Know What the Basic Statistical Terms Mean
Peter F. Cronholm MD
Joseph B. Straton MD
How Clinicians Make Decisions
To make informed, evidence-based decisions, providers need to have an understanding of several statistical concepts. The decision-making process begins by assessing information by means of a history and physical examination framed within an understanding of the relative probabilities of disease states. The next step is to determine the likelihood that the patient has the disease in question. If we have enough information at that time, no further testing is needed, and we may move on to treatment. If not, more information is needed, and further testing must be done to better determine whether the disease in question is in fact the underlying etiology. For each step of the decision-making process, we need to understand testing and disease characteristics.
Clinical decision making is based on an understanding of the incidence and prevalence of diseases considered in differential diagnoses for the types of patients considered. The prevalence of a disease tells us how many people at a given point or period of time have the disease in question. Prevalence combines people who already have the disease and those that will acquire the disease during that period of time. The incidence of a disease tells us how many new cases of a disease develop or are likely to develop over a period of time. Incidence is a measure of risk, whereas prevalence is more of a measure of the burden of disease for a given population. The process of developing a differential diagnosis is a ranking of etiologies based on our understanding of the incidence and prevalence of diseases for a given set of historical and physical data.
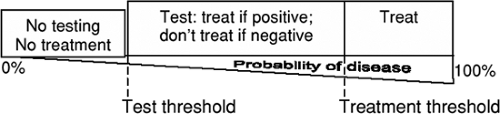
Decisions are made based on the likelihood of a disease for a given clinical situation. The likelihood of a disease ranges from nil (0%) to absolute (100%). There exists a range of likelihoods that vary depending on the balance of costs and benefits of provider decisions that determine what our next steps should be in terms of making choices to treat, not to treat, or to conduct diagnostic testing. Diagnostic testing should be considered when there is a difference between the likelihood that a patient has the disease and the threshold at which a provider chooses to move forward with treatment options. Two thresholds must
be considered that determine the range over which diagnostic testing should be considered. The first is the “testing threshold,” which is the likelihood below which a provider would consider the disease sufficiently rare a cause that he or she would not empirically treat for the disorder nor test for the presence of the condition. To make treatment decisions, providers need to have some point at which they will decide to treat a patient, given the weight of the evidence with no further testing. This point is referred to as the “treatment threshold” (Fig. 312.1).
be considered that determine the range over which diagnostic testing should be considered. The first is the “testing threshold,” which is the likelihood below which a provider would consider the disease sufficiently rare a cause that he or she would not empirically treat for the disorder nor test for the presence of the condition. To make treatment decisions, providers need to have some point at which they will decide to treat a patient, given the weight of the evidence with no further testing. This point is referred to as the “treatment threshold” (Fig. 312.1).
Shaping a differential diagnosis is a process of categorizing the probabilities of various diseases associated with the patient history and exam. The probability that a patient has the disease before any diagnostic testing is done is known as the “prior probability” of disease. Diagnostic testing increases or decreases the likelihood that a person has the disease in question. The likelihood that person has the disease after diagnostic testing is known as the “posterior probability.” Diagnostic testing occurs along a continuum of likelihoods when the prior probability is lower than the treatment threshold but higher than the testing threshold (Fig. 312.1). If the prior probability is above the treatment threshold, one treats the patient without further testing. If the prior probability is below the treatment threshold, further testing is required, the results of which either move one away from the treatment threshold if they are negative or closer or over the treatment threshold if they are positive. A series of tests may be necessary to move the posterior probability that a patient has the disease to the point of treatment. As an illustration, if one operates on a person only if one is 70% sure that he or she has the disease, but after the history and physical one is only 40% sure, then one needs to do more testing to move the likelihood above 70%. There is no need to perform tests when one is already over the treatment threshold (although these are often done for “academic” reasons) or if the test will not provide enough evidence to move one over the treatment threshold if no other testing is linked or available. For example, if a febrile patient has tender anterior cervical anterior cervical adenopathy with an exudative pharynx and the
absence of cough by history, he or she should be treated for bacterial pharyngitis without further testing.
absence of cough by history, he or she should be treated for bacterial pharyngitis without further testing.

Full access? Get Clinical Tree