Melissa C. Davis, Camilo E. Fadul
Intracranial Tumors
Primary malignant and nonmalignant intracranial tumors represent a small fraction of all types of cancer, but they have a major physical, psychological, and financial impact on individual patients, families, and communities. Brain metastases from systemic neoplasm are equally devastating and significantly more frequent. Expedient diagnosis and treatment of brain tumors are essential to minimize potential complications and to maximize functional quality of life. As the first point of contact for patients when acute or subtle changes in health occur, primary care practitioners play an important role in the diagnosis and ongoing care of patients with brain tumors. The practitioner’s knowledge of a patient allows the detection of subtle clinical changes, affording appropriate evaluation and timely diagnosis. Ongoing supportive care during treatment and follow-up of a patient with the diagnosis of a brain tumor is imperative and can be well managed by the primary care practitioner in collaboration with the specialist.
Definition and Epidemiology
The term brain tumor is defined as the growth of abnormal cells in the tissue of the brain. This includes neoplasms that arise from intracranial structures, such as the meninges, which are not a component of the nervous system. Brain tumors can be nonmalignant or malignant, and can be primary or metastatic. Tumor nomenclature and grading are based on the histologic characteristics of the tissue. Whereas primary brain tumors arise from structures of the nervous system, brain metastases are thought to arise from the hematogenous spread of circulating tumor cells that migrate into the perivascular space after disruption of the basal membrane. For primary brain tumors, the World Health Organization (WHO) grading system provides a means to prognosticate the biologic behavior of the tumor. It is based on the tumor’s proliferative potential, nuclear atypia, mitotic activity, and presence of necrosis (Table 203-1). Although prognosis correlates with WHO grade, immunohistochemistry and genetic profiling provide additional information that allows for more accurate brain tumor characterization. The combination of histology and genetic characteristics guide individualized treatment.
TABLE 203-1
Classification of Central Nervous System Tumors
| Tumor Type (Frequency)3 | WHO Grade* |
| Astrocytoma (21.9%) | |
| Oligodendroglioma (1.7%) | |
| Mixed oligoastrocytoma (0.9%) | |
| Ependymoma (1.9%) | |
| Meningioma (35.8%) |
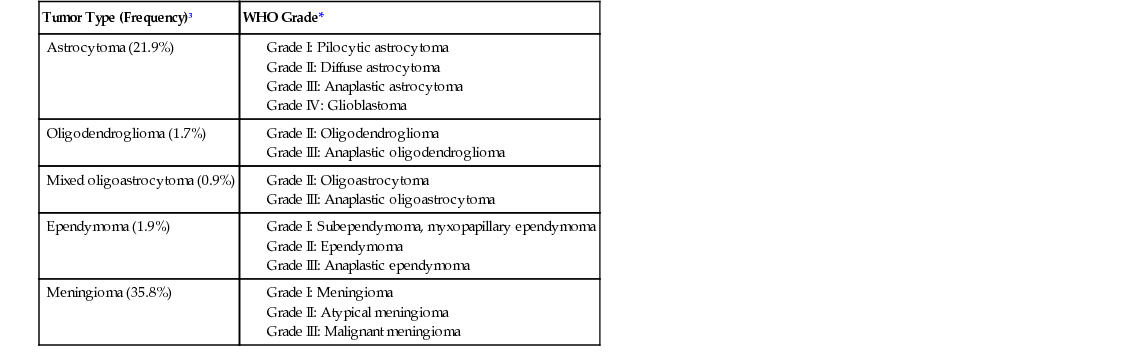
Tumors with glial characteristics, called gliomas, are the most frequent type of primary malignant brain tumor. Based on the cell of origin, gliomas are further classified into astrocytomas, oligodendrogliomas, mixed oligoastrocytomas, and ependymomas.1 The hallmarks of high-grade malignant gliomas (anaplastic gliomas and glioblastoma) are neovascularization, high mitotic rate, infiltration into surrounding tissue, and presence of necrosis.
The cause of primary brain tumors is unknown. Previous cranial irradiation has been associated with the development of meningiomas. The incidence of meningioma also seems to be higher in women with a history of breast cancer, probably related to the expression of hormone receptors by these tumors. There are familial cancer syndromes that have a high incidence of brain tumors. For example, the Li-Fraumeni syndrome, caused by the mutation of the tumor suppressor gene p53, is associated with a high incidence of brain tumors. Primary central nervous system (CNS) lymphoma occurs more frequently in patients who are immunosuppressed after transplantation or in patients with acquired immunodeficiency syndrome (AIDS) in association with Epstein-Barr virus infection. In patients who are not immunocompromised, the cause is uncertain.
