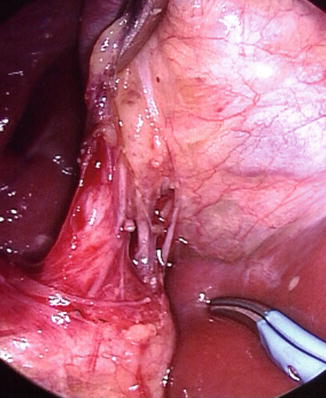
Fig. 7.3
Intraoperative view during laparoscopic cholecystectomy showing critical view of safety with cystic duct and artery at Calot’s triangle

Fig. 7.4
Intraoperative cholangiogram showing the anatomy and (unexpected) common bile duct stones
Ideal treatment is based on the acute cholecystitis Tokyo consensus guidelines:
Grade I (mild acute cholecystitis, with no organ dysfunction and limited disease
Grade II (moderate acute cholecystitis: extensive inflammation but no organ dysfunction)
Grade III (severe acute cholecystitis including gangrenous cholecystitis or empyema with organ dysfunction).
Both grades I and II (mild and moderate) cholecystitis can ideally be treated by laparoscopic cholecystectomy. In case of intraoperative difficulties subtotal cholecystectomy can be performed (although there are no proven advantages).
Both grades II and III (moderate and severe) in high-risk patients can be treated by transhepatic drainage (cholecystostomy).
7.3.2 Perforated Gastroduodenal Ulcer
Laparoscopic repair is feasible and should result in less postoperative pain and surgical site morbidity.
The treatment of choice is simple closure of the perforation (Fig. 7.5) and adequate medical treatment of Helicobacter pylori.

Fig. 7.5
Closure of a perforated acute post-pyloric peptic ulcer with two stitches
Sutures, glue, and/or omentum, sometimes associated.
A hybrid procedure consists of drawing the omentum through the perforation by means of an endolumenal endoscope.
Open repair might be better when:
Patients are hemodynamically unstable.
Patients are at risk for pneumoperitoneum.
Patients have already undergone previous upper GI surgery needing extensive adhesiolysis.
More extensive time-consuming operations are necessary.
Patients are at high risk (two or more Boey risk factors).
Chronic ulcer with a diameter of more than 20 mm is present.
7.3.3 Acute Appendicitis and Acute Pelvic Problems in the Female
Laparoscopic appendectomy (vs. open):
Can be advantageous in the obese and the elderly.
Can be performed in the pregnant women, but care is warranted to adjust trocar insertion to uterine height.
Stump closure is no longer a matter of debate: recent studies have reversed the purported advantages of staplers used routinely, and these should be reserved for patients when loop closure seems difficult or inappropriate (stump necrosis) or there is need for rapid closure. Higher costs for the staplers, however, must be considered, and loop-closure is often chosen instead
Adnexal torsion and ruptured ectopic pregnancy:
Ideal settings for emergency laparoscopic surgery.
Patient must be hemodynamically stable.
Requires specific equipment (vacuum, special suction probe) for tubal preservation.
7.3.4 Complicated Diverticular Disease
Hinchey stages I and IIa can be treated medically, sometimes combined with percutaneous drainage.
Patients with persistent septic signs after drainage and in those with Hinchey IIb, Hinchey III and IV require surgical treatment.
Laparoscopic treatment has been shown to be safe and as effective as open treatment for Hinchey IIb and III.
Source control consisting of resection of the perforated colon segment, with or without immediate anastomosis, is still the standard treatment and can be performed laparoscopically.
However, some surgeons advocate simple laparoscopic lavage, associated or not with suture and/or drainage, the goal being to avoid a major bowel resection and potentially a stoma:
Quantity: four liters of saline followed by drainage plus antibiotic therapy.
Decreases mortality and morbidity (particularly surgical site complications).
Suture or fibrin glue closure of the perforation (if obvious) can be attempted, sometimes reinforced with an omental patch.
Usually no further surgery is required.

Full access? Get Clinical Tree