In 2014, primary nervous system tumors will account for approximately 1.4% of all new cancer diagnoses.2 In the United States, the estimated incidence of malignant and nonmalignant brain tumors is 21.03 cases per 100,000 person-years, with approximately 66,240 new cases per year. Meningioma, usually a nonmalignant brain tumor, accounts for 35.8% of all cases, followed by glioblastoma, a malignant brain tumor, which accounts for 15.6% of cases.3 Survival rates vary significantly based on histology and grade. The 5-year relative survival rate for a grade I meningioma is 82%.4 Conversely, the 5-year relative survival rate for glioblastoma (grade IV glioma) is less than 5%.3
The incidence of brain metastases varies significantly based on primary malignancy. Although melanoma and small cell lung cancer (SCLC) have the highest predilection to metastasize to the brain, the prevalence of brain metastases is higher from non-SCLC and breast cancer, given the frequency of these malignancies. It is expected that the incidence will increase as imaging techniques become more accessible, particularly brain magnetic resonance imaging (MRI). The incidence of brain metastases is also expected to increase as systemic therapy, which often does not cross the blood-brain barrier, improves survival.5 Prognosis is influenced by primary malignancy, age, performance status, and number of brain metastases. Median survival after diagnosis of brain metastases ranges from 4.9 months for SCLC to 13.8 months for breast cancer.6 The prognosis has improved in recent years, and the number of long-term survivors is increasing.
Clinical Presentation
Brain tumors cause symptoms by infiltrating, expanding, and displacing healthy brain tissue. In addition to the infiltration of normal tissue, brain tumors can increase the permeability of blood vessels, leading to edema that dislodges and compresses normal structures. As the brain tumor volume and resulting edema move normal structures, patients can sustain ischemic strokes from blood vessel occlusion and herniation from displacement of brainstem structures. In addition, tumors can cause injury to normal neurons, resulting in increased excitability of the neurons and seizures. Tumors involving the hypothalamic-pituitary axis can cause a variety of endocrinologic syndromes.
A meticulously taken history and thorough examination are essential to the diagnosis of a brain tumor. The growth pattern and location will determine the symptoms. Fast-growing tumors such as glioblastoma tend to produce subacute symptoms, whereas slow-growing tumors such as meningiomas can become very large before producing symptoms. The clinical presentation of brain metastases is usually more abrupt, related to rapid tumor growth and associated edema. On occasion, brain tumors can have an acute presentation as the result of intratumoral bleeding or a seizure. In children, tumors are usually in the posterior fossa and most frequently manifest with signs of increased intracranial pressure.
There are three neurologic syndromes (combination of symptoms and signs) caused by an intracranial neoplasm, categorized as nonfocal, localizing (focal), and seizures. These syndromes vary according to tumor location, size, and growth rate. Nonfocal syndromes may include symptoms caused by increased intracranial pressure and brain herniation, personality changes, gait disorder, and endocrine dysfunction. Localizing symptoms are usually focal and specific to the area of the brain involved, and may include motor, sensory, language, or visual impairments. Approximately 30% of patients will experience a seizure at some point during the course of the illness. Seizures can be focal or generalized. Focal seizures involve one hemisphere of the brain and typically manifest as sensory or motor symptoms. Generalized seizures occur when there is abnormal electrical activity in both cerebral hemispheres7 (see Chapter 201).
Physical Examination
The examination needs to be thorough, albeit focused on eliciting findings that provide the best diagnostic yield. A mini-mental examination should be included, given that alteration in mental status is frequently observed in nonfocal syndromes. Examination of the optic fundi is also crucial because papilledema may be the only finding to indicate increased intracranial pressure.
Components of the neurologic physical examination allow for localization to a particular brain region. Visual field testing by confrontation can localize involvement of the optic nerve pathway, as well as the occipital or parietotemporal lobes. Abnormalities of ocular movement can occur from compression of the oculomotor nerves or involvement of the brainstem. Motor and sensory abnormalities correlate with frontal or parietal involvement. Aphasia can be seen with damage to the dominant frontal or temporal lobes. Of note, focal speech disorders can be erroneously diagnosed as confusion (nonfocal). Gait, tone, and coordination examinations are fundamental for posterior fossa brain tumors. Examples of the signs most frequently elicited on presentation of intracranial tumors are included in Table 203-2. In the case of seizures, patients may initially have focal findings on examination that disappear once the patient has recovered from the postictal state.
TABLE 203-2
Physical Findings
| Syndrome | Symptom or Sign | |
| Nonfocal | Increased ICP: headache, confusion, papilledema, vomiting Herniation: cingulate, tentorial, tonsillar, CN III, CN VI Personality changes: dementia, anger, passivity, memory 
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|



